Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
News 5/1/20
Top News

Health data and software company Arcadia acquires assets of the Massachusetts EHealth Collaborative, including technology and customer accounts.
MAeHC President and CEO Micky Tripathi, MPP, PhD will join Arcadia as chief alliance officer while continuing his roles with Argonaut, Sequoia, CommonWell, HL7, HL7 FHIR Foundation, and CARIN Alliance.
Reader Comments

From VCU Observer: “Re: VCU Health’s rip-and-replace of Cerner with Epic on May 1. At least one board member says the project hasn’t been approved nor the implementation costs outlined. The expenditure, rumored to be hundreds of millions of dollars more than Cerner’s upgrade bid, doesn’t make sense at this time.” Unverified. VCU announced a mid-2021 go-live when they chose Epic in December, which seems challenging given limits on travel and in-hospital presence for the all-important initial planning and on-the-ground design meetings.
From PPP Shooter: “Re: paycheck protection plan loans. The Small Business Administration has clarified that publicly traded companies, as well as the portfolio companies of private equity funds, are prohibited from receiving PPP loans and must pay them back by May 7 if they received them. Hundreds of publicly traded companies received these loans and the PE firm clarification may cause problems for the health IT world.” SEC filings indicate that 220 public companies need to return $870 million that they received before the rule was changed, with more that are likely still be disclosed since SBA has refused to release a list of the companies that received money. Publicly traded health IT company Castlight Health received the maximum loan of $10 million, but says it will return it.
From Pickle Bickering: “Re: contract tracing by smartphone app. Is it worth the privacy intrusion?” Apple and Google are doing exactly what big tech companies always do when barging into healthcare with minimal knowledge — they are thinking that a cool app can fix everything. App-based contact tracing is doomed to fail, in my opinion, and not just because of privacy issues:
- Not all Americans own smart phones and carry them at all times. Children, for example, appear to be significant spreaders and will become more so when schools and daycares reopen, but few of them will be carrying a contact-tracing app on a phone.
- Many people won’t use tracking apps because they don’t know they exist, don’t derive any personal benefit from their use, or refuse to be tracked regardless of privacy assurances. There is no way that Americans will accept an opt-out model in which they default to being users and also no way that a significant percentage will otherwise opt in.
- These apps have never worked in a country where their use was voluntary, nor rolled out late in a country whose initial COVID-19 response was as indecisive as ours.
- Accuracy is questionable. The six-foot range will flag contacts between cars, on opposite sides of plastic shields in stores, and where physical protection is in place and makes virus spread unlikely. I’m not confident that a record of whom I’ve passed within six feet of is all that useful in controlling coronavirus spread.
- Users are expected to manually enter their positive COVID-19 test result for the benefit of others who will then be notified. Then, unlike in other countries, it’s up to those people who get the “you’ve been exposed” warnings to take action since they are not identifiable.
- Contact tracing requires having a strong system of 14-day quarantine in place, such as providing private living space and checking up on self-monitoring. We can already guess that many nursing home residents, mass transportation riders, homeless people, prisoners, and laborers who live in employer-provided dormitories are infected, but any isolation is voluntary and limited by their resources.
- The bottom line: this sort of contract tracing works only if at least two-thirds of Americans use the app and we roll out widespread COVID-19 testing to identify those who are infected but symptom-free to catch potential spreaders early. Even then our society, as it returns to being mobile, will make it nearly impossible to address the potentially hundreds of people that someone could pass near in the days or weeks before they receive a positive test result.
From Looking For Answers: “Re: Clarify Health Solutions. Laid off 70 employees, about 40% of its workforce, on March 19. KKR gave it a bridge loan instead of agreeing to a Schedule C. I’ve seen nothing online, but a former colleague who used to work there told me.” Unverified. I don’t think I’ve ever heard of this particular analytics vendor, which has raised $63 million, almost all of that in a September 2018 Series B round by KKR. The company announced a couple of COVID-19 apps less than a week after this rumored layoff.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Mayo Clinic (MN) will invest in Current Health and work with the company to develop COVID-19 predictive and remote monitoring technologies.

