Neither of those sound like good news for Oracle Health. After the lofty proclamations of the last couple years. still…
News 1/6/21
Top News
Value-based care performance management company Cedar Gate Technologies acquires population health IT vendor Enli Health Intelligence.
Enli earned “Best in KLAS” designation for population health management in 2017, 2018, and 2020.
Enli’s roots go back to 2001 as Kryptiq, which then worked with Providence Health & Services to commercialize the latter’s CareManager starting in 2016. Kryptiq acquired CareManager in 2012 and was then itself acquired by Surescripts the same year, and Surescripts spun off Kryptiq in 2015 as Enli.
Kryptiq was founded by Luis Machuca (Enli CEO), Jeff Sponaugle (CTO of Surescripts), and Murali Karamchedu (Enli CTO).
Reader Comments

From Peony Picker: “Re: Haven. Why do you think it failed?” We don’t know much about the company’s mission, priorities, and plans, but here’s my armchair quarterback opinion:
- The idea that Haven’s three big bureaucracy owners would join hands and fix healthcare was naïve from the start. Companies that size can’t change the impenetrable fortress of healthcare by halfheartedly forming a company that was barely bigger than their bathroom supply expense task force. Politics and conflicting objectives make just about every joint venture a failure.
- Amazon was the only one of the three participants that knows anything about healthcare beyond what it costs and had little incentive to share its knowledge instead of creating new business lines, as it is doing now with PillPack. I would bet that most of whatever commercially viable “learnings” can be plucked from the ashes of Haven will end up as Amazon products.
- It took 14 months for the company to even choose a name for itself and it never made it clear exactly what it was doing. Haven basically disappeared immediately without displaying any anger, joy, or boldness, basically launching itself like wheezing legacy business that was just trying to hang on under journeyman leadership.
- Atul Gawande is big-picture influential, but was probably not necessarily the best person to lead this kind of business, not to mention that we don’t know what kind of marching orders and resources he was being given by his many bosses.
- The three owner companies have employees scattered all over the place, and other than maybe Seattle in the case of Amazon, they weren’t going to scare big health systems very much by threatening to take their business elsewhere. Those health systems have spent fortunes building their brands, and while their self-developed reputation may not always be matched by their outcomes, their employees wouldn’t be thrilled to be excluded from the gleaming skyscrapers downtown and instead turfed off to lesser-known but better and/or cheaper hospitals.
- Health systems hold nearly all of the useful personal and aggregated health data and don’t share it freely with competitors, making it easy to starve out an outsider whose business model is based on analytics.
- All big companies hate paying high healthcare costs and getting poor outcomes in return, but none of them have had any success whatsoever in disrupting the status quo. The idea that employers hold power over the healthcare system has been repeatedly proven to be untrue.
- Employers want to reduce healthcare costs to the maximum extent possible without driving away their most valuable employees. That tension varies by company, region, and overall benefit design. It would be easy for companies to either reduce their healthcare costs to zero (by not offering any healthcare benefits) or to spend a lot to make recruitment and retention easier, but anything in between is hard to tailor to meet those competing company objectives.
From Rants On Fire: “Re: grammar. It’s like wearing masks — you do it for others.” Actually, it’s like masks in that correct use benefits both parties. Many in the anti-mask cohort are perceived rightly or wrongly as lacking intellectual ability, possessing little empathy for others whom they could protect with the tiniest of efforts, and choosing a puzzling platform to convince themselves of their illusory autonomy. Taking the extra time to communicate clearly within the broadest rules of the road is the same — you look smarter, it shows that you value your own message, and it demonstrates that you’ve found meaningful ways to display your rugged individualism beyond exhibiting sloppiness and defying anyone to criticize you for it. Most of us are knowledge workers in which rewards seldom accrue to those who appear lazy, ill-informed, or selfish.
Webinars
January 13 (Wednesday) 2 ET. “The One Communication Strategy Clinicians Need Now.” Sponsor: PerfectServe. Presenters: Clay Callison, MD, CMIO, University of Tennessee Medical Center; Nicholas E. Perkins, DO, MS, hospitalist and physician informaticist, Prisma Health. Healthcare organizations are leveraging their current investments and reducing their vendor footprint, so there’s no room for clutter in healthcare communication. The presenters will describe the one communication strategy that clinicians and organizations need today, how to improve patient experience and protect revenue, and how to drive the communication efficiency of clinical teams.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Haven, which launched in 2018 with the goal of improving healthcare costs and outcomes for employers, notifies its 57 employees that it will shut down by the end of February. The joint venture among Amazon, JPMorgan, and Berkshire Hathaway started losing executives in 2019 with the departure of COO Jack Stoddard, followed by high-profile CEO Atul Gawande, MD last May, Head of Measurement Dana Safran in July, and CTO Serkan Kutan in September. Analysts believe the company’s efforts to improve care access, insurance benefits, and prescription prices were stymied by separate, employee-focused projects that were being conducted by its founding members.
Population health technology company Color raises $167 million in a Series D funding round led by General Catalyst, bringing its total financing to $278 million.

