News 9/27/24
Top News
Graybill, a California-based primary care group, will split from Palomar Health Medical Group, citing that organization’s inadequate support following an April 2024 cyberattack that took systems offline for months.
Palomar disputes Graybill’s claim that some of its systems are not yet fully recovered. It also suggests that Graybill shares responsibility, noting that a Graybill physician serves as Palomar Health Medical Group CMIO.
San Diego-based Arch Health Medical Group and Graybill Medical Group joined Palomar Health to create the 170-physician Palomar Health Medical Group in November 2020.
Reader Comments
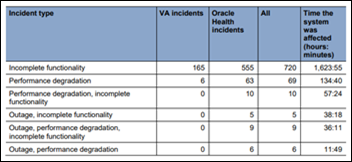
From A Frustrated Vet: “Re: VA. Happening as I write this on the House VA Technology Modernization Subcommittee: ‘Our veterans would have been much better served if the VA had not abandoned the Medical Appointment Scheduling System (MASS) in 2019. This project had implemented Epic’s scheduling system and patient portal in Columbus, Ohio, and they were working well. But the VA leaders at the time made a special effort to eliminate it, paving the way for Cerner to duplicate the work and install an inferior system. This was a disastrous decision that we are all still paying for.’ – Chairman Rosendale (R-Mont.)” Thanks. I will recap more fully in the weekend’s news once the hearing is finished.
HIStalk Announcements and Requests
Conference season is the ideal time to become an HIStalk sponsor and get year-round exposure to decision-makers instead of betting the farm on a booth rental. Lorre is likely offering incentives for new sponsors, startups, and former sponsors who return to my little fold, although she will also ensure that current sponsors, some of whom have supported me for more than a decade, don’t get shortchanged. Also for sponsors, if your company is attending HLTH 2024 in any capacity, send me your info soon to be featured in my online guide.
One last housekeeping item: hair-trigger spam filters always inappropriately unsubscribe readers from my spam-free update list. Drop your email here to stay in the loop—you won’t get duplicate emails regardless.
I got the ChatGPT update today with Advanced Voice Mode. It’s cool, though not revolutionary—it allows for natural voice conversations, pauses if interrupted, and adjusts its responses based on what you say. It’s fun that you can choose a voice with a personality that affects tone and word choice. Advanced Voice makes Alexa, Google Assistant, and Siri seem even more primitive, and it’s convenient to interact with ChatGPT via voice. The microphone stays open until you turn it off, so my phone sits beside my keyboard, ready to respond without requiring a wake word or key press.

I politely declined the interview invitation of Kat McDavitt, Lisa Bari, and Melissa Denino, the boundless energy folks who are behind the “Health Tech Talk Show.” Reasons for no-ing: (a) I avoid the spotlight like a vampire shuns sun; and (b) I say everything I know right here and don’t see the value of repeating myself. Still, I offered to help them feed the content beast by inviting potential interviewees to email them at hello@healthtechtalkshow.com. It’s refreshing not to need to stab the eject button seconds-in on a host who is long on self-importance but short on industry knowledge and a compelling style.
Webinars
October 24 (Thursday) noon ET. “Preparing for HTI-2 Compliance: What EHR and Health IT Vendors Need to Know.” Sponsor: DrFirst. Presenters: Nick Barger, PharmD, VP of product, DrFirst; Tyler Higgins, senior director of product management, DrFirst. Failure to meet ASTP’s mandatory HTI-2 certification and compliance standards could impose financial consequences on clients. The presenters will discuss the content and timelines of this key policy update, which includes NCPDP Script upgrades, mandatory support for electronic prior authorization, and real-time prescription benefit. They will offer insight into the impact on “Base EHR” qualifications and provide practical advice on aligning development roadmaps with these changes.
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
India-based Qure.ai completes a $65 million Series D funding round to expand into the US market and to pursue acquisitions.
Sales
- UAB Health System will implement Epic as its single EHR in a seven-year, $380 million project, replacing Oracle Health.
- ChristianaCare will implement Epic, replacing Oracle Health.
- Children’s Hospital of Orange County will deploy Oneview Healthcare’s Care Experience Platform on patient room TVs.
People

Susan Worthy (Amwell) joins Gainwell Technologies as chief marketing officer.

Former Cerner executive Maria Flynn, MBA, MS is named president and CEO of the Patterson Family Foundation, a $1.5 billion asset non-profit that focuses on rural health and was founded by Cerner founder Neal Patterson and his wife Jeanne, both deceased. She was also co-founder of Digital Health KC.
Announcements and Implementations
Cobb County, GA joins the Find Help social network to launch an online resource that connects residents with assistance programs.

Sonifi Health integrates NESA’s Epic-integrated virtual care system with its patient room TVs.

