News 6/17/09
From Scot Silverstein: “Re: your idea of ‘on a less contentious level, at least fully defining the extent of practice variation in real time and alerting physicians of areas for improvement.’ That was an approach suggested over 20 year ago: Perry L. Miller [Yale Center for Medical Informatics}, Expert Critiquing Systems, Springer-Verlag New York, Inc., Secaucus, NJ, 1986. Your ‘anon-a-doc social networking’ idea is interesting, but then how to differentiate advice from good docs and bad docs” I wasn’t necessarily picturing that the docs would be anonymous, so their advice could be evaluated in the same way as Amazon and Citysearch reviewers. And like those sites, I would assume that since good docs vastly outnumber bad ones that an aggregated set of opinions would lean heavily toward the best answer.
From Pharmacist H: “Re: Pittsburgh medication system problems. Whoever wrote about the electronic medication problems of an unnamed vendor is shouting fire in an inferno.”
From HITMan: “Re: physician variation. I am a non-clinican IT guy and CIO. I am constantly amazed by the quality care that my clinician colleagues deliver, but I also keep in mind the point that the most significant healthcare advances in the past 80 years have been driven not by physicians but by public health initiatives (think immunizations). I still think, however, that physicians think too highly of their own value and the quality of their EMR progress notes. Ask some nurses — they would probably have good insight about who really brings value to the health system equation. Nonetheless, I stand by my comment that variation is the enemy of perfection and that by forcing physicians to deliver care in an evidence based-way (mon dieu!) and standardizing the care they deliver that we can improve the care that we deliver to our customers (I mean patients).” I agree with nearly everything you say, especially the primary role of public health (and not medical treatments) that have extended life expectancy. However, good doctors have told me this: evidence-based medicine works for 80% of the people, but it doesn’t allow physician discretion in identifying and managing the other 20%. Maybe docs ought to be able to justify and exclude those exceptions, which is what all of us would want if we were one of those patients. My working assumptions are (a) doctors don’t go to work each day with the intention of harming patients; (b) they will do the right thing if they know what it is; and (c) the view from the cheap seats is different (sometimes better, most often worse) than from the playing field. Evidence-based care is fine as long as it has been developed and vetted by practicing doctors, which isn’t always the case.
From Mr. Pepperton: “Re: Fletcher Allen. They have gone live with Epic and the project was a huge success.”
Thanks to DrLyle for his HIStalk Practice writeup on the President’s speech to the AMA yesterday.
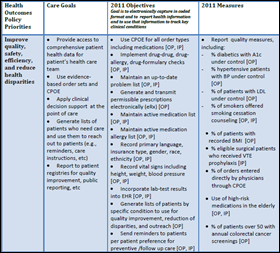
HHS publishes its meaningful use matrix (warning: PDF) with these priorities:
- Improve quality, safety, efficiency, and reduce health disparities
- Engage patients and families
- Improve care coordination
- Improve population and public health
- Ensure adequate privacy and security protections for personal health information
My first impression: excellent. Some of the criteria will be a bit soft to measure and validate, but most of them are not only solidly thought out, they are objective and absolute. They are ratcheted in through 2015. What do you think? Better or worse than you expected? Inga weighs in below as well.
Nurse Deborah Leyva and a technology attorney (her husband, I think) have put together the HIPAA Survival Guide, which includes a section on HITECH.
McKesson says it won’t raise base salaries of its executive officers in 2010. It also claims it will raise the bar on executive bonuses. That may not have been a coincidental announcement: it hit the wires at about the same time as stories about CEO John Hammergren’s FY2009 compensation: $29.7 million, including a $12 million bonus. That’s damn generous considering the company’s stock dropped 33% over that same period, shafting those worker bees who invested their rather more modest proceeds in company stock. Doesn’t anyone in healthcare work for a reasonable wage any more, other than the few nuns left?
Sarasota Memorial Hospital (FL) is using social media to communicate with the public, including Twittering its $49 heart disease checkup special.
GE has set aside $100 million to loan new customers its EMR systems who don’t have the upfront cash to benefit from ARRA, rather like those used car dealers that offer to use your yet-unreceived tax refund as a down payment. Everybody rides!
Vanderbilt clinicians and informatics professionals are testing what they say is the first real-time sepsis detection system, to be followed this year with decision support tools to guide its treatment. Their description of a “state-based decision engine” is interesting: “Essentially, this involved breaking down the guidelines into a series of independent processes that can take place sequentially or simultaneously. ‘This really captures the way doctors work. If we see low blood pressure, then we think of one set of treatments. If we see low blood sugar, then we think of another set. If we see the two together, then we consider a third set of possible measures we can take.’”
