News 1/7/15
Top News

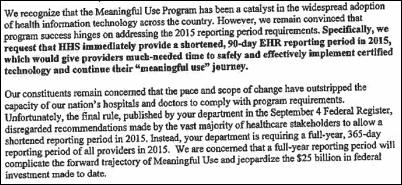
The American Medical Association says EHRs, ICD-10, prior authorization, and Medicare fraud detection programs are “barriers to providing high-quality care” that it will oppose in 2015. AMA will continue its push to make the Meaningful Use program more flexible, improve EHR usability, and expand EHR interoperability. It will also “urge regulators to ease this physician burden” of the October 1 implementation of ICD-10, study the physician workload impact of prior authorization, and push CMS to overhaul its RAC-centered “bounty hunter” fraud and abuse programs.
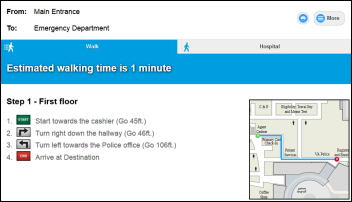
From Hallway: “Re: smartphone wayfinding apps. I passed along information on Jibestream that you mentioned in June 2014. I agree that this type of application will offer competitive advantage, not only with patients and visitors, but for new hires, for patient transportation, and for ancillary staff that need to deliver services at the bedside, maybe even eventually to route robots delivering supplies (I can just picture R2D2s roaming the halls).”
From Title Contender: “Re: smartphone wayfinding apps. Check out Logic Junction, whose solution works on both web and mobile with a single database that can be updated in real time.” The company lists Cleveland Clinic, LA County, Sarasota Memorial, and the VA as clients. The online demo is pretty cool and doesn’t require registration to run. If I were the company, I would white label the product and let hospitals sell ads or promote their own services to make it cost neutral.
HIStalk Announcements and Requests
I’ve ordered Eric Topol’s “The Patient Will See You Now” and Steven Brill’s “America’s Bitter Pill,” so I’ll have book reports soon.
The latest in my long line of pet grammar peeves: starting sentences with “there.” The next-to-latest: sites that post articles with a question as the headline, indicating that the author isn’t confident enough to actually answer the question (meaning: the article is a complete waste of time). I’m curmudgeonly even in restaurants whose menus gets overly cute by offering “veggies” and “mashers.”
Webinars
January 13 (Tuesday) 1:00 ET. “The Bug Stops Here: How Our Hospital Used its EHR and RTLS Systems to Contain a Deadly New Virus.” Sponsored by Versus Technology. Presenter: John Olmstead, RN, MBA, FACHE, director of surgical and emergency services, The Community Hospital, Munster, Indiana. Community Hospital was the first US hospital to treat a patient with MERS (Middle East Respiratory Syndrome). It used clinical data from its EHR and staff contact information from a real-time locating system to provide on-site CDC staff with the information they needed to contain the virus and to study how it spreads. Employees who were identified as being exposed were quickly tested, avoiding a hospital shutdown.
Acquisitions, Funding, Business, and Stock

Allina Health (MN) will take an equity position in Health Catalyst as part of a 10-year agreement in which the Allina will outsource its 60-employee analytics and quality improvement teams to Health Catalyst and will contribute its clinical expertise, while Health Catalyst earns a portion of its payment when Allina hits specific quality improvement targets as overseen by a governing committee. The organizations value the agreement at $100 million. I interviewed newly promoted Allina President and CEO Penny Wheeler, MD this week about the agreement and other topics.
Lexmark acquires Toronto-based medical imaging technology vendor Claron Technology for $37 million in cash. Lexmark will position the company’s medical imaging viewing platform and zero-footprint viewer within its Perceptive Software business, which offers a vendor-neutral archive and medical content management.
Staffing services company General Employment Enterprises acquires Jacksonville, FL-based medical scribe contractor Scribe Solutions.
Baltimore-based hospital hiring software vendor Pegged Software, which claims to have reduced employee turnover in its customers by an average of 45 percent, raises $9.2 million to increase its sales and marketing efforts.
Guided episode management software vendor Wellbe raises $2.42 million.
Honeywell renames its HomMed remote patient monitoring business to Honeywell Life Care Solutions.
The non-profit MedicAlert Foundation will reduce headcount and cut its budget “to better focus on its core mission of protecting and saving lives by serving as the global information link between members and emergency responders during medical emergencies and other times of need.” Beyond a variety of bracelet-type medical IDs, the organization offers an online health record linked to the medical ID number for an annual membership fee that starts at $19.99.
Sales

Saint Luke’s Health System (MO) chooses Phynd to create a single provider profile of its 15,000 referring and credentialed physicians.
Children’s Hospital of San Antonio (TX) selects Ingenious Med’s patient encounter platform.
People




HIMSS adds four new board members who will serve three-year terms: Michael Nusbaum (MH Nusbaum & Associates); James Peake, MD (SVP, CGI Federal); Christopher Ross (CIO, Mayo Clinic); and Ferdinand Velasco, MD (CHIO, Texas Health Resources).

