Monday Morning Update 8/21/23
Top News
Point32Health, the second-largest insurer in Massachusetts, reports a six-month loss of $103 million that its CFO attributes almost entirely to a security breach at Harvard Pilgrim Health Care.
Harvard Pilgrim discovered the ransomware attack on April 17, 2023. Its website and online member accounts were offline for more than two months.
The hackers gained access to the protected health information of 2.5 million people, which was exfiltrated from its systems.
Reader Comments
From Cosmos: “Re: Meditech. Has quietly shut down its professional services division. Their website was just scrubbed of any mention of this service.” Confirmed, at least the “scrubbed from the website” part. The company hasn’t replied to my inquiry from Friday or the one from mid-May when a reader first told me that the service was being eliminated, four years after it was announced. UPDATE: Meditech re-sent a response from my May inquiry that I didn’t receive, with this update:
MEDITECH will continue to offer services for analytics and quality initiatives to further the widespread adoption of these expert-based solutions across our customer base to ensure customer success. We are in the process of defining all of these services and will release more details on our website as they become available. Going forward, customer requests for large-scale, full implementation project work will be directed toward MEDITECH-certified consulting firms. All existing contracts will be honored to ensure customer success.

From Baffle; “Re: HIStalk search. Could you add a function that returns pages with links?” The existing search function at the top of each page does that, although it’s really just a Google site search. Everybody would like to be able to search with sorting or filters by date range, but I’ve spent money several times on custom search engines and WordPress plug-ins that failed to work ideally. A viable company will eventually develop an affordable ChatGPT-powered chatbot search tool that will help catalog the treasure trove of industry information that is contained in the 16 years’ worth of HIStalk content — I didn’t save information from the old site host from the first four years – and I’ll be excited to implement that. Everything here has already cleared the bar of being both newsworthy and concise, so powering that with ChatGPT-type access would be powerful for market research and learning from the past.
HIStalk Announcements and Requests
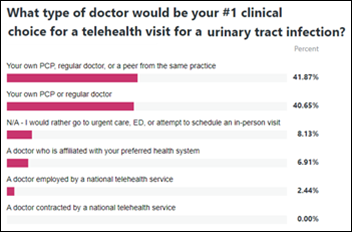
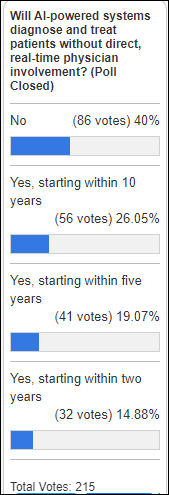
Most poll respondents would like having their UTI treated via telehealth, but with a doctor or health system they are familiar with rather than someone from a national telehealth service.
New poll to your right or here: Do you think it’s good that hospitals are consolidating into huge health systems? I set up the poll, the choices of which are admittedly clunky by necessity, to allow you to answer in your multiple roles as a consumer, taxpayer, and health IT employee.
Listening: 90s-style grungy indie rock from Blondshell, which is actually just LA-based Sabrina Teitelbaum under a far more marketable brand along with a backing band that can rock hard. The concept of “band” is fading fast in favor of one-shot collaborations and solo artists hiring other players to retain career flexibility, revenue, and the benefit of independent solo craftsmanship.
The industry seems to be thawing out again and competitors are repositioning themselves after a year of hunkering down, so this is for their marketing folks. Current HIStalk sponsors get free spotlights and text ads, while prospective ones can talk to Lorre about the benefits of full-year exposure. Startups and former sponsors might even get a lagniappe. Lorre also has a single Top Spot banner for companies that are seeking maximal exposure and the satisfaction of always seeing their ad atop those of competitors. Sponsors get zero influence over news and opinion, but that’s to their advantage since decision-makers will bail quickly on thinly veiled pay-for-play and inexpert babbling.
Webinars
August 24 (Thursday) 2 ET. “RCM analytics in action: How to use your data to drive decisions + revenue.” Sponsor: Waystar. Presenter: Laura Tungate, solution strategist team lead, Waystar. This webinar will describe how to use RCM analytics to take control of your data even if you use outdated or multiple tools. Attendees will learn how to target improvements, describe the KPIs that are key to revenue cycle leaders, prioritize dashboards that spotlight organizational goals and build alignment, and how and when to apply RCM analytics to go from analysis to action faster.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock

