News 3/20/15
Top News
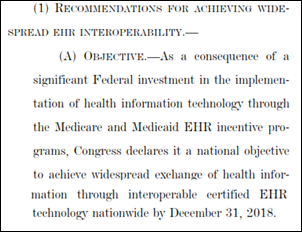
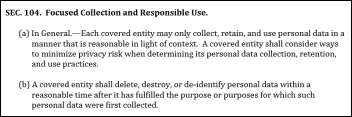
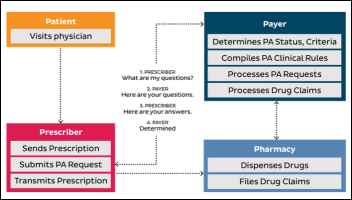
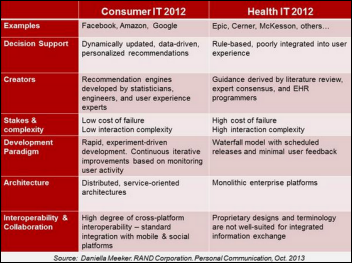
The House’s proposed doc fix SGR bill includes a requirement stating that “Congress declares it a national objective to achieve widespread exchange of health information through interoperable certified EHR technology nationwide by December 31, 2018” and orders HHS to take action if interoperability metrics aren’t reached that could include Meaningful Use penalties and EHR decertification. The bill would also require providers to declare that they that they haven’t restricted interoperability as part of their attestation (that sounds tricky to interpret). It also calls for studying the creation of an EHR feature comparison website. Other language in the proposed legislation addresses data usage and telemedicine, so it’s pretty heavy in IT-related language. Now the political sausage-making begins, hopefully without someone’s ICD-10 Hail Mary sneaked in as time expires.
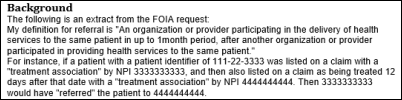
From Data Driver: “Re: Demand-Driven Open Data (DDOD). I’m cautiously optimistic about this new mechanism to open and track government data requests. I say ‘cautiously’ because I’ve seen competent people in HHS’s ‘Entrepreneur in Residence’ program have their projects stymied by unspecified limitations.” HHS’s DDOD program, launched in November 2014, lets startups, providers, and researchers tell HHS (via online use case requests on Github) what data or APIs from CMS, NIH, CDC, and FDA they would like to have. Requests are prioritized by potential cost savings and input from data users, and if approved, the requestor works with HHS to manage its development as a project. Some interesting use cases: retrieve Medicare pricing by CPT, create a consolidated registry of marketed medical devices, export FDA’s drug warning letters to data format, and create a de-identified claims dataset for tracking utilization and quality.
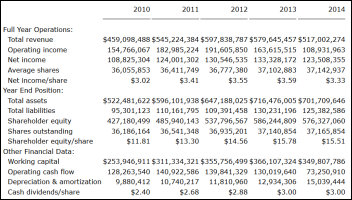
From Brutus: “Re: Standard Register. I haven’t seen any news on its implosion. The CFO resigned in January, they got booted from the NYSE, and now they’ve filed Chapter 11. They bought iMedConsent from Dialog Medical awhile back and seemed to be making a slow transition from their paper forms business.” They’ve announced restructuring plans to sell the company to a turnaround-focused hedge fund for only $275 million. Standard Register’s electronic healthcare offerings include electronic forms, document capture, electronic consent, electronic storefronts, medication history, discharge follow-up, and workflow. The company bought Dialog Medical for $5 million in 2011.
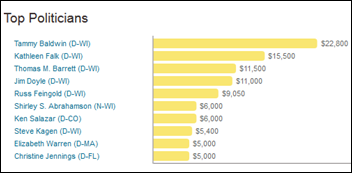
From Sturges: “On the noise around Epic and the Senate interoperability hearing, everyone is missing one piece: who asked the question on CommonWell to Epic’s Peter DeVault? The answer: Tammy Baldwin, US senator from Wisconsin. Judy is one of her largest political donors. So, Epic (and/or Brad Card, their lobbyist) planted the question with Baldwin’s staff. Baldwin is happy to help a large donor. Epic’s DeVault provides his rehearsed, untruthful reply. It is typical Washington." Senator Baldwin is not only Judy’s heaviest-supported politician (Judy’s campaign contributions are listed are above), Senator Baldwin was one of five members of a Congressional delegation that in 2011 wrote a letter to the Department of Defense urging it to consider buying Epic, which seemed cheeky at the time, but now Epic is one of three finalists for the DoD’s $11 billion EHR project and the free VistA is off the table.
