HIStalk Interviews Dennis McLaughlin, VP, Information Builders
Dennis McLaughlin is VP of the Omni product division (Omni-HealthData) of Information Builders of New York, NY.

Tell me about yourself and the company.
I have been with Information Builders for quite some time, specializing in data and data integration technologies. I have been involved with the healthcare business since we started investing in it roughly 10 years ago. It has become a significant, strategic part of the business. My role is driving the innovation and the technology direction of our healthcare business to match what the market needs and what our customers are looking for.
What are the most pressing analytics needs of health systems?
The biggest challenge that we run into is around data. There’s lots of great movement in the analytics and visualization space, but in healthcare specifically, having a great tool doesn’t do much if you can’t get the data together and work with it in a dynamic and consistent way.
The pressure that we see a lot for organizations is, “I want to do better care management, but I can’t get the pieces and parts of the data in place effectively to be able to do that.” That’s where we’ve been trying to break down some barriers to make it easy for folks to have access to data, have that data be consistent and comprehensive, and to then be able to apply it to their analytics challenges.
How are health systems that are expanding by acquisition making sense of all of the data that starts rolling in from those new organizations and the systems they use?
Healthcare is awesome and gets me excited when I talk about data, because there’s lots of data out there. It’s not that there’s anything wrong with the data that we have, it’s that the systems that run healthcare generally automate healthcare itself. They deal with people or they deal with financials.
When you’re trying to bring the data together and apply it to a set of requirements that weren’t anticipated when the data was collected — for example, almost anything coming out of care management or population health — you need to be able to take that data, apply some level of governance to it, and then be able to answer the questions that the modern healthcare industry is driving forward.
When we started in this business, fee-for-service was the thing. Now everybody’s working under contracts, whether those contracts are guided by CMS or whether they’re guided by the payer. Trying to look holistically at the patient and be able to provide care in a way that makes sense for the patient’s overall benefit and with reduced risk. All of that is driven by data. If the data that we are trying to base those decisions on isn’t good, then the care can’t be good. We don’t know whether or not that patient has had the appropriate level of care, especially in acute care situations and chronic situations. We don’t know what’s happening. The more data we can bring in, make relevant, and make available at the point of care, the more we can bend the curve.
The other side of this is that traditionally a lot of systems, like EMRs, are right there at the point of care, but some of the advanced data and analytics that you are going after don’t really get analyzed until down the road. It’s hard to make an impact for a patient who’s sitting in front of a doctor.
Another of the trends that we are seeing is, how can we take this insight that we’re developing out of the data, start to bring it to a much more real-time perspective, and get that information right there to the point of care?
Are health systems making bad operational decisions or failing to make operational decisions because their data governance is immature?
It would be unfair to be judgmental to folks on decisions that they made, mainly because in many cases in healthcare, unlike almost any other industry, the business of healthcare tends to drive decisions about the technology. The poor IT department is constantly on the ropes reacting to, decisions such as, “We’re going to have a new EMR. We’re going to have a new system to manage these cancer drugs. We’re going to have a new system to manage cost.”
A lot of our IT partners are responding constantly in a reactive way instead of a proactive way. Despite their efforts, even those who are dedicated to data governance recognize that if the chief medical officer makes a strategic decision about a particular automation system, that thing is probably going to happen. What we have to do after the fact is to figure out how to then govern the data that is flowing through that system and the way it interacts with other systems.
It feels at times like our customers are in a constant scramble to balance the needs of the business, while at the same time recognizing — especially those on the data and IT side — that they have a responsibility to ensure that data is of the highest quality. Especially for the organizations where they’re dedicated to making data be a strategic asset in the way that they approach the business, whether that’s related to quality, care management, or any of their initiatives.
A lot of the initiatives of these health systems relate to being the highest-quality provider in the area, or branching out to cover the largest potential population. That takes us back to, do we have data that can support that agenda?
Are health systems using more external data, such as from claims or pharmacies?
Absolutely. The health systems and organizations that we deal with have a voracious appetite for data. They want everything that they can get. They would like to get data from the payers. They would like to get data from labs that aren’t their own labs. They would like to get data everywhere they can.