Sentara Healthcare (VA) works with Picis to integrate its LYNX Medical Systems ED revenue management system with Epic’s EDIS. Sentara says it has gained millions of dollars in revenue from the integration. Picis also announces LYNX C/Point, a revenue management system that reduces the risk of recovery audit contractor (RAC) penalties.
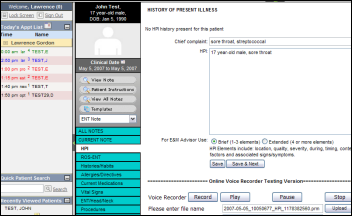
Nuance releases the results of its EHR Meaningful Use Physician Study, which found that more doctors (75%) want a better way to document care than with a mouse and keyboard than want stimulus money (69%).
The AMA adopts principles for EMR breaches: (1) tell the patient; (2) follow appropriate procedures for disclosure; (3) place the interest of the patient first; and (4) give the patient information to mitigate the consequences.
Orlando Portale, Chief Innovation Officer of Palomar Pomerado Health, and Jonathan Bush, CEO of athenahealth will speak at the Fortune tech Brainstorm 2009 next month in Pasadena, CA. Also on the dais: Barry Diller, Robert Iger, Ashton Kutcher, Mark Hurd, and bunch of other business luminaries. Registration costs $3,500 and the hotel is $260 a night. The conference offers press passes, so maybe I’ll show up.
New hospital software: Hysteria Hospital: Emergency Ward, a game for the Wii and Nintendo DS systems.
Followers of a saint-like woman named Amma who dispenses hugs and runs charitable hospitals says her methods will be replicated on a larger scale. Among her organization’s projects is healthcare IT. “Amritanandamayi’s volunteers have made significant contributions to various programs in India, including telemedicine and electronic medical records. Gottsegen helped develop a computerized record-keeping system that is now used in all of Amritanandamayi’s medical centers throughout India. He and a team of volunteer software engineers from India and California are adapting it for use in the U.S. health care system. If they can win a piece of the federal stimulus funding earmarked for electronic health records, they hope to compete with other top developers.”
Here’s an interesting quote: “It is no more practical to have ‘health insurance’ to pay for prescription drugs and routine doctor visits than it is to expect your auto insurance to pay for your oil changes and tire rotations … Health insurance does not insure your health, nor was it ever intended to. Health care insurance, formerly called ‘medical insurance,’ is merely an instrument of neutralizing risk … As a strictly financial planning endeavor, the issue never seemed to be discussed in terms of being ‘a right’ or in terms of ‘compassion.’ But ‘medical insurance’ as a component of financial planning has morphed into ‘health care’ as a right for everyone in the new political parlance.”
There’s a nasty brouhaha brewing over at AuntMinnie.com. Dr. Dalai tells me, involving an Ohio hospital group’s decision to replace its local radiology group with a national firm. I couldn’t follow it all on the forums, but it involves back room deals, accusations of shoddy work, tie-ins of the new company with Mass General and at least one executive of the American College of Radiology (to which the displaced rads pay dues), and clueless hospital administration. It’s not IT related, but if you want to witness the squabbling that happens when a healthcare provider’s income is threatened (both the hospital’s and the rad group’s, in this case) it’s worth a look as a picture of things to come.
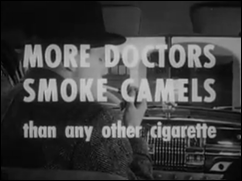
Inga ran an old commercial in which doctors extolled the virtues of Camel cigarettes. Interesting: this article points out that JAMA accepted tobacco company advertising starting in the 1930s, although that has now replaced by the drug companies that fuel 20% of its budget. And this quote might be apropos about HIMSS and HIT vendors if you swap the words: “… the AMA has found that it can’t rely on membership dues to generate the kind of revenue that the AMA leadership is looking for. Instead, they’ve turned to corporate sponsorship—businesses with money to make by casting a veneer of medical respectability around their pursuit of profit find a relationship with the AMA to be useful.”
AMICAS pays off patent troll Acacia Research, which if I recall, claims a few generic patents it bought means it owns the concept of PACS.
Weird News Andy, an artist whose medium is obscure news stories, has been at it again:
- A hospital nurse in London is fired for shutting off a baby’s heart alarm so she could continue chatting with another child’s parents.
- Also in the UK, a nurse is fired for complying with the wishes of an elderly patient’s family to perform no aggressive measures on her.
- A British female athlete dies in a private hospital when doctors bungle a surgery to reduce sweating of her hands and feet.
- A Polish woman wakes up in a morgue body bag after being declared dead.
- A new study says finds that men are 40% more likely to die of cancer than women because they refuse to see their doctor.