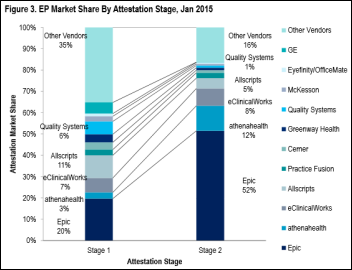
From MrSoul: “Re: Spartanburg Regional Medical Center (SC). They’re going Epic, replacing GE Centricity in the clinics and McKesson Horizon inpatient. That means Bon Secours St. Francis, GHS, and Spartanburg Regional will all be Epic soon. No Epic jobs on their site yet.” Glassdoor is now showing some Epic jobs at Spartanburg Regional.
HIStalk Announcements and Requests
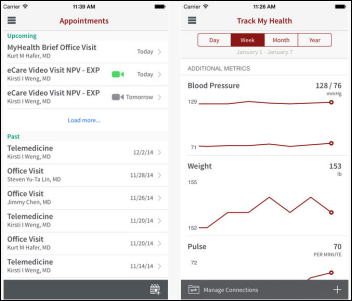
This week on HIStalk Connect: Health Catalyst raises a $70 million Series D round to expand its data analytics platform. Google secures a patent for a wrist-worn system that will search for and then attack cancer cells in the bloodstream. 23andMe announces that it will begin using its genome database for drug discovery research. HealthTap introduces RateRx, a platform for doctors to rate the effectiveness of medications.
This week on HIStalk Practice: Austin Regional Clinic gets into virtual visits via CirrusMD. Mettrum Health launches physician portal for medical marijuana services. AHIP attempts to one-up the AMA in Chicago. VSee helps telemedicine go galactic. Jerry Broderick outlines how practices can give themselves a leg up when it comes to capturing physician commitment. HHS and PwC look back at ACA hits and misses. Zobreus Medical takes its EHR to Kickstarter. Physician optimism around mobile apps may be naive.
Webinars
March 31 (Tuesday) 1:00 ET. “Best Practices for Increasing Patient Collections.” Sponsored by MedData. Presenter: Jason Bird, director of client operations, MedData. Healthcare is perhaps the last major industry where the consumer does not generally have access to what they owe and how they can pay for their services. Collecting from patients is estimated to cost up to four times more than collecting from payers and patient pay responsibility is projected to climb to 50 percent of the healthcare dollar by the end of the decade. Learn how creating a consumer-focused culture, one that emphasizes patient satisfaction over collections, can streamline your revenue cycle process and directly impact your bottom line.
Acquisitions, Funding, Business, and Stock
Clinical trials software vendors CentrosHealth and Clinical Ink merge.
The Houston business paper profiles seven-employee Medical Informatics Corp., which offers the FirstByte alarm management program and says its real-time clinical decision support application should pass FDA approval and enter the market in this year.
IBM invests an unspecified amount in Modern Medicine, which is working on Watson-powered ambulatory clinical decision support.
Sales
Washington’s Department of Social and Health Services chooses a hosted version of Cerner’s Millennium and revenue cycle for three psychiatric hospitals.
Announcements and Implementations
Premier announces PremierConnect Supply Chain to manage a health system’s entire purchasing process including, real-time supply analytics, online sourcing, catalog management, and materials management. Test sites included Adventist Health and Fairview.
Cerner and Intermountain announce implementation of iCentra — the EHR/PM system they’ve been working together to develop — at two hospitals and 24 clinics, with the rest of Intermountain going live through 2016. The announcement says the collaboration makes iCentra “more unique” (which is grammatically horrifying) than competing EHRs.
Government and Politics

California tax authorities and Blue Shield of California are criticized for failing to disclose that the insurance giant’s non-profit status was revoked seven months ago before people starting signed up for insurance on Healthcare.gov. The state’s insurance commissioner applauds, saying Blue Shield charges excessive rates and doesn’t operate any differently than for-profit insurance companies. The organization paid its CEO $4.6 million in 2011 (and has declined to say what it has paid him since) and spent $2.5 million for a San Francisco 49ers luxury box last year. Blue Shield’s just-resigned public policy director is running a public campaign to convert the insurer to a for-profit company that could be worth up to $10 billion and use the money for safety net care. The questions raised could be logically extended to health systems that don’t pay taxes despite billions in income, millions in surpluses, and the highest executive salaries in the non-profit world.
