EPtalk by Dr. Jayne 11/9/23
Several readers messaged me trying to get my thoughts on exactly which companies I think might be “in bad shape” following my recent discussion of the Olive shutdown.
The short answer is that a lady never tells, but readers didn’t even have to wait a day to see a non-healthcare answer, as WeWork filed for bankruptcy. The company had a pre-COVID valuation of $47 billion and has had to cope with the upheaval that the pandemic brought to the office-sharing and remote work space. Now there are questions as to how the company’s bankruptcy will impact the commercial real estate market, since the company had billions of dollars in lease agreements, including those for seven million square feet of office space in New York City alone.
One reader sent me the recent Block (formerly Square) shareholder letter, which mentions that they will cap employment at 12,000 people “until we feel the growth of the business has meaningfully outpaced the growth of the company.” They went on to say, “We know the inverse is true today.” A quick web search indicates that the company has about 1,000 more employees than that cap, so I hope they have the foresight to buff up their resumes.
As a public company, Block is required to release certain information and there’s the potential for shareholders to hold the company’s leadership accountable for performance. Block’s futures are closely tied to the retail economy, so it will be interesting to see what happens over coming months given the current state of things in the US.
Speaking of post-COVID challenges, a couple of my colleagues who are infectious disease specialists brought to my attention that the Centers for Disease Control and Prevention is working on an update to its Isolation Precautions Guidance, last updated in 2007. The newest document isn’t due to be complete for several more months, but a draft was finalized last week. It recommends that masks be worn to reduce respiratory pathogens such as influenza and COVID-19, but the mentioned masks are medical masks or surgical masks that aren’t as good at preventing transmission as N95 and other respirators. There’s great concern among physician and nursing leaders that the relatively weak recommendations will allow hospitals to go for the cheapest option rather than making sure that employees are adequately protected.
There’s a lot of discussion about burnout and turnover among frontline clinicians. I would offer a suggestion that one way to make employees feel more valued and appreciated would be to provide higher-level protection to anyone who wants it, without making them jump through hoops or reuse personal protective equipment which has already been anecdotally reported this respiratory season. I’ll take a giant pack of N95s or KN95s over a pizza party any day.
I had a lot going on at the end of October, so I missed the fact that the Federal Communications Commission (FCC) voted to begin the process of restoring net neutrality regulations that would keep US internet providers from slowing down services on their networks based on content. As expected, broadband providers plan to fight the effort, claiming that it is burdensome and that the effort is a regulatory overreach by the FCC. Public comments on the proposed rule are open and the earliest we’ll see a potential change would be 2024. If you’re looking for some scintillating bedtime reading, the Notice of Proposed Rulemaking and a fact sheet are available for your perusal.
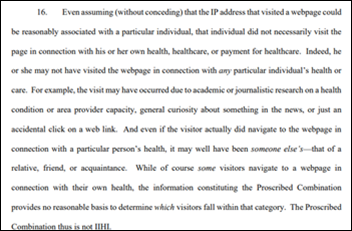
Also in my October mail bag was an overview of a new proposed rule that details “disincentives” for information blocking that was recently published by the US Department of health and Human Services. The proposed penalties include losing “meaningful user” status in a given EHR reporting period, which leads to economic penalties; receiving a zero score for Promoting Interoperability under the Merit-based Incentive Payment System (MIPS); and restrictions on participating in the Medicare Shared Savings Program. The proposed rule also describes the process to occur when an organization is accused of information blocking.
It still baffles me that organizations are struggling to get on board with this, since in the vast majority of situations, having greater access to patient data benefits patients and clinicians. I understand the financial ramifications and the desire for organizations to want to restrict competition, but it just comes off as being anti-patient at this point. Physicians in my area are happy to name and shame when organizations do it, and I’ve seen those revelations steer referral patterns away from uncooperative organizations. More information can be found on the related HealthITbuzz blog.

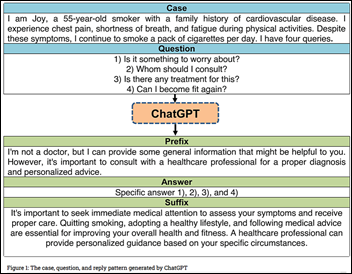
I recently became aware of a new startup that is working to mitigate how often artificial intelligence systems hallucinate or make up information. Vectara has about 30 employees and has raised $28 million in seed funding. Its founders include former Google AI researchers with deep expertise in the field. The company cites the rate of hallucination by AI platforms as ranging from 3% (OpenAI) to 27% (Google’s Palm chat). Meta’s systems rang in at 5%. The company plan to offer solutions that will mitigate the risks of hallucination, bias, and copyright infringement. Putting on my marketing hat, I like their logo, which feels clean and has forward mobility, and the use of color just kind of grabbed me. Including such a spectrum definitely reduces the need for people to debate which Pantone color is the “right” one.
A reader also asked me what I thought about the recent news that Cigna is considering an option to jettison its Medicare Advantage business. Perhaps Cigna has figured out, as have others, that it’s becoming harder to make a buck in the Medicare Advantage space while keeping patients happy and avoiding pressure on physicians and providers to overstate patients’ complexity. Medicare Advantage only comprises 4% of the company’s external revenue, so it makes sense for leaders to consider bringing in some cash so the company can focus its efforts elsewhere. There’s also the tidbit where Cigna is paying over $170 million to settle claims about its previous track record of trying to make patients seem sicker than they really are. As I re-enroll with insurance plans, I’m avoiding Medicare Advantage because the rewards don’t seem to be worth the administrative headaches.
Is your organization doubling down on Medicare Advantage or have they decided to pursue other interests? Leave a comment or email me.

Email Dr. Jayne.










































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en