Mike Linnert, MBA is founder and CEO of Actium Health (formerly known as SymphonyRM) of Palo Alto, CA.

Tell me about yourself and the company.
Actium Health helps health systems and payers with CRM intelligence. We take all the data they have about their members and identify “next best actions” to drive lifetime value for the members. Before founding Actium Health, I grew up doing similar things for companies in the wireless and financial services industries, and before that, I was investing in consumer internet companies.
What could “next best action” look like for me as an individual consumer, both inside and outside healthcare?
Starting outside healthcare, the goal is to drive lifetime value for a customer relationship. Some “next best actions” don’t have revenue or profit associated with them in the near term, but their investment is in the long-term relationship.
I’ll give you some of the simplest ones I started with. When I was in the wireless industry way back in the early 2000s, you might have called the call center with a question about your bill. While we had you, we might have observed that last month you could have saved $3 had you been on the 100-messages plan instead of the 50-messages plan. You as a consumer would think, “Great! That’s great,” and we as the wireless provider would feel like, “We helped you save some money, but also we probably encouraged you to do more texting, which is something that we wanted you to do anyway because it attaches you to your device more.” Things that you liked about our service, and in the long run, we probably decreased your propensity to churn. And if we increased your usage of text messaging, we hopefully increased the value that you saw from us.
As you get more complex, you can think about perhaps your wealth advisor at your bank. At any given time, your wealth advisor might know that you forgot to make your 529 education contribution for one of your kids, you didn’t make an IRA contribution this year, you haven’t rebalanced your portfolio, or mortgage rates have gone down and you could potentially refinance your mortgage and save some money. The ”next best action” involves which of those things is most valuable to you. I’m a wealth advisor, so my job is to stand by you, not to stand by the products and broadcast out to you, “Hey, this product fits you.” I stand by you, you tell me about your needs, and then I say, “Here’s the most important thing. I know your kids are important to you. If we only have five minutes to talk today, let me focus on the 529 plan.” But to do that, I have to come up with what the most valuable thing is for you. We bring AI to do that on behalf of the wealth advisor or the health advisors here in healthcare.
Is it uncomfortable for providers to think of the lifetime value of a given patient and to reach out to them to offer more services, either to bring in more revenue, to benefit the patient, or both?
It shouldn’t be. The goal is to drive the lifetime value of the relationship. If I ever slammed you products you don’t need, I should assume that you’re going to turn and go somewhere else. Maybe there’s some near-term profit, but over the long run, you’re not going to be with me any more. You’re going to find somebody who takes care of your needs better.
In the financial services example I gave, the goal was to say, “What is most valuable to you and to our relationship?” In healthcare, let’s assume that I’m on a value-based care model with my local health system. The health system knows that I’m past due for a colonoscopy, and maybe they know that I haven’t seen a primary care doc in the last three years. Maybe from looking at their data, they suspect I’m high probability for having kidney disease and don’t know it.
At least for me as a patient, I would love it if the health system didn’t worry about whether they were violating the revenue goal, or violating something about our relationship, and instead felt a moral imperative to reach out and tell me, “Hey Mike, based on the data we have, we think it’s worth you taking this health risk assessment for kidney disease” or “here are the top three reasons that you should come in and see your primary care doc.” I would like them to be reaching out.
Certainly what I don’t want, and what would be violation of HIPAA marketing, is for them to be hawking drugs that may or may not fit me, or to let me know that they have a new partnership with a local imaging center and I should consider going there. Those aren’t the things I want. But I do want things that help drive health for me and my family.
Some patients, especially younger ones, don’t necessarily see the value of ongoing engagement with a health system or primary care physician. How do providers convince them of the value of that engagement or use “next best actions” to address their needs?
You have to step back and, again, talk about what drives lifetime value. Your point is exactly right. What drives lifetime value for my dad in the health system is very different from what drives lifetime value for my son in the health system. My dad wants to know that the health system is proactively thinking about him, looking at the data they have about him, and proactively reaching out to engage him. My son wants to know that they are there if he needs them, so maybe they let them know that he can schedule through text messages or which simple conditions could be managed at urgent care at a lower cost and shorter wait time than the ER.
You have to think about what these things are for each cohort. That is the whole point of the “next best actions” approach. We are developing one-to-one dialogues that for each customer, think uniquely about the things that we have that can create value. I’m not trying to upsell and cross-sell so much as I’m trying to up-serve and cross-serve. If I serve you better, that will drive the loyalty.
I’ll give you a stat so you have a sense of why I think this is important. If I look at Verizon and AT&T, I might say it’s customer churn. I haven’t looked in a while, but last time I looked, it was around two to three percent. Two to three percent of their customers leave them each year. Health system churn, from our back of the envelope math, is between 20 and 30%. It is 10X. What we think we provide is a highly personalized, highly customized solution. You have to ask ourselves why that’s happening.
Healthcare switching costs might be lower than for changing cell providers, and some degree of unavoidable churn occurs because people change employers or their insurance changes. Some people also don’t need or have any provider interaction in a given year. Is healthcare different where they might come back to a provider when they need them or decide that someone else might address their problem more readily?
The difference between total churn and addressable churn is absolutely important. Someone may have moved away someone or switch to plans your physicians aren’t in. But that doesn’t put a big enough dent in the 10X difference that you would say, “This isn’t important to me.” For a lot of health systems, if you haven’t been in to see your primary care or other doctor in two to three years, they make you re-onboard. You have to go see a nurse again before you can see the doctor. We don’t want to do that.
We especially don’t want to do that for the younger generation you mentioned. We’re just helping them. They may not want to see a doctor for one to two years. But during those years, those patients have been thinking about their health. I saw a study that said that the average American spends 11 to 12 hours a month online reading about health information.During that time, I promise you that the people online who are giving them that health information — it could be Google, it could be other health websites — they want those members, patients, or customers as customers of theirs, too. People realized that the lifetime value of having a customer relationship centered on healthcare is very high.