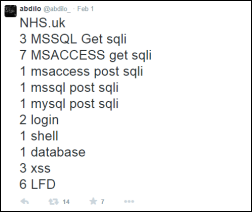
Privacy and Security

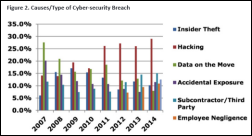
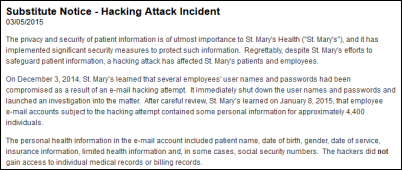
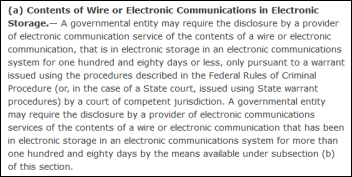
Sacred Heart Health System (FL) notifies 14,000 patients that their information was exposed when the email account of a contracted billing vendor’s employee is hacked. Please, well-intended writers and self-appointed experts – stop yammering about encrypting data at rest (which wouldn’t have prevented any of the recent big breaches) and focus on phishing attacks. They aren’t as easily detected as earlier primitive attempts that featured laughably poor English and poorly disguised links that would fool only the least computer-literate employees. Phishers have become convincing in luring even intelligent people into clicking official-looking links or opening malware attachments that claim to be faxes, legal documents, or password reset links. That doesn’t even account for phone phishing where smooth-talking people convince employees to divulge passwords. Encryption is worth zero if someone steals the password of an employee who has data access.
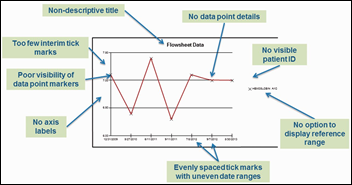
An AHRQ-funded review of how eight inpatient EHRs display lab values finds inconsistency and graphical limitations, with the authors suggesting that ONC beef up certification criteria. Some EHRs failed to include the patient’s birthdate, a description of the value being displayed, or a data legend.
Clinicians and technologists in Vermont join to create MEDSINC, a mobile app for poor countries that allows users with no medical training to input information about a sick child and then receive suggested treatment options based on local conditions. The app was envisioned by UVM pediatrician Barry Finette, MD, PhD and built by Physicians Computer Company co-founder John Canning with input from 10 university pediatricians who reviewed WHO protocols and evidence-based research. Testing at UVM suggests that pediatricians and the app agree 94 percent of the time vs. the 80 percent agreement typically found when two board-certified pediatricians review a case. Field deployment in Bangladesh begins later this year. The developers say it might eventually land in the US provided they can get through the FDA’s process. They’ve formed a company called ThinkMD.

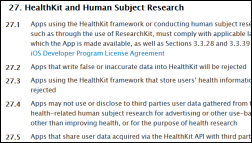
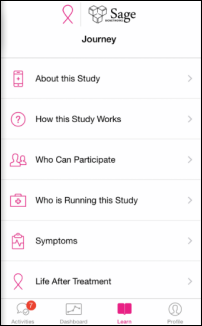
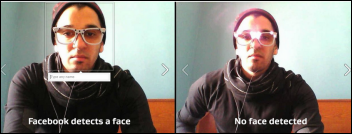
A report says Apple decided to move ahead with ResearchKit in September 2013 after one of its executives heard a Stanford MedX talk by Stephen Friend, MD, PhD, a former drug company oncology SVP who co-founded Seattle-based non-profit Sage Bionetworks that provides tools for large-scale, transparent biomedical research. It says Friend decided to work with Apple rather than Google or Facebook because as a hardware manufacturer, Apple won’t sell data.
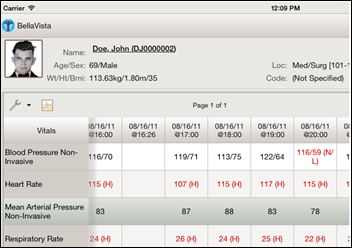
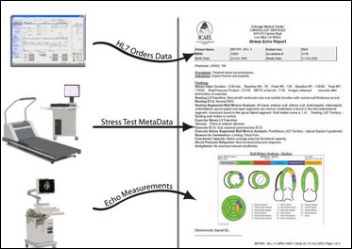
Don DeCoteau is developing BellaVista, an EHR-agnostic, native client (iOS, Android, and JAVA-supported desktop) that displays clinical results with a framework to integrate QR codes, real-time medical device streams, videoconferencing, and voice-based ordering and documentation. He’s got it running with the VA’s VistA to illustrate that the client can work with any EHR that offers an API for accessing clinical information. Don is looking for early adopters.