Probably the number one question we get involves data related to things like benchmarking or feedback loops. A lot of the folks in healthcare have a scientific background. They are paying close attention to what the market is doing, what particular studies are in play, determining the best way to run their business, and figuring out how to best interact with their patients. In those cases, outside data is critical for being able to do that.
The challenge that they have is that in healthcare, while there are interesting sharing points related to data, I’ve always said, “You’ve seen one HL7 implementation, you’ve seen 40.” While healthcare is moving in a direction of being able to share data more effectively, it’s not the easiest thing for these organizations to do. That’s an area where we try and help them alleviate the pain of that challenge.
Are those health systems working toward reaching out to patients and their communities in general in treating them as customers?
Yes. We have worked with some organizations that have been very progressive in that area. From the ability to recognize when people move into town, to paying very close attention to where they site their clinics and their facilities, trying to match the outreach of the organization to the people in the area where they live, and provide services to folks closer to where they live. All of those would be second nature in certain industries.
You look at an organization like McDonald’s. The way it does its siting is high science. This is coming to healthcare. These folks are recognizing that to be able to effectively manage their customers, their patients, and their families, they have to borrow from some of these other industries. You’re starting to see a lot more of the techniques that we typically might see in marketing, advertising, or retail being applied to the healthcare challenge.
I think it’s a great thing. If I know that a particular group of my patient population has a propensity towards needing cardiac care and I don’t have a clinic anywhere nearby, then I’m not servicing them well. Being able to analyze the patient population, being able to analyze the surrounding market and my competitors, and then taking action accordingly gives an organization a leg up in a market that has become pretty competitive.
Are health systems using technology to help them align with independent physicians, or to co-market their services with their technologies, such as being listed in the health system’s physician directory or taking appointments online?
Yes. Ever since the budget deal that created the requirements around technical automation and doctors, we’ve seen a lot of consolidation in the market related to affiliations. Physicians are joining networks that they never would have considered before or are associating with a network.
At the same time, not everyone is going to hire the physicians into an expanded network. We see organizations we deal with range from, “We are going to expand and market to these physicians and get them to join us” all the way to, “We are going to make their experience so seamless and positive that they will want to affiliate with us, and we can provide a lot of efficiencies that the physician or the physician group wouldn’t be able to provide on their own.”
We did an innovation a couple of years ago that we would not have predicted, and that is around mastering physician practices. It’s not just knowing who the physicians are, but knowing where they’re practicing. Physicians are entering and exiting various practices on a much more frequent basis than ever before. It’s super important for us to be able to feed that information, to be able to say that Dr. Smith is now associated with this other practice even though he spent 10 years at another place.
That has been a rapidly changing part of the market, although you would normally think that data and information would be stable. It’s been changing a lot and we have spent a lot of innovation to be able to match it. We make it easier for these organizations to keep track of those folks and to be able to market them when they’re affiliated and not necessarily employed by the health system or the health network through its various tentacles. When we looked at our roadmap 10 years ago, we didn’t look at physician stability as something that would become a significant data challenge, but we have experienced exactly the opposite.
Do you have any final thoughts?
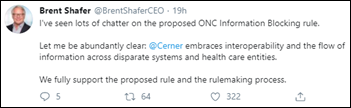
We talked a lot about data, the kinds of things that we’re looking at in the market, and how we are responding. The biggest challenge moving forward for both us and the market is, how do we now use some of the initiatives that are being pushed down by CMS and the market in general — things like FHIR – to take interoperability to a whole new level? One of our key themes for this year is to not only be able to access, manage, and govern this data, but now to look for ways that we can get that data, these analytics, and these insights that derive from the data into the systems that physicians, nurses, and health systems are using to be able to improve care. How to give them additional insight, whether that’s related to social determinants or just pure efficiency. 2020 is the year for better ways of getting data into the hands of the folks that can use it to impact care.
































Favorite flight delay was in a Airbus that had already left the gate and was taxiing on the ground when…