From the Cerner earnings call:
- Chairman and CEO Brent Shafer says he is pleased with the productivity and performance of its 27,000 employees after the majority of them moved to working from a virtual environment.
- The company expects the VA and DoD to revise their timelines due to COVID-19 and Cerner has factored that into its guidance.
- Cerner expects a slight drop in next-quarter bookings, but says clients are generally moving ahead and it won’t be a lot different than usual, especially since unlike the 2008 market crash, health systems were doing fine financially before coronavirus and stimulus money will help get them back on their feet.
- President Don Trigg says the federal government’s role of top regulator and payor will expand due to COVID-19 and health system consolidation will accelerate and extend into ambulatory practice.
- Clients are starting to ask about getting into the queue for services that will be in high demand.
Sales
- Penn State Health selects RCM software and services from R1 RCM.
Announcements and Implementations
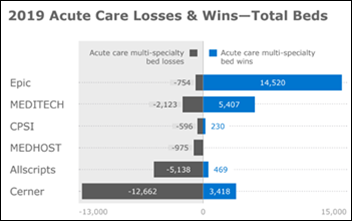
A new KLAS report on US hospital EHR market share finds that Meditech Expanse is drawing new interest from customers outside its usual small-hospital base, with a new 400+ bed health system sale in 2019 giving the market a chance to see how Expanse scales. Meditech won about half the decisions made by its legacy customers in 2019, and half of its losses came from product standardization and provider M&A. Cerner saw its first-ever decrease in market share after losing four big clients in 2019, with its losses most often due to customers who standardized on Epic and those who were frustrated with Cerner’s revenue cycle management solution. Epic has grown to cover 40% of US acute care beds, with its new wins split between new decisions and standardization and acquisitions. Allscripts continues to steadily lose market share, with 2019 losses of customers of Sunrise (eight), Paragon (16), and Horizon (seven). Small, standalone hospitals were left with few choices after Athenahealth exited the inpatient market, with Cerner CommunityWorks and Meditech Expanse coming closest to meeting their needs.
Epic will embed telehealth into its EHR using Twilio Programmable Video, which is also used by Kaiser Permanente, MDLive, Doctor On Demand, and several health systems. Investment firms are already warning companies like Teladoc that their reach into academic medical centers may be constrained with the availability of an Epic-embedded virtual visit platform that is staffed by a hospital’s own clinicians.
Critical access hospital Macon Community Hospital (TN) goes live on Cerner in a go-live that Cerner managed remotely.

Allegheny Health Network’s Saint Vincent Hospital (PA) implements virtual ICU software and support from Mercy Virtual.

Greenway Health announces GA of GRS Express, a suite of expedited RCM services to help practices maintain cash flow.

EPSi announces GA of COVID-19 Planning Analytics to help providers anticipate ICU capacity, financial burdens, and the impact of resuming elective procedures.
QliqSoft will incorporate the Suki voice-enabled digital clinical assistant in its telemedicine platform to create medical notes and perform tasks such as EHR information retrieval.
Reliance EHealth Collaborative is developing COVID-19 use cases via data management, analytics, and reporting from IMAT Solutions.
Government and Politics

HHS awards $20 million to six organizations to help them expand telemedicine access.
COVID-19
Conflicting studies on the use of remdesivir came out Wednesday following several incidents in which leaked information found its way to mainstream media headlines. Preliminary results from a government-run trial showed patient time to improvement was 11 days versus 15 days for placebo, which meets the NIH study’s endpoint, but the drug did not provide a statistically significant improvement in survival rate. Almost simultaneously, results of a peer-reviewed study performed in China showed no benefit from using remdesivir. Experts say the benefit isn’t necessarily how well remdesivir works, but a reminder that the virus has vulnerabilities that can be exploited incrementally to improve outcomes even in the in the absence of a blockbuster drug, as was the case with HIV/AIDS.
NIH announces a $1.5 billion challenge for rapid deployment of coronavirus diagnostic tests.
A Kaiser Health News article observes that hospital information that is stored in proprietary, siloed EHRs cannot support hospitals sharing their COVID-19 treatment experience. Experts say everybody knew from the early days of the $36 billion Meaningful Use program that hospitals were seeking systems to optimize billing, not public health. Health Catalyst CTO Dale Sanders was quoted in the article as saying that CDC should have developed a coronavirus data collection plan, with standardized terminology, that would have allowed hospitals with non-interoperable EHRs to look at the big picture (Health Catalyst is a member of the COVID-19 Healthcare Coalition that is trying to assemble information for real-time support). Public health systems are also often unable to accept electronically submitted information, requiring hospitals to complete manual forms that can take up to 30 minutes to complete and often even then with missing information.

Most of the tent hospitals that were expensively built to provide services to an expected crush of COVID-19 patients are scheduled for closure, having seen few patients:
- New York is shutting down two tent hospitals that didn’t see a single coronavirus patient, having spent $350 million in federal taxpayer money to plan and build temporary facilities. The only field hospital that saw patients, at Javits Center, will close Friday after treating 1,000 patients in the 4,000-bed facility.
- Chicago’s pared-back, $64 million, 500-bed hospital at McCormick Place has treated only 12 patients.
- Detroit’s 1,000-bed convention center hospital has seen just 36 patients and is scheduled for closure.
- Philadelphia will close its 200-bed temporary hospital in two weeks. It has never had more than six patients at a time.
- New Jersey’s four field hospitals totalling 1,000 beds have treated 346 patients.
- The temporary hospital that was set up in the New Orleans convention center is averaging 100 coronavirus patients.
- The Navy’s 1,000-bed USNS Comfort will leave Manhattan this week to return to its home port of Norfolk, having treated just 182 patients.
The Atlantic says Georgia’s rush to reopen businesses is an experiment “to find out just how many individuals need to lose their job or their life for a state to work through a plague” given that Georgia is moving forward despite meeting none of the accepted testing and infection success benchmarks. On the other hand, the article fails to note that the same number of people are likely to die either way, just over longer periods, unless we complete a technological Hail Mary in the form of a vaccine, effective treatment, or a sound containment containment strategy.
Privacy and Security
The New York Times says Europe’s world-leading GDPR privacy rules are falling short of expectations because of small national data protection budgets, lack of enforcement, and tech company pushback. The only tech company to have been penalized is Google, which paid a relatively paltry $54 million versus the law’s maximum of 4% of global revenue. Public experience with GDPR has been mostly negative as web users are forced to click through countless pop-up consent windows.
Other