France-based Volta Medical, which has released AI-powered arrhythmia management software and is working on software to improve the first-procedure accuracy of ablation surgery for atrial fibrillation, raises $28 million. President and co-founder Julien Seitz is an interventional cardiologist at Saint Joseph Hospital in Marseille.
Healthcare compliance, consulting, and credentialing firm VantagePoint Healthcare Advisors merges with assurance, tax, and consulting firm BerryDunn.
Sales
- State of Franklin Healthcare Associates (TN), Syracuse Orthopedic Specialists (NY), and Hudson Headwaters Health Network (NY) choose Emerge’s health data integration and aggregation software and services.
- Adena Health System (OH) will implement Epic through a Community Connect partnership with Ohio State University Wexner Medical Center.
- Withings will use Redox’s API to connect its Med Pro Care remote patient monitoring devices with EHRs.
People

Sam Hanna, PhD, MBA joins Divurgent as EVP of innovation and consulting / chief strategy officer.

Direct Recruiters promotes Mitchell Herman to partner.

Ken Levitan, who served as CIO of Einstein Healthcare Network for 10 years through 2015 and is now EVP/CAO, is named as its interim president and CEO.

Industry long-timer Jay Deady (Jvion) joins claims cost and payment optimization solutions vendor Zelis Healthcare as president. He rejoins fellow Eclipsys alumnus Andy Eckert, who is CEO.
Announcements and Implementations

Arcadia announces GA of solutions to help providers with COVID-19 vaccine programs, including patient-focused resources for education, targeted outreach, engagement, stratification, and dose tracking; plus reporting and analytics.