Nasdaq notifies Veradigm that the company remains non-compliant with its listing requirements and faces de-listing for its failure to file its FY2022 and Q1/Q2 financial reports, which the company blames on software it implemented to meet new accounting standards. Veradigm says it hopes to file the reports before the 180-day exception period ends on September 18, but can’t guarantee it.
A good article in Behavioral Health Business reviews the digital therapeutics market following the bankruptcy of substance abuse app vendor Pear Therapeutics:
- Insurers are reluctant to pay for digital therapeutics products, although state Medicaid plans and the VA have been more active in covering them.
- Those Medicaid programs are concerned that other companies will follow Pear’s example in failing to stick around long enough to deliver value.
- Programs that require provider workflow changes and education are less likely to succeed.
- Companies are trying to establish a foothold with employers instead of treating their offering as a pharmacy benefit.
- Insurers are particularly reluctant to pay for software-only products, so companies are expanding to bundle coaching and clinical oversight as a virtual-first service.
Sales
- West Tennessee Healthcare engages Nordic to support its transition from Oracle Health to Epic.
Announcements and Implementations

London-based virtual hospital startup Doccla, which works with NHS, acquires remote patient monitoring platform vendor Open TeleHealth to expand into nine additional countries in Europe.
MUSC Health Orangeburg will go live on Epic on December 7, replacing Oracle Health.
Other
Epic UGM runs Monday through Wednesday this week. I always appreciate getting attendee reports. Verona is under a heat advisory (isn’t everybody), with highs Sunday through Wednesday of 92, 85, 95, and 95 versus barely 80 degrees last year. Cling to those memories of huddling by the first-night’s campfire in the crisp air, but at least be glad it’s not on Thursday, when the high will hit 100 degrees.
Sponsor Updates
- EClinicalWorks releases a new customer success story, “How healow Self-Scheduling Helped a New Practice Fill 400 Appointment Slots.”
- SeamlessMD’s Digital Patient Podcast features Meditech EVP and COO Helen Waters.
- NTT Data becomes a Microsoft Global System Integrator partner.
- Ronin publishes a new whitepaper, “Clinician Experience: The Missing Link Between High-Efficiency and High-Tech Healthcare.”
- Visage Imaging posts a case study titled “Optimizing Enterprise Imaging in the Cloud Using Visage 7 PACS Platform on AWS with Allina Health.”
- Sectra announces that a US-based health system will expand its use of the company’s technology to include the Sectra One Cloud enterprise imaging cloud subscription service for diagnostic imaging.
- Verato will exhibit at the Civitas 2023 Annual Conference August 21-23 in Maryland.
- Waystar will exhibit at the HFMA North Carolina HFMA Summer Conference August 23-25 in Myrtle Beach, SC.
- Wolters Kluwer Health will present at Rise West 2023 August 29 in Dallas.
Blog Posts
- How Meditech is driving AI innovations in health IT (Meditech)
- Amplifying Success: Integration Drives Positive Patient Experience (NeuroFlow)
- Lights Out: Defeat Digital Darkness (Optimum Healthcare IT)
- How Integrated Is Your Omnichannel Strategy? Here’s a Quick Guide (OptimizeRx)
- How Better Communication Improves Revenue Cycle Management (PMD)
- Leapfrog Rapid Response: Interventions to Improve Your Healthcare Ratings (ReMedi Health Solutions)
- IOT Sensing-as-a-Service Enriches Hospital Food Service (SmartSense by Digi)
- What Is the CMS GUIDE Model: A Paradigm Shift in Dementia Care (Trualta)
- Healthcare Transformation Series: Why Incorporating Digital Mental Health Solutions Makes Sense (Zynx Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.







































Today's post contains the phoenixes rising from the ashes of the post COVID telehealth era. There's two things that destroy…