Curbside Consult with Dr. Jayne 3/2/20
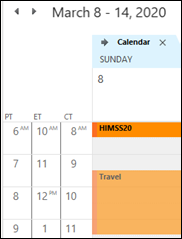
We’re definitely in the pre-HIMSS doldrums, with very little going on and even less news about it. Anyone who has a major announcement is going to hold it for the big show, even though odds are it will get lost in all the noise. Or the silence, if HIMSS chooses to cancel the event.
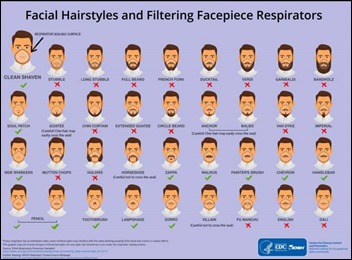
Most of the non-IT news out there in the healthcare realm is about the novel coronavirus and its transition to community spread within the US. Lots of chatter about how organizations are gearing up to identify and track it, but there are still serious challenges as far as how healthcare organizations are actually going to manage the patients especially given shortages of masks, gowns, and other critical supplies.
We finally had some surgical masks appear in our workplace this weekend, although it’s not clear if the supply will hold out or if the office will be replenished if we run out again. Most of the time we’re using them to help reduce the risk of flu transmission.
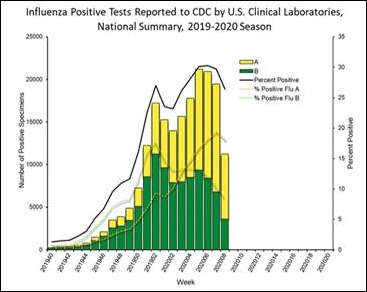
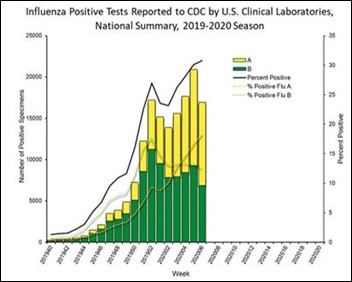
I was glad to see the most recent CDC numbers show a sharp decrease in positive flu tests. However, I think some of that downturn might be driven by people who aren’t coming in to be tested because they know just about everyone they’ve come in contact with has flu, so they’re just assuming a diagnosis and staying home. Several local schools have closed for deep cleaning as well, so at least they will be well practiced when coronavirus arrives. Our practice is as busy as ever with multiple providers covering extra shifts to make up for those who are out with flu.
Mr. H mentioned in his Monday Morning Update that Cisco is canceling, and there are plenty of rumors about other companies that are bailing out but haven’t announced it yet. HIMSS has been uncharacteristically slow in sending out invites (or “sorry, you’re not invited” notices) for many of their breakfast and lunch events, which is annoying both to the attendees who tried to register for them as well as the vendors who are paying for them. I’ve heard of many companies that had previously decided to downsize their exhibit hall presence and were planning on sending fewer employees than past years, so it would be less of a loss if they decide to cancel.
For those of us who aren’t being subsidized by a vendor or employer and who attend out of pocket, it’s not a small financial hit. Even if it is canceled, I have half a mind to go anyway and just enjoy being somewhere warm with a pool. On the other hand, I could stay home and catch up on all the things I haven’t been able to do since flu season has been so exhausting. I have some Maintenance of Certification questions I need to do for my boards and I would no longer have an excuse to dodge them. There’s also taxes to file and a shower to re-caulk, so the possibilities are endless for fun and excitement.
In the event that HIMSS goes forward, and a good chunk of exhibitors decide to show, I always get the question about what I’ll be looking for or what I want to see at the event. Here’s a short list of things I’m interested in:
- Ambient intelligence, smart exam rooms, and the like. How close are they to being able to make this work for in-the-trenches primary care practices? Are the solutions able to handle the scenarios where anything could walk through the door, and most of the time patients present with multiple and complex problems? Are they able to integrate with multiple EHR platforms or just the big ones? There are thousands of physicians across the US who are in need of such solutions but who don’t have Epic or Cerner.
- Telehealth. What do consumer-facing organizations have planned for the next five years? Will hospitals and health systems continue to try to do internal programs, or will they partner with some of the national players? Will the institutionally-focused vendors merge or partner with the consumer-facing ones? Will they be able to thrive financially, or will they continue to run on thin margins?
- Patient engagement. Are vendors really able to drive the needle for deliver patient outcomes, or is it all flash? Do the apps have staying power for patients or are they like fitness trackers and other solutions that patients use for a few weeks or a few months and then abandon?
- Helping the “little guys” succeed. What solutions are out there to help small practices or organizations that aren’t in the 800-pound gorilla range? What’s out there for people that don’t have half a billion dollars in the bank ready to spend on IT solutions?
- And finally, one of the least provider-facing but very important topics. What’s new in terminology, taxonomies, and all the “guts” that make the systems run while trying to facilitate interoperability and data exchange? I’ve heard that there may be some cool things on the horizon that could be transformative from the informatics perspective. I do love the logic and organization of a well put-together system, and if there are tools that can make that better, I say bring them on.
We should know soon whether HIMSS is a go or no-go and people can start adjusting their plans accordingly. If you’ve already decided you’re not going to attend, how do you plan to spend your time? Will you play catch-up on projects or are you so busy that staying home will just keep you from falling behind? Leave a comment or email me.

Email Dr. Jayne.


















Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…