The University of Vermont Health Network pushes back the second and third phases of its Epic implementation, citing the need to focus its resources on COVID-19 response efforts and continuing recovery from an October ransomware attack.
West Virginia OrthoNeuro implements Emerge’s ChartGenie to convert data to its new Athenahealth EHR and archive legacy data.
Ochsner Health (LA) goes live on Vynca’s advanced care planning software, giving physicians access to Louisiana Physician Orders for Scope of Treatment forms from within Epic.
Retia Medical uses the Device Driver Interface development strategy from Capsule Technologies to connect its Argos Cardiac Monitor to other systems.
Independent urgent care provider FastMed goes live on EvoHealth’s zero-footprint PACS in its 100 locations.
Government and Politics
ONC publishes Cures Act developer resources, including a summary of compliance dates and an API resource guide.
A Nature paper by health privacy expert Deven McGraw, JD, MPH and Boston Children’s Hospital’s Kenneth Mandl, MD, MPH says that US privacy and security protections are not sufficient to fuel a learning health system, making these points:
- Non-traditional health data is used widely for commercial purposes without regulation.
- Social determinants of health information could be improperly used by companies, such as to avoid high-cost areas and populations.
- Health data protections need to include penalties for uses that harm people or populations.
- HIPAA coverage is based on which organizations hold patient data rather than the data type itself, and much of the health-related information that is being collected (such as by apps) falls outside of HIPAA.
- Regulatory authority shifts from HHS OCR to the Federal Trade Commission as data flows from covered entities through APIs to consumer apps. FTC’s authority does not extend to non-profit organizations and insurers and FTC’s protections and enforcement mechanisms are not comprehensive to healthcare.
- The public is realizing that HIPAA offers them little protection, such as allowing covered entities to sell their de-identified data that can be readily re-identified.
- Big tech companies are getting involved in healthcare who have behaved questionably in their data collection and consumer tracking.
- It isn’t adequate to provide consumers with a notice of how their data will be used as a condition of using an app or service. The notices are hard to understand, seldom read, sometimes changed without notice, and require consumers to consent to just about any use of their information that companies might come up with in the future. It also puts the privacy burden on the consumer.
- GDPR and state privacy laws, such as the California Consumer Privacy Act, continue to rely on consent and haven’t limited how businesses collect and use personal data.
- De-identified patient data can be re-identified and no penalties exist for doing so.
HIPAA focuses more on what covered entities can do with data rather than which information they collect in the first place and for what purpose, which might be something that should be spelled out, and companies could be prohibited from collecting and selling patient information except for uses that consumers might expect and that would benefit them. - Companies that collect, use, or disclose both identifiable and de-identified patient data should establish independent data ethics review boards.
- Stronger protections are needed for discrimination so that marginalized populations will be confident that they can allow their data to be collected for healthcare learning purposes.
COVID-19
Monday saw another record day of COVID-19 hospital inpatients at 128,210.
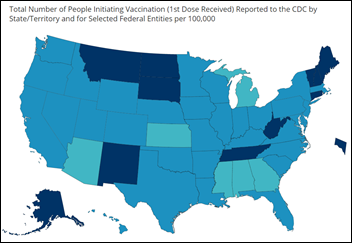
CDC’s data tracker says that 15.4 million coronavirus vaccine doses have been distributed and 4.6 million administered, both falling far short of projections. The states with the lowest percentage of people injected are Michigan, Arizona, Kansas, Mississippi, Alabama, and Georgia.
FDA declines to adjust its approved COVID-19 vaccination regimen to speed up rollout by stretching the interval between doses, giving lower doses, or mixing and matching products, warning that such use has not been studied for effectiveness and may place the public at risk. FDA also warns that studies didn’t continue following participants who failed to get the second shot in the designated time, so assessment of one-shot effectiveness is not possible without additional studies.
Meanwhile, a just-published analysis (not a preprint) in Annals of Internal Medicine finds that the best use of the limited supply of vaccines would be to vaccinate more people initially — using most of the available initial supply and production for the first three weeks instead of holding back half for second doses as is being done today — then holding more vaccine for follow-up injections.
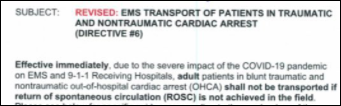
Los Angeles County orders ambulance crews to not transport patients with low survival odds and to conserve oxygen for the most critical patients. Ambulances are waiting up to eight hours before they’re allowed to take their patients into the ED.
New UK research finds that family members who are under 17 are more likely to bring coronavirus into the household than adults and those aged 12-16 are seven times as likely as adults to be the household’s first case. Data consistently indicates that coronavirus transmission is lower when schools are closed.
COVID frontline primary care doctors who aren’t affiliated with hospitals have no access to COVID-19 vaccine, with most of those surveyed saying they don’t even know where they will get the vaccine. Most states seemed to have forgotten that not all doctors work for hospitals, whose highest priority is vaccinating their own employees and those doctors who generate the most revenue.
UCHealth (CO) uses Conversa Health’s automated vaccine monitoring software as part of its employee vaccination program. Data collected from a wearable two days before and seven days after vaccination will be analyzed to help researchers better understand the vaccine’s effects, particularly on high-risk patients and long-term care residents.
States that were somehow caught off guard by the release of COVID-19 vaccines and don’t have online appointment systems for signups are instead using free party RSVP sites such as Eventbrite and SignUpGenius. Others are using sign-up sites that are crashing under heavy volumes and some are simply telling people to join long lines and hope that the shots don’t run out.
Other
ED residents are finding few available jobs upon completion of their programs, as COVID-lowered ED volumes caused hospitals to stop recruiting ED doctors. More than half of US ED doctors work for investor-owned staffing companies that have been more aggressive in cutting back staffing. Some of the residents are doubling down on emergency medicine by signing up for low-paying fellowships.
Private equity-owned medical practices — many of them in dermatology, gastroenterology, and obstetrics — are requiring patients to sign binding arbitration agreements to prevent them from filing medical malpractice lawsuits.
Sponsor Updates
- ReMedi Healthcare Solutions publishes a white paper titled “Increase Go-Live Efficiency with a Virtual Model.”
- Audacious Inquiry customer Texas Health Services Authority receives ONC’s STAR HIE Program Award.
- Change Healthcare announces the successful introduction of its first cloud-based medical tools for radiologists and other specialties.
Blog Posts
- How 3 CEOs Successfully Navigated 2020 (Get-to-Market Health)
- Secure Healthcare IT Offshore Services to Meet Domestic Standards (314e)
- Making sense of the new No Pay RAP (Ability Network)
- COVID-19 Exposes Need for Interoperability & Integration in Healthcare (Part 2) (AdvancedMD)
- AdventHealth – One Unified System. One Team. One Holistic View. (Agfa HealthCare)
- Is Your Patient Engagement Strategy Ready for the COVID-19 Vaccine? (Arcadia)
- Condition Coding Management: Maximize Reimbursement Through Accurate Coding Practices (Bluetree)
- 2020 MIPS Relief for Extreme and Uncontrollable Circumstances (Ingenious Med)
- Exploring Post-Acute Authorization (CarePort Health)
- Healthcare Triangle’s Keys to a Successful Application Support Services Transition (Healthcare Triangle)
- 2021 Health IT Predictions: Fasten Your Seatbelts for Dramatic Transformation (CereCore)
- Access Centers and Patient Orchestration: What Health Systems Need to Know (CentralLogic)
- A word of thanks to front-line health workers (Cerner)
- Enterprise Imaging: Getting Organized and Collecting Data (Impact Advisors)
- How Increased Interoperability in Eprescribing Can Elevate Patient Safety (ChartLogic)
- Telehealth Prescribing is Low – Decision Support Can Help (CoverMyMeds)
- Optimum Healthcare IT Top 5 Blog Posts of 2020 (Optimum Healthcare IT)
- Optimization Shouldn’t Be Confined to the EHR (Divurgent)
- Thirlby Clinic: Using Telehealth and CCM for Better Disease Management (EClinicalWorks)
- Advancing digital health solutions beyond the pandemic (Meditech)
- Stop Digging, Start Climbing: How to Increase Revenue Without Cutting, Cutting, Cutting (EnsoCare)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