CHIME names University of Michigan Hospitals and Health Centers CIO Sue Schade as its 2014 John E. Gall, Jr. CIO of the Year.

Rick Adam is named president and COO of analytics vendor Stanson Health. He has work for a variety of health IT vendors over the years, including Baxter, NEON, and Recondo Technology. The company’s board chair is Scott Weingarten, MD now with Cedars-Sinai after co-founding Zynx Health.

Halfpenny Technologies hires Carl Smith (Airclic) as CFO.

David Silberstein (Teradata) joins Leidos Health as service line director for analytics.

The former HHS acting director of cybersecurity is sentenced to 25 years in federal prison for distribution of child pornography, including participating in discussions with another member of a private website that the two get together to fulfill their mutual fantasies of raping and murdering children. The FBI says Timothy DeFoggi used the technology expertise he gained in working for HHS to evade detection, ultimately unsuccessfully.
Announcements and Implementations

Epic announces plans for Campus Five, a five-building expansion that will add 500,000 square feet of space, 1,600 offices, and 1,500 parking spaces, all with a children’s literature theme. The company says it needs the space because 45 percent of its employees are sharing offices. Epic’s Wizards Academy campus is already under construction and will open in about a year.
Connance adds a Claims Optimization platform to its predictive analytics solution.
The HCI Group creates a freely viewable e-book, “The Definitive EHR Go-Live Guide.”
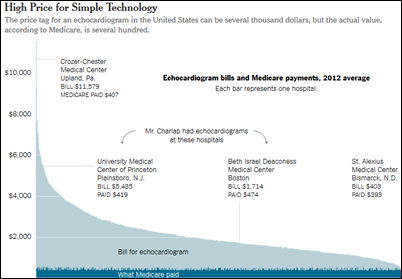
Steven Brill, who wrote a lengthy Time magazine cover story two years ago called “Bitter Pill: Why Medical Bills Are Killing Us,” says in a new book that the Affordable Care Act won’t help control healthcare costs because Democrats struck too many industry-friendly deals to get it passed. He adds in a Washington Post interview that organizations like Cleveland Clinic should be allowed to sell their own insurance under tight regulation, such as limits on hospital profitability and CEO salaries. He thinks insurance companies are the victims of providers who overcharge, leaving those insurance companies to run a low-margin business by abusing their customers. He says about ACA-driven value-based payments:
Sure, I think there’s more focus, for example, on hospital readmission for Medicare patients, which is costly, but in the sum total of things, it’s kind of a drop in the bucket. There are little things like that, but there aren’t any big things, there’s nothing to control the price of drugs, there’s no tort reform, there’s nothing to control the profits of allegedly nonprofit hospitals. There’s nothing to deal with the profits and the secret contracts that device-makers negotiate with hospitals that buy their products.
It’s not just the lobbying influence. You combine that money with the emotional pull and fear that people have when they think about healthcare. People care more about their health than they do about healthcare policy. And then you add to that the multi-channel political power of the healthcare industry in every congressional district, because in about every congressional district, the largest employer is the local hospital. And the local hospital is again seen as a charity. You combine that kind of local power with the lobbying power, with the fear and emotion that’s attached to healthcare, and that makes for a toxic political stew.
How is that going to change? I think the only way it’s going to change relates to what the thinking was in Massachusetts when Romneycare passed. They’re very candid about this — we’ll give everybody coverage and then when people see how much it costs, there’ll be this huge political wave to say we have to reform this or we’re going bankrupt.
Technology
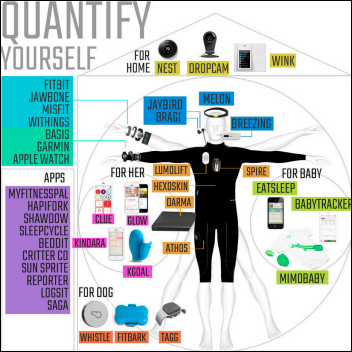
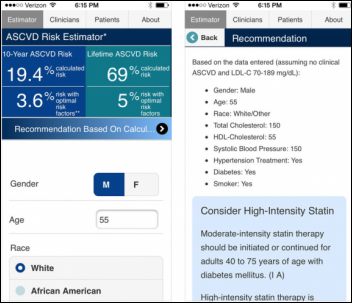
NPR’s “All Things Considered” covers the consumer medical devices being displayed this week at the International Consumer Electronics Show in a piece titled “Self-Tracking Gadgets That Play Doctor Abound at CES.” It mentions CellScope (a phone-powered ear camera that sends images to doctors for diagnosis) and Neurotrack (quiz-based Alzheimer’s diagnosis). The article wanders confusingly into thinking that phone apps have something to do with cyberattacks and telemedicine, so the only interesting aspect is that NPR wrote up the article in the first place.

