J. Erin Hutchinson, MA is owner of Narrative Shift of Herbster, WI.

Tell me about yourself and the company.
I’m a Midwestern farm girl, so I don’t like to talk about myself, as most of us don’t. I’ve spent my career starting companies, starting with clothing stores and video store chains. I have 45 years’ of experience in the healthcare technology world. Ten years ago, after launching many small ventures, I started what is now Narrative Shift.
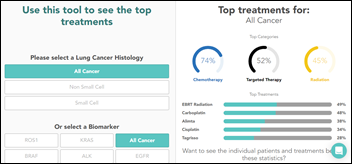
We help founder-led companies and startups in the healthcare and biotech space successfully launch their products and services. We help them craft compelling narrative to create curiosity and excitement among their target customers so that they are interested in having a conversation. All of us are bombarded with lots of shiny marketing stuff, but it’s hard to get your message out there so that people take action and have that initial sales conversation. We do full-service graphic design, marketing, and go-to-market strategy. It’s a startup advisor in a box, as I like to say.
You went from being a psychologist to leading teams at Epic, engineering companies, and consulting firms. How have you applied your psychology knowledge in those roles?
I worked for Epic back when it was fewer than 100 people. In my late 20s, I was working with physicians and surgeons who were new to technology, to the point that I had to teach them how to turn on a computer and use a mouse. A surgeon threw a keyboard at my head once, so that’s when I used my clinical psychology skill set to get people to change.
In helping new companies get launched and bringing more revenue to tech startups, I draw from that background of how we communicate and connect with other people. Companies tend to get myopic. They may have the best thing since sliced bread, but they lose track of being able to put themselves in their customer’s place. I help these companies craft their identity and craft their story so that it is communicated and connects with their target audience.
Tech people are not always the best at the human element, so my background has helped a lot. Plus I was a child and adolescent psychologist where humor is important, especially when you are working with young kids. I bring that to my work with my clients. Starting and growing a company is hard work and I like to bring a little bit of fun to that.
What is narrative therapy?
I was trained in, and my dissertation was in, using the narrative approach in working with children and adolescents. I could bore anyone to tears with all of the heavy post-modern theory aspect of narrative therapy, but in essence, it’s that we as humans create meaning and communicate with each other through through narrative, through stories. That is the core element of how we express our experience. The essence of successful design and marketing is that you have to communicate to your customer through a story.
Bringing the narrative therapy approach involves working with your clients to understand the narratives that shape their world view, and then working with them to re-author those in the way that they see themselves. Maybe they can re-author their narratives to psychologically shift their perspective.
Founders are usually interesting and have a lot of personality and humor, but they seem to be coached into dullness as their companies grow, to the point that all communication is filtered through conference rooms pull of people who suck the life out of it. Can large companies be interesting and fun?
To be 100% transparent — and sometimes I’m painfully so — one benefit of owning a company is that you can choose to be that way. I choose not to work with many large, established companies. They are either overly prescriptive about “this is how we must present ourselves” or they have armies of corporate marketing people who are maybe good at putting on events, but not so great in figuring out better ways of connecting with their customers.
We in healthcare are do a really bad job of using creative ways to get the interest of target customers and target markets. I set a rule with clients that if they want shiny, happy stock photos of people who look like doctors and nurses, then they need to find a different agency to work with. I generally shy away from those companies that grow and become the Borg.
Early-stage or founder-led companies, which more often maintain that entrepreneurial culture, are more open to being creative and asking for help to find their voice, establish their identity, and craft the narratives that will get prospects interested. I’m probably trying too hard to be politically correct in saying that big companies are boring. Those that grow successfully need to maintain that fine line, but cut through the noise by being a little bit irreverent and not being afraid to try something different in their marketing. It’s easier to do that if you have strong leaders who maintain that entrepreneurial spirit and don’t hire a bunch of marketing Borgs or large agencies without experience in healthcare or healthcare tech, which perpetuates this culture of stock photo websites and material and messaging that all looks the same.
How much do you help create strategy rather than just communicate it?
It’s a little bit of both. I love working with smaller companies and startups because I’ve been in the role of starting companies. I’ve been a part of many ground-floor new ventures. I’ve done the work. I didn’t just get a marketing or design degree. I’ve gone through the process of getting funding and I know what that takes.
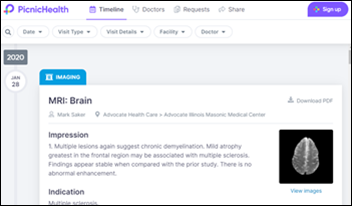
With my background as a therapist, many clients ask for help because they hate their website or their sales pipeline isn’t growing. But most of the time, that ends up turning into a combination of helping to craft the strategy, especially from a go-to-market perspective, as well as the messaging and those narratives. I find it impossible to separate those two. Maybe it’s because I’m opinionated, honest, and open that I can’t hold back, so I give my advice and clients can take it or leave it. I can’t just churn out stuff that looks pretty and sounds good. If I can help someone with their strategy and to be more successful in growing their company, I’m going to do that.