“COVID frontline primary care doctors who aren’t affiliated with hospitals have no access to COVID-19 vaccine, with most of those surveyed saying they don’t even know where they will get the vaccine. Most states seemed to have forgotten that not all doctors work for hospitals, whose highest priority is vaccinating their own employees and those doctors who generate the most revenue.”
To make matters worse, pediatricians (who give more vaccines daily than everyone else combined) have been largely shut out of the distribution discussion and process. Instead, pharmacies have been sent to the head of the line (big donors) and unless I misread https://covid.cdc.gov/covid-data-tracker/#vaccinations it looks like the LTCF program from the Feds (which has pharmacies vaccinate Long Term Care facilities) has delivered on only *13%* of the vaccines distributed to them so far, a little less than the rest of the delivery system (35%). And we KNOW CVS + Walgreens aren’t getting paid what the few bucks independent pediatricians get paid for this service.
Is it not possible that Pediatricians aren’t at the table because the vaccine isn’t really ‘tested’ for < 16 y/o?
Pediatricians are the largest immunization delivery network in the US and should/can be used to distribute the vaccine. 100s (1000s?) of practices have signed up to become distributors (I know some who have been approved already) and are waiting to serve their communities, they’re just lumped in with . It’s not about vaccinating the patients <16yo, it's about which parts of the industry already have tested workflows for delivering the vaccines. Pediatricians already know how to do curbside vaccine delivery, know how to track and recall people for their followup shots, know how to run vaccine clinics that can take care of 100s of patients in a morning, and submit to the state IIS programs. And, dear lord, pediatricians are CHEAP.
Community-based Pediatricians are also in vital patient-facing roles. I've heard too many reports of hospital billing staff and work-at-home admins getting their vaccines while non-hospital-employed primary care physicians are left to fend for themselves.
I absolutely love the mask-grammar mashup you did there. Beautifully combines two of my pet peeves. I’m going to steal it – with attribution, of course.
And if I used poor grammar anywhere in this comment, please feel free to correct me.
My point isn’t that grammar and writing should be perfect, but that people should at least make an effort to communicate clearly when they are choosing to expound on a public forum, as a courtesy if nothing else. I make grammar mistakes too, but not because of lack of attention, effort, or respect for those who read what I write.
“The public is realizing that HIPAA offers them little protection, such as allowing covered entities to sell their de-identified data that can be readily re-identified”
Who is buying? Please name names.
Everyone and anyone who has a profit motive to do so. Online advertising is a massive industry, and healthcare providers and pharmaceutical companies participate the same as anyone else. Websites and internet service providers can very easily identify who you are. They know your name, age, sex/gender, and where you live by the time the page finishes loading. They know what other websites you go to. They know what medical conditions you look for on search engines. They are all legally allowed to freely sell, exchange, and reconnect this data however they want. Your healthcare provider doesn’t need to sell identified data when your online presence is basically screaming out your name, everything post you’ve liked, the web pages you’ve visited, etc.
https://www.scientificamerican.com/article/how-data-brokers-make-money-off-your-medical-records/
https://www.bloomberg.com/graphics/infographics/whos-buying-your-medical-records.html
https://www.fiercehealthcare.com/payer/quest-for-identified-data-why-firms-are-starting-to-bypass-hospitals-and-buy-data-directly
https://www.advisory.com/en/daily-briefing/2018/04/10/patient-data
Two options: go full privacy nut, put your smartphone in a microwave, delete all your social media and email accounts, and exclusively use Tor browser with Duck Duck Go. Or, vote for politicians that want to improve consumer privacy protections.
Off the top of my head google and pfizer. More generally, Buyers are Insurance companies including both health and life, large pharmaceutical companies, smaller more research oriented pharmaceutical companies, advertisers, data brokers/resellers, investment firms, consulting firms doing “benchmarking”. If you are actually interested, quintilesims, veradigm, and competitors would be a good place to look.
“States that were somehow caught off guard by the release of COVID-19 vaccines and don’t have online appointment systems for signups are instead using free party RSVP sites such as Eventbrite”
Scammers are also using Eventbrite to steal money from the elderly:
https://thehill.com/homenews/state-watch/532682-eventbrite-sites-targeting-florida-seniors-charged-for-fake-vaccination
In Florida’s defense, at least they are allowing the most vulnerable group to be vaccinated.