Scott Finfer is co-founder, CEO, and board chair of Emerge of Dallas, TX.

Tell me about yourself and the company.
I’m CEO of Emerge. We offer a solution set that can overlay on top of EHRs. The strength of our company is our people, a unique group that has come together.
How common is it for EHRs to offer a search function and how is it used?
Search can mean different things to different people. In the world of Emerge, when we talk about search and when we talk about what our mission is, it is searching not only the data that exists inside of the EHR that is discrete and accessible, but also information that isn’t necessarily searchable by the EHR unless they are using optical character recognition and natural language processing to use scanned and free text information.
But more importantly, when we talk about search, we stay patient centric. If I search for information about a patient and I’m at an ambulatory facility, in an ideal world, I should be able to have their records available to me if I need to treat that patient inside of the acute world. We’ve made our life’s mission to figure out how that search is not just about searching in records that exist — that’s the easy part — but searching for all the possibilities of where we can bring this information together on a master patient index to have one patient file that can theoretically travel with the patient wherever they go.
Does it make clinicians more efficient or allow them to find the most important information more easily?
I got stuck in healthcare. I’ll be honest about that. I didn’t realize how incredibly difficult the space was. I came out of IT services. Before that, I was doing real estate. I’ve made tons of money doing everything I’ve ever done, but I’ve spent tons of money over the past 10 years to build this business up, because healthcare is way harder than we expected.
But the good thing is that we now have the ability to understand what the problems are. We can document and have engineering problems versus, wow, it’s just not going to work. That’s a big difference. You can say, is it solvable? Well, maybe. Everything is potentially solvable. But what’s better than solvable is that it’s an engineering problem. If we do this, this and this, this allows for this to work.
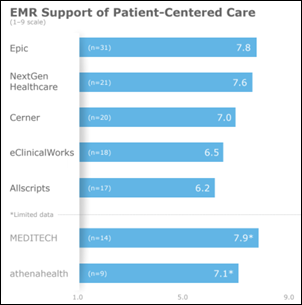
That’s where we are at this stage of development. The people in the country now – patients, administrators, forward thinkers, caregivers, providers –everybody keeps struggling with these friction points that exist that are self-made. One of the big friction points is that, what is the center of importance in healthcare? I would argue with you that it is often missed, because providers are the center of healthcare. The patient is the center of healthcare. This isn’t against any particular EHR, it’s against every EHR that provides acute services at a bare minimum. Why are the systems developed around hospital beds as opposed to patients? The whole thing is designed for something different than staying focused to patient care.
We have the problem now to fix all these silos. Then it’s compounded by the fact that, who is the best source? Is it one source or multiple sources? All these things are playing friction. The one thing that has never been delivered, regardless of what belief system you’re of — and I’m a no belief system here, I’m neutral, I just want to help healthcare — is that getting my record in and out and moved around and shared has been a disaster.
One of the reasons is because, most of the time, that’s a manual exercise that happens in the back office. People don’t think about this or don’t know this, but when there’s an official records request, it’s a money-losing proposition for the facility to have to go back through and figure out what the record is. Our technology, because it breaks everything down and starts with the patient at the center, says, I always have to keep it. Wherever it came from, I should break it down and bring it to the patient. That should always be the focus of whatever I’m doing for my flows of information.
When we encounter a situation where a health system is on multiple EHRs, we can come in and they don’t have to make any more investments. We can overlay on top of those systems and not only make them communicate with each other, but we can start to automate and provide smart services. Like, push a button and here’s your health record, because we can define what it is. I can get it for you. That’s what we have with ChartGo. With the push of a button, you’ve got the health record.
If it’s that easy to grab control of the health record with so much more granularity, now we can go to the big health system. We’re talking about big health system in California, and they want Northern California and Southern California to communicate with each other. But even more important than that, they want their patients, when they are traveling on holiday, to have easy access to their records and to share if needed wherever they are. That’s now possible because it’s being patient centric.
Is it difficult to access the information so you can create the overlay?
No. The most difficult thing in working with these facilities is the facilities themselves wanting to work with you. There’s this fear with some organizations about what is going on with the cloud. As you look at a lot of healthcare systems, it’s heavy steel. Man, it’s big money up front. For me, that’s fine. You don’t even have to change what you’re doing, but for pennies on the dollar, I can automatically make you 100% digital in the cloud. Your data, your control. Tell me where you want me to send it. That has never happened before. It has always been under the control of whoever sold you the operating system. We can help change operating systems, make them work better.
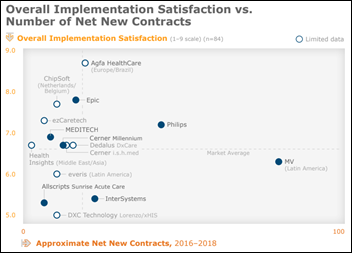
We’ve got a wonderful partnership going with a couple of EHRs right now, Athenahealth and Allscripts. Their senior leadership says out loud – which I’ve never heard someone say — we’re not the only thing. We’re part of the infrastructure. We’re part of the ecosystem. I said to myself, wow, they get it. There’s not going to be one — it’s not going to work. It’s got to be able to work together. Part of working together is knowing that some people might be great EHRs and some people might be great this or great that, but at the end of the day, what is needed is glue to make them work nicely together. Forward-thinking people, and there’s a lot of them, recognize that this is an ecosystem play. That’s where we are headed.
We know how to operate in any ecosystem because we speak all languages. Doesn’t matter which EHR, doesn’t matter the versioning, doesn’t matter the age of the technology. Our guys are utilizing state of the art technology and there’s no lift on the back end. I come to you and I say, let me solve your problem for you. The facility says, what’s it going to cost? Nothing. OK, and what kind of resources do I need to provide for you to do that? None. They look at it and they go, it’s not possible.