Because of my background and being one of the few firms out there that specializes in the provider market, they don’t have to spoon feed me and educate me on their business and their customers. I know it. That also helps me to be more strategic and holistic in the work that I do with my clients. It also means they don’t have to go through the agonizing process of writing a lot of copy for me to clean up because I can already articulate what is needed to their customers.
Social media tech companies have embraced psychology in ways that aren’t entirely positive, getting people to keep coming back, pushing analytics-targeted ads, and entertaining them with short videos. Does that change the way that companies might get and keep the attention of prospects?
Because of the evolution of media and how people consume information, there’s no longer a standard recipe of what will work for a particular type of company or customer. I tell clients that some things aren’t worth wasting your time on. You aren’t going to get a hospital CEO to call you just because you have a great Twitter feed. Some clients I’ve worked with think a social media presence will magically result in more customers.
I wish that the diversification of media and expansion of the ways people get information make it easier to grow your company and to get the attention of your customers, but frankly, it has made it a lot harder. You have to spend more time understanding who they are, developing your buyer personas, and then figuring out where they are. What are they looking at? How do you get in front of them and get their attention? You need to have a multi-pronged approach. We no longer have four TV channels, three radio stations, and two newspapers.
It goes back to psychology understanding. What do you have to offer? What is your secret sauce? What makes you special? Whose attention are you trying to get? The psychology component gets infused into figuring out which tools to leverage and crafting campaigns and materials that are targeted at these types of potential customers. That was simpler before social media.
Some companies based their entire marketing strategy around the HIMSS conference, then reaped whatever benefit they received for a whole year. How will that change in the absence of in-person conferences for now and with provider customers whose priorities are dramatically different than they were six months ago?
I’ll be blunt. If there is one upside to the pandemic that we’re living in, it’s that it upended the HIMSS apple cart. My guidance to clients for at least the last five years is, don’t do it – don’t spend the majority of your marketing budget on this one event. Feedback from the last 10-15 companies that I’ve worked with, which has gotten louder over the last few years, is that they sunk a ton of money into HIMSS and got next to zero return, other than meeting a few new people. I’m hoping that this has forced companies to reevaluate and rethink their spending. I will be curious to see, by the end of this year or the middle of next year, if companies look back and realize that HIMSS didn’t really impact their bottom line that much, and they got good results using other methods.
Will that level the playing field so that small companies can use creativity rather than a big bank account and sprawling booth to chase business?
The benefit is that people have to think differently about getting their name out there and marketing themselves. The benefit of in-person conferences was getting face time in forcing your way in front of those most likely buyers. The companies that will succeed now will be creative and able to adapt. That’s harder for a large company that has entrenched corporate marketing departments and strategies, where it’s harder to adapt and be willing to diversify in trying different things and methods. Established, bigger companies put 75% of their marketing budget into HIMSS or other conferences. Now there’s the freedom to take that money and be more creative and use a variety of marketing campaigns.
Smaller players are relegated to the HIMSS “basement,” sometimes literally on the fringes of the big show floor. This is a time where it’s harder to get healthcare buyers to pay attention to you. They playing field is leveled if you are creative an willing to try different things. Your prospects aren’t getting the impression that since you don’t have a big booth, you’re not worth talking to.
I live in a very rural, isolated part of the country that relies on tourism. I’m involved in the local farming and arts communities. We have offered for 15 years a local artist studio tour, with hundreds of people visiting this tiny town of 100 people that I live in. We couldn’t do it this year because of the pandemic, so we pivoted to a virtual tour. We’ve had three times the traffic as we had last year, which had been our most-attended year. This has made made everybody think differently about how you can market and sell art and for artists to connect with potential buyers as well as just people who appreciate art. Corporate America and companies that sell into the provider market might be surprised by the amazing results they can see if they connect with people virtually.
What psychological observations do you have from working in 100-employee Epic now that it’s 10,000-employee Epic?
They have had to adapt some things as they have grown, but I’m not surprised that the company’s culture has remained consistent, since it is 100% driven by the founder. She has remained consistent in her perspective on how she wants the company to be portrayed, even in things like not wanting to get a bunch of “professional” marketers and designers.
Back in the day, I was one of the people producing the UGM multimedia presentations. It was all employees, and now they have people they pay to do that. But the company has always been proud of not devoting tons of time and resources to sales and slick marketing, and that has helped them continue that same kind of vibe. Going back to pure psychology, Judy established the narrative of what she wanted Epic to be early on and has not deviated much from that as the company has grown.
Some great case studies will be written in the next decade or so that Epic didn’t follow the rules of the road, but still scaled the company without growing up, maturing, and making everybody wear suits. People will look back and see that you can be true to yourself if you establish that really strong identity and strong narrative. You can grow and become the monolithic, 10,000-pound gorilla.
Do you have any final thoughts?
Everyone is struggling. 2020 has been a year that none of us could have expected. If you are struggling, like we all are, this is a great time to reevaluate and take a look at how you are communicating and defining the story you want to tell. Think about trying something different, because honestly, what’s it going to hurt? The rules have been broken by the fact that we are living in a completely new reality. Have fun with that a little bit.
Comments Off on HIStalk Interviews J. Erin Hutchinson, Owner, Narrative Shift












































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…