HERtalk by Inga
Full disclosure: I did not sit in on the HIT Policy Committee meeting today, though I did read through the “meaningful use matrix” and other documents listed on the ONC website. I realize the document is still in draft mode and these are not the final definitions. However, I’m not understanding how some of the stated “policy priorities” match with the measurements and objectives. For example, one of the stated policy priorities is to improve quality and efficiency and to reduce health disparities. To prove “meaningful use” as it relates to this priority, a provider must generate quality reporting measurements (e.g, % of diabetics with A1c under control and % of hypertensive patients with blood pressure under control, etc.) For this same quality priority, the listed “objectives” for 2011 include maintaining current medication and problem lists and incorporating lab results into EHR. In other words, there is no clear tie-in between how meaningful use will be measured (by producing reports) and the policy priority (improving quality). The assumption is that if a provider maintains a current medication and problem list, care will improve. But does that correlation really exist? Admittedly the connection between some of the priorities and measurements seem more straightforward than this one. Regardless, if we are going to be handing out millions of dollars, I want to feel assured that my money makes a difference. Simply being able to create a report does not mean a doctor is necessarily providing better care.
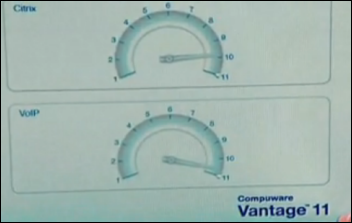
Should you be looking for a job change, Computerworld just announced its Top 100 Best Places to Work in IT 2009. If you would prefer working for a health system, try Lehigh Valley, Cedars-Sinai, Texas Health Resource, HCA, VHA, Norton Healthcare, or Adventist. Lehigh Valley earned the highest spot (43), largely because of its strong commitment to employee feedback. Over 200 IT staff receive annual reviews that include personalized comments from a team director CIO Harry Lukens, plus an annual review meeting also attended by the CIO. Employees also have a chance to participate in a "Wild Idea Team” that is tasked with finding new technologies for the organization. The best HIT vendor employer: Cerner. Perks at Cerner include work-out facilities, including an indoor pool, a Montessori school, and an on-site primary care center. Free pizza was not mentioned. Quest Diagnostic, Compuware, and Red Hat also made the list.
Virginia is the latest state to formally announce plans for a statewide HIE. Governor Timothy M. Kaine says the Virginia Health Exchange Network will connect health plans, health systems, and state agencies.
KLAS releases its annual rankings for best-performing medical equipment vendors. The research company assigned Best in KLAS honors to six companies across seven categories.
A judge sentences a former Cedars-Sinai Medical Center employee to four years in prison after he pleaded guilty to stealing patient information to defraud insurance companies of $354,000. The former billing department employee billed insurance companies $1.3 million for treatment never provided. He gas to repay the $354,000 plus $62,000 in back taxes and penalties.
QuadraMed’s Affinity Revenue Cycle Management M8 software is now available for general release. QuadraMed also just introduced its Quantim HIM Workflow solution.
New Island Hospital (NY) names Larry Maggiotto its new AVP and CIO. Interim CIO Chris Cody is promoted to assistant director of health information management.
Certify Data Systems closes a round of Series B funding led by Ziegler HeatlhVest Partners LP.
Geneva Medical Center (OH) launches its EHR June 30th. Geneva is the first University Hospital system facility to go live on the $100 million system.
Newly live on EHR: Fletcher Allen HealthCare (VT). The hospital is in the midst of a $57 million project that includes automating its 750 affiliated medical practices.
PatientCompass, RelayHealth’s online business office solution, achieves Level 1 Service Provider Certification and has been validated as PCI DSS-compliant.
The CEO of the 15-bed Drumright Regional Hospital (OK) reports their Cerner-hosted EHR is fully operational and helping increase revenues.
As evidenced by the recent departure of Andy Eckert at Eclipsys, non-virtual organizations may be returning. Eckert chose not to leave California to live in Eclipsys’ Atlanta headquarters. Experts are now seeing more workers returning to traditional offices, particularly senior managers. I suppose if you have been working virtually for years and have to return a “real” office, at least you have a big shopping spree to look forward to.
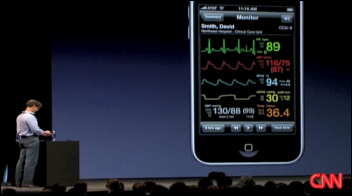
HIT Ladies: we are not alone. Researchers find that women are an increasingly important market for technology brands and that an estimated 45 million of us bought a digital product in the last six months. Sexy iPhones are just as much a fashion essential these days as the perfect shade of lipstick, and, of course, sexy pumps.






















































There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…