Regions Hospital (MN) works with Medtronic to develop software that allows providers to remotely monitor and adjust ventilators. Regions providers say the software, which went from concept to implementation in just 10 days, has cut down on in-room visits to COVID-19 patients by 50%, and helps conserve PPE. Several other hospitals are also piloting the technology.
Experts say it’s not the imagination of Zoom users that the videoconferencing app leaves them anxious, unable to think clearly, and tired — the app’s bandwitdh-conserving degradation of video quality leaves the brains of users to fill in the image’s gaps, especially in trying to analyze poorly rendered or out-of-sync facial expressions. Telephone calls, oddly enough, offer a more natural feeling of presence and engagement.
Sponsor Updates
- Elsevier adds resources for biomedical and scientific researchers to its free Coronavirus Research Hub.
- The Chartis Group publishes a new paper, “After the Surge: Five Health System Imperatives in the Age of COVID-19.”
- InstaMed releases the 10th edition of its “Trends in Healthcare Payments Annual Report.”
- InterSystems makes available the latest version of its HealthShare suite of connected health solutions, including capabilities to support final federal interoperability rules.
- Engage announces feature updates for its Wait Times app.
- Impact Advisors publishes a white paper titled “COVID19 Federal Stimulus Package – Impact on Providers.”
- HBI Solutions names Jackie Porter, BSN, RNC-E (Syapse) client success director.
- Meditech highlights the successful utilization of its virtual visit functionality at Citizens Memorial Hospital (MO), Grand View Hospital (PA), Avera Health (SD), and Mount Nittany (PA).
Blog Posts
- 3 Practices Finding Success with Telehealth (EClinicalWorks)
- Balancing the New Normal: Parenting, Practices, and Patients (PMD)
- Transitioning to a Remote Discharge Planning and Case Management Workforce (Ensocare)
- RT@COVID19 – Answering Sam Gamgee’s Questions (CloudWave)
- COVID-19: The Importance of Lab Professionals (Optimum Healthcare IT)
- COVID-19 Crisis: Why Now is the Time to Invest in Glycemic Management (Glytec)
- Leadership Insights with Scott Becker (The HCI Group)
- Healthcare Crisis Underscores Strategic Importance of Strong IT Support (HCTec)
- Struggling with Working from Home? Try These Tips! (Healthfinch)
- The impact of COVID-19 on healthcare systems from an imaging point-of-view (Hyland)
- Rapidly Expanding Capacity for the Coronavirus Pandemic and Beyond (Impact Advisors)
- 7 best practices for supporting telehealth, virtual care, and remote visitation amid COVID-19 (Imprivata)
- Provider Directory: How a Golden Record Can Be a Big Hit (InterSystems)
- Agility and COVID-19: IMO’s ongoing pandemic response (Intelligent Medical Objects)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



Thanks for sharing the link to the “Why Zoom Is Terrible” article – the phone seems to work better than Zoom. KISS.
Re: Tent hospitals. The cost is terribly high, but before anyone bemoans government waste, consider that 1) the cost amounts to roughly 15% of the total $3T federal response, 2) a couple of months ago we were projecting a much more severe impact (over 80k fatalities vs the 60k we have today) and we REALLY thought we would need these facilities after the news from China and Italy, and 3) the media images of tent hospitals in Central Park and other urban areas served as a powerful visual reminder of the severity of the crisis, and may have reinforced the need for social distancing in the hardest-hit areas.
Spot on…I don’t appreciate all these news pieces insinuating that it was wasted dollars. Next time something similar happens, we don’t build them, and we need them, what are we going to say? Based on what happened in China and Italy, it really looked like they would be needed, and it’s not something you can build overnight.
“Dentists have been telling me to brush my teeth all my life, but I don’t have any cavities! Look at all that money I wasted on toothpaste!”
Totally agree. Atypically cynical post from Mr H, with no editorial comment. Poor preparation and lack of investment in public health were some of the reasons the pandemic has been so bad, yet when we do try to prepare , the critics come out. Anyone working in Queens over the last 6 weeks was happy to see this “excess” capacity. Morgues are already overflowing; how much worse would it have been if the capacity was needed and not there? The critics are probably the same people who complain about all the disincentives for prevention in US healthcare.
If you are concerned about the cost, then I would suggest finding less expensive, more nimble ways of providing this type of service when needed. For those treated in the tent hospitals, there was certainly value in having a place to go. Hopefully we can learn more about the process so that the next time rapid expansion of capacity is needed, we are more efficient. I would write more, but have been working in an ICU in New Jersey and I am weary.
RE remdesivir study: statistical significance means less than 5% probability the result is due to chance, but you have to specify the one thing you’re measuring in advance. They didn’t do that—instead changed from mortality to recovery time. This sort of thing raises the question of how many more slices of the apple they would have taken until something passed the test.