An interesting use of telemedicine: St. Joseph’s Regional Medical Center (NJ) connects ED victims of domestic violence with county court officers, allowing them to take out restraining orders within 45 minutes directly from the hospital. The program is being expanded to make an iPad-equipped judge available around the clock to handle night and weekend cases, which are the majority.
Other
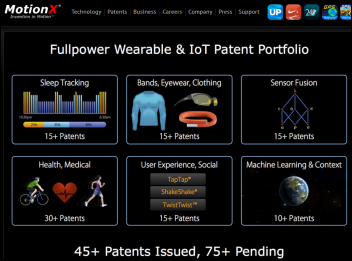
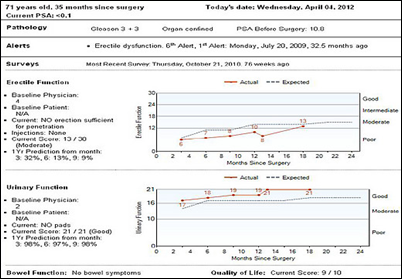
Physicians responding to a Sermo poll name wearables-based remote patient monitoring and telemedicine as the top two expected trends of 2015.

Surgeon and writer Atul Gawande, MD, MPH weighs in on technology in an interview with Bob Wachter, MD:
Information is our most valuable resource, yet we treat it like a byproduct. The systems we have – Epic and our other systems – are not particularly useful right now in helping us execute on these objectives. We’re having to build systems around those systems … the issues have less to do with systems than with governance … the residents feel they’re caught up in this world where everything they need to know is on the computer screen. That’s creating angst in their day-to-day life. You go up to the floor of the medical service in my hospital, and there are no doctors there. They come, they see the patients, and then they escape to this tribal room where all 15 residents hang out together, each doing his or her computer work. That means that many of the informal interactions that used to occur between the docs and the nurses, or the docs and the patients and their families, have withered away.
A veteran sues the Atlanta VA hospital that was treating him for PTSD, claiming that the single dose of antidepressant he was prescribed created a weeks-long erection that made him the laughingstock of doctors and nurses and resulted in improper treatment that left him disfigured. “One had mentioned that I should line up all the women. I haven’t had that many people who had seen it in my whole life until I went to that hospital.” His attorney (Mr. Johnson, strangely enough) cites another patient who took the same drug with the same result, to whom a jury awarded $10 million.

Weird News Andy drives us into the new year with a story he titles, “Making a turn for the better.” Surgeons remove a turn signal lever from a 1963 Thunderbird from the arm of a man who had been in a car accident 51 years ago, unaware until now that he had a seven-inch piece of metal embedded there.
Sponsor Updates
- Phynd publishes a blog post titled “Direct Addresses Are Yet Another Reasons Hospitals Need to Move to a Single Provider Profile (SPP) Model.”
- ADP AdvancedMD will integrate its EHR with physician practice reporting from Iron Bridge Integration, giving customers access to pre-built connections to 57 registries in 48 states to help meet Meaningful use Stage 2 requirements.
- Chadron Community Hospital (NE) successfully attests to Meaningful Use Stage 2 using NTT DATA’s Optimum product suite. I interviewed CIO/COO Anna Turman several months ago and it’s still among my favorites.
- Netsmart publishes several new white papers: “In Transition: How Electronic Data Sharing Enables Improved Outcomes and Reduced Costs,” “5 Things to Consider When Selecting Your New (Next) EHR,” and “Transforming the EHR into a Knowledge Platform to Ensure Improved Health and Healthcare.”
- Medhost describes the use by Larkin Community Hospital (FL) of its YourCareLink integration service to automate public health reporting for Meaningful Use Stage 2.
- Amerinet will offer the interoperability and population health management solutions of Sandlot Solutions to its members.
- A market research survey finds that VMware’s AirWatch enterprise mobility management solution is the #1 choice of decision-makers, handily beating out MobileIron.
- Four Army National Guard locations will use AtHoc’s network-centric crisis communications system, which allows base officials to quickly send deployment orders and emergency notifications via text, phone, and desktop.
- Besler Consulting offers a review of the FY2015 Hospital Outpatient Prospective Payment System.
- A CareSync blog post reviews CMS’s chronic care management reimbursement program and how doctors can use the company’s CareSync CCM product.
- Clinovations posts an article titled “Patient Access: What Does Failure Cost?”
- CommVault announces the schedule of its “Hockey Helping Kids” fundraiser.
- DataMotion publishes an article, “Want to ensure secure and compliant data exchange? Integrate security!”
- Divurgent will participate in the HIMSS East Tennessee Summit on January 22, 2015 in Knoxville and the HFMA Florida Mid-Winter Conference January 26 in Miami.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.































































































































































































Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…