After surviving being told that for 10 years, we now have successful investment bank software company. The most important part about it is that we did it with our own money, and now it’s making enough money to stand on its own two feet with no venture capital in the deal. We did it to solve healthcare problem because my co-founder, who is a doctor – cardiologist William C. Daniel, MD, MBA — is a humble enough guy to understand that when you’re treating patients as a cardiologist, there’s plumbers and there’s electricians. I love this guy. I’ve known him since I’m 13 years old. I wouldn’t have gotten into this business if it wasn’t for him.
What he said to me was, I’m killing people. I said, what? I’ve never heard a doctor say that before to me. He said, I’m 100% killing people. I know I am. I just can’t prove it. I’m seeing people in my office who are coming to see me because I’m a plumber. I don’t know electricity all the way through the detail. There’s stuff going on that if the EHR record was scrubbed, I would know that this guy needs to see an electrician, and I would get them to the electrician. That’s how this whole idea came up.
ONC pushed EHR vendors years ago to make it easier for users to export patient data from one EHR that could be imported into a different EHR, making switching easier. Has that gotten any better?
There’s no lift. Zero. We literally have converted over 100 different brands of EHR into the systems of our trade partners. They are left with non-usable data most of the time coming out of whatever EHR they’re coming from. Athenahealth is a partner of ours and one of our prime relationships. When Athena signs up a new customer, Athena brings us to meet the customer, because the customer can literally have everything waiting for them inside of Athena. They have access to not only to their old data, they have access to 300% more of their old data.
But that’s not even the big kicker.They didn’t have to do anything. They turn on Athena’s state of the art system in the cloud, and it’s set up and ready to run. All of a sudden, both the old information and the new information through Athena are able to merge together as they see new patients through Emerge on a go-forward basis. They are always getting the full context view. If we need to add on other feeds from other EHRs, HIE, or API to allow somebody else to pump in a third-party data from a payer, all those things are now possible. That’s what we are building with Allscripts and Athena.
What does it take to sign new partners?
I don’t think you have to sign on new partners. I had a wonderful client and mentor in Oklahoma named John Harvey. He told me that he took a chance on us. He brought us up to the Oklahoma Heart Hospital early on, even before we really had a product. That’s the truth. We thought we had a product, but we didn’t realize what a problem there was in the space. John brought us up there and we were doing great stuff. We were going after every EHR back then. We were going to try and integrate with everybody.
John said, if you boil the ocean, you’re going to die. You had better pick one and try and make it work. Then if you can make it work in one, you can make it work in all of them.
That’s exactly what we did. Now we are in four of them — Epic, Cerner, Allscripts, and Athena. When I say having to get a partnership, I’d love to do a partnership with Epic if they want to do one with me. I can save millions of dollars in conversions for anybody switching to Epic. To bring their database from their old system to the new system will cost them $25,000. I mean, this is the digital age, so I have a digital solution. A lot of people are beginning to embrace it, and things are going to change rapidly. But the most important thing is that it works, it’s patient centric, and it’s following how medicine is supposed to work.
What is the direction of the company going forward?
We see ourselves following the same footprint that we started 10 years ago. A lot of companies set out to solve problems, and then they bring the solution to market. They say to the doctors, nurses, providers, staff, administrators, or the quality people –if you would only use my tool how I designed it, it would work for you. There’s a problem with using my tool as I designed it to work for you, and that is workflow. Part of our strategy has always been to make sure that we are directly in the workflow, but not in the way.
We have done that now with over 100 installs. You could literally take our install list and pick anybody on it and ask for a referral and they’ll give you one, a good one. Everybody’s happy. We have this massive retention rate because we’re in the workflow. That is key for where I see ourselves as we move forward.
Our roadmap for the past 10 years was written by my customers. With my subscription model, somebody says to me, I wish I could track proteins on these pregnant women that are coming in from all these facilities. We say, we can help you with that, and we do that for them. Then we turn around to any other OB-GYN who has a subscription with us and we give them that same functionality if they want it. Our subscription gets stronger and stronger, and what we are doing gets stronger and stronger.
We are much much more than search at this point. That’s a small underpinning of what the company is really doing. One of our strengths is the downtime viewer. If your EHR goes down, you can log in through our portal and have a digital version of everything available through our search tools, to be able to search the record while you’re in downtime. We have population health tools that don’t require an SQL search. You don’t need to spend millions of dollars to have a consultant come do this. Tell us what you want. I want to find all the patients that have not had a colonoscopy in the past 10 years and that do not have an appointment scheduled. Give me that list. Oh my God, 10,000 people that should be getting this procedure done. That’s 10,000 times whatever the cost of a colonoscopy is, $1,000, massive revenue from the existing population. And if they don’t do that, the cost of care is going to go up.
We are getting proactive, making sure that we’re hitting large target parts of the marketplace all at the same time. We have a way to find them. More importantly, we have a reverse delivery message available. If you miss something on coding and the only place where it’s appropriate to code like that is between the patient and the doctor at the point of care, it has to be done at that point. I’m inside the EHR and I have dashboards to use it in their workflow. If there is something that that doctor needs to code, adjust, or to change because the customer can now be paid for the work that the doctor’s already done, it’s a very efficient way to put it in the workflow. It can even get caught before the doctor does it, because we’re using our automated tools for the chart prepping process. We can chart for up an entire facility with a push of a button.
I don’t know exactly where it will be 10 years from now, but we’re going to do the same thing that we’re doing, which is, show us the problem, give us your requirements, let us solve it, and help us make our subscription stronger with each new member.





































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…