The other big trend that’s happening right now is value-based care coming on scene. Value-based care is enabling a lot of competitors to build lucrative businesses around having deep customer relationships. In the old model of healthcare, to make a lot of money, you had to have a lot of specialists, because that’s where the money was. In value-based care, you can make a lot of money by keeping people healthy and having good, loyal relationships. You see people like One Medical, VillageMD, Walmart and CVS getting in and saying, “If there’s a new way to have consumer service-based relationships with patients and healthcare, that’s an opportunity.”
How does a health system run “next best action” programs for both their population health and marketing programs without confusing the consumer and making sure that each campaign’s messages are appropriate?
This is where you have the two-canoe problem, with fee-for-service and value-based care competing. But if you scratch a little deeper and look at individual contracts and different incentives, you probably have closer to a 200-canoe problem, with different people and different incentives. But that’s the whole point of the “next best action,” one-to-one dialogue approach. We want to figure out for everybody, what is the most valuable thing we can say to you based on what we know about you?
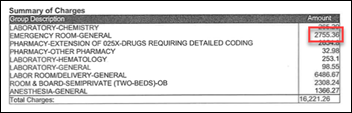
Let me give you an example of what the differences could look like. I’m going to give you some directional numbers that aren’t exactly correct. If I was a health system, I might ask, what is the value to me as the health system of bringing someone in for a breast cancer screening? Of course there’s value in that I am supporting my patients, but if I look at it on a dollar basis, I would say for every 100 screens I do, I’m going to do about 10 diagnostic follow-ups. I’m probably going to discover one case of cancer, and about half of those I’ll end up treating. Just ballpark numbers there.
For most health systems, if you did the expected value of the margin at each level there and multiplied them up, you’d get about $250. And if I get really good at predicting that women in this cohort are six times more likely than average, reaching out to those women and getting them in is potentially worth $1,500 to me, six times more than average. If I flip it around and ask the community, “What’s it worth if I reach out to you, invite you to come in, and we find that you have cancer and you weren’t otherwise going to come in?” it’s a lot. Because if you didn’t come in, that cancer was going to be much worse by the time we found it.
In a value-based care world, where I make money is by not finding cancer, or finding it so early so I stave off the later costs. That’s worth $250 for an average fee-for-service, but double that on a value-based care contract, closer to $500, to be doing those screenings to avoid the cost of finding later-stage cancer. That’s in addition to bonuses that I unlock or business value I unlock because I hit five stars on my screening, or because I met some threshold in a contract, and I’m able to market my Medicare Advantage plan differently. If you start to take all those into account, you start to realize that for health systems that are truly in value-based care models, there’s enormous value to proactively reach into the community and find people who have cancer and don’t know it. Or reaching into underserved communities and pulling people in that need care from us.
A survey written up on your website found that consumers perceive that their doctors and hospitals ignored them during the pandemic by not answering their phones or reaching out. What is the opportunity for health systems to move ahead from that?
I’m going to give you three quick examples. From January 2020 until now, our customers have increased proactive digital outreach by 10X, and I think there’s still another 10X to go. I think my health system should be reaching out to me at least once a month proactively with, “Here’s your family health income statement and balance sheet” or “Here are new services we have” or “Here are things you should know about what’s going on in the community.”
Second, I move around between health systems. Kaiser is not a customer of ours, but I’m going to mention something they did. During COVID at the peak, Kaiser was sending me three emails a month or even per week on some occasions. Three emails a week. And they were valuable, meaty emails. I liked reading them. They were telling me about positivity rates in my community. Stuff that I was really curious about and stuff that, had they not said it, I would have gone on Google. Kaiser was providing me a service.
The third thing is that last year, cancer diagnosis in the US was down by about half. We didn’t cure cancer last year. What did happen is that half of all the cancers that we probably would normally have discovered got worse. They went untreated, they went undiscovered. Health systems, to my way of thinking, have almost a moral imperative to be reaching out to people, to be looking through the data and saying, “Where are the communities that are most underserved? Who are the people that we think are at higher risk of breast cancer? How do we reach out to them and get them in for screening?” Most of those screenings are free. We have a free service that helps you discover and stave off cancer. That’s not to say anything about kidney disease and all the other diseases that went unaddressed faster that we need to get back to.
Where do you see the industry and the company in the next 3-4 years?
We’ve been talking for a long time that healthcare is a consumer service. If we are a consumer service, then there are some things that are fundamentally true, and you can look around at other consumer service industries. Most importantly, we need to stop thinking about patients as customers. We need to start thinking about people as members. Members have a recurring relationship with you. It’s enduring, it needs to be taken care of, and if you don’t, other people are going to come take your members. And if we have members, then we need to be thinking about how to drive value, delight, and loyalty among our members. Value means value they get from us, delight how happy they are, and loyalty our ability to influence behavior. We do that with “next best actions.”
Value-based care is the sport of the future. It may take a while, but it is the sport of the future. That pay-vider model is coming fast. New competitors are coming in to take advantage of that if our current health systems don’t. Our job is to work with today’s health systems and payers to say, this what’s coming. We can help you bridge the gap to this membership model. To this proactive engagement, where you drive value, delight, and loyalty. We have the portfolio of “next best actions” to do it. At least as I know it today, we are the only company that is working with healthcare providers that hang expected values on “next best actions,” and that is critical to investing and making them happen.
Comments Off on HIStalk Interviews Mike Linnert, CEO, Actium Health







































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…