Meditech kicks off its annual customer leadership conference in Foxborough, MA.
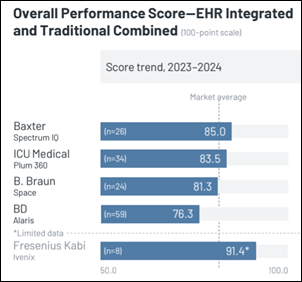
A new KLAS report on smart IV pumps finds that BD Alaris recalls and the FDA’s approval of next-generation technology are driving earlier replacement and expansion decisions. EHR integration is the most important factor in purchasing, usage, and satisfaction, followed by cost and ease of use.
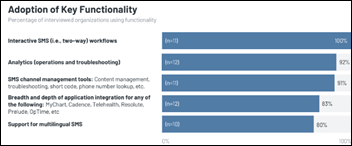
KLAS also takes an initial look at Epic’s Hello World integrated SMS messaging system. All interviewed organizations are satisfied, would recommend it, and would buy it again. Customers say it reduces appointment no-shows using reminders, speeds communication with patients, and is deployed via MyChart.
Government and Politics
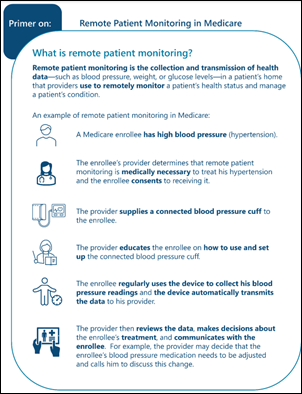
HHS OIG finds that the use of remote patient monitoring for Medicare patients has increased dramatically, but needs additional oversight to prevent fraud as patients are not always receiving all required services and Medicare lacks the information to oversee its use. CMS agrees with OIG’s recommendations: (a) require a provider’s order for RPM that is included on claims and encounter data; (b) develop ways to identify the health data that providers say they are monitoring; (c) educate providers about billing for remote patient monitoring; and (d) identify and monitor those companies that are billing for RPM. OIG says that 43% of Medicare enrollees did not receive all three mandatory RPM components: education and device setup, collection of an adequate number of device readings, and use of the data to manage treatment.

The Senate unanimously votes to hold Steward Health Care CEO Ralph de la Torre, MD in contempt of Congress for ignoring its subpoena to answer questions about his compensation as the bankrupt company’s hospitals struggled to deliver safe, effective care. A spokesperson for de la Torre says that he has the right to not answer questions under the Fifth Amendment and won’t be intimidated by Congress. He faces prison time as the first person to be held in contempt by the Senate since 1971.
Other
Allina physicians report problems that were caused by order entry confusion resulting from the health system’s switch of in-house outpatient lab work to Quest Diagnostics last week.
I truly enjoy reading the “Hey Judy” posts on Epic Share, where she has written these ruminations for September:
- She paid her 15-year-old son – who wrote contest-winning computer games from their home basement where Judy was working on Epic — $5 to develop a programmer test after hiring Epic’s first programmer and then realizing that people aren’t always as talented as they think. Epic used that test for 18 years to choose new employees, then expanded the question bank when they leaked out.
- She describes the origins of Share Everywhere, which Dave Furhmann created (he’s now SVP of R&D) after Judy learned that Cerner hospitals couldn’t exchange information with each other.
Sponsor Updates
- Black Book Research ranks Inovalon #1 in its 2024 provider enterprise RCM analytics solutions survey, with top ratings across 12 KPIs.\
- A new KeyCare survey of 400 patients finds that the majority prefer telehealth to office visits for medical issues including urgent care, preventive care, chronic care, and specialty services.
- Black Book Research publishes the results of its 2024 supply chain customer experience survey, with Dimensional Insight taking the top spot for benchmarking and comparative analytics.
- Inovalon promotes Sandy Warford to director of product marketing.
- Five9 and Verint expand their partnership to deliver AI-driven customer experiences.
- Fortified Health Security will present and Healthcare IT Leaders will sponsor the Georgia HIMSS Conference October 1 in Atlanta.
- Linus Health unveils new tools for early dementia detection at AAFP’s FMX 2024 conference.
- Meditech customer Ontario Shores Centre for Mental Health Sciences becomes the first hospital in Canada to implement Expanse Genomics.
- MRO will exhibit at the Medical Practice Excellence: Leaders Conference October 6-9 in Denver.
Blog Posts
- Healthcare’s Current State vs Perfection: Which is Best? (Vyne Medical)
- Revenue Cycle Management: Boosting Operational Efficiency and Productivity (EClinicalWorks)
- Addressing Healthcare Staff Satisfaction through Innovation and Support (FinThrive)
- A year of DAX Copilot: Healthcare innovation that refocuses on the clinician-patient connection (Microsoft)
- Embracing Generative AI as a Change Agent to Drive Clinical and Financial Value (Impact Advisors)
- Maximizing ROI on IT Required by CMS Rule 0057 Takes a Village (InterSystems)
- Solving Quality Issues in Healthcare Data: KONZA’s Leadership in NCQA DAV Accreditation (Konza National Network)
- NAFLD Guidelines: A Shift in Understanding & Focus (Lucem Health)
- Your Guide to HTI-1 (Medhost)
- Why We Need Proactive Technology And Human Collaboration To Combat Medicare Fraud (Medicomp Systems)
- One year in: How Suki and Meditech are transforming clinician workflows with voice AI capabilities (Meditech)
- Med Tech Solutions Broadens EHR Support Expertise (Med Tech Solutions)
- Hospital Physical Therapy: Empowering Patients Toward a Safe Transition Home (Net Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



























This is a great point—many discussions about patient wait times still focus on staffing or technology, while the real issue…