A New York Times Magazine article pokes fun at people who worship “optimization” because it’s easier to appease their “inner bean counter” than to develop talent or ambition also takes on the Apple Watch in comparing it to the Stalin Gulag’s computer-driven optimization of “maximum work given minimum food”:
After time keeping, the watch’s chief feature is “fitness tracking”: It clocks and stores physiological data with the aim of getting you to observe and change your habits of sloth and gluttony. Evidently I wasn’t the only one whose thoughts turned to 20th-century despotism: The entrepreneur Anil Dash quipped on Twitter, albeit stretching the truth, “Not since IBM sold mainframes to the Nazis has a high-tech company embraced medical data at this scale. And yet what attracts me to the Apple Watch are my own totalitarian tendencies. I would keep very, very close tabs on the data my body produces. How much I eat. How much I sleep. How much I exercise and accomplish. I’m feeling hopeful about this: If I watch the numbers closely and use my new tech wisely, I could really get to minimum food intake and maximum work output. Right there in my Apple Watch: a mini Gulag, optimized just for me.
Other
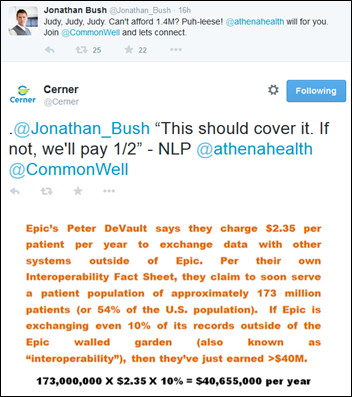
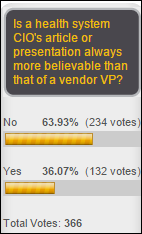
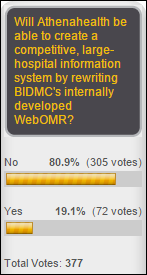
It’s fun to have a sideline seat for the public vendor interoperability squabbling generated by the Congressional testimony of Epic’s Director of Interoperability Peter DeVault, who disclosed upon direct Senatorial inquiry this week that Epic charges customers $2.35 per patient per year to send data to non-Epic systems. Athenahealth’s Jonathan Bush says he’ll pay Epic’s $1.4 million fee to join CommonWell, while Cerner calculates the many millions Epic receives from its data sharing tollbooth. Meanwhile, as reader Where’s Waldo suggests, we can take one important issue off the table right now if McKesson’s John Hammergren will simply state in writing that his RelayHealth business (CommonWell’s technology provider) will never sell data, which is different than having CommonWell itself say it won’t sell data. Hammergren has seemed awfully excited when describing CommonWell to investors.
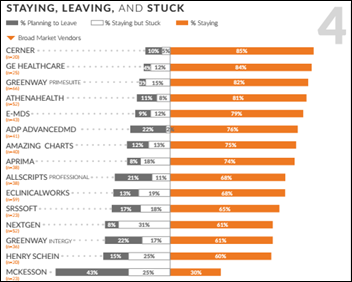
A KLAS report on small-practice (1-10 doctors) EHRs puts Cerner at the top for broad market vendors in a fairly stunning turnaround, with PCC topping the specialty category (pediatrics in its case). Bottom-ranked and trending hard in the wrong direction are NextGen, Allscripts, and McKesson. McKesson leads the pack in clients planning to replace its product at 43 percent, while PCC has the highest planned retention at 98 percent. Small-practice customers in general say their EHR vendors spend too much time chasing Meaningful Use and ICD-10 rather than delivering customer-suggested enhancements. Users of Greenway Intergy, NextGen, and McKesson called their vendors out as having “black-hole syndrome” where support loses or ignores their tickets or fails to follow up. Customers of Allscripts, eClinicalWorks, and Bizmatics complained that the support reps often don’t speak English very well and one NextGen customer reporting that he’s tired of getting calls from overseas at 3 a.m. The biggest complaint by far of customers planning to replace their EHRs is poor usability (although those same EHRs had the same poor usability when those same customers bought them, so those customers are more to blame than anyone).
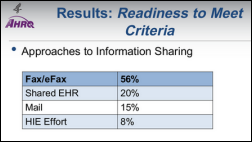
A random telephone survey (which raises validity flags every time even if you ignore the leading questions that are asked or days and times calls were made) finds that 75 percent of respondents think their providers should be able to share their information, while 87 percent don’t think either providers or patients (i.e., themselves) should have to pay for it. Most respondents also said they love puppies and their country (wait, I made that part up). The real way to tell if data sharing is important is to ask people (a) if they’ve switched providers who don’t or can’t share information, and (b) would they pay extra for it.
Epic’s underground Deep Space Auditorium is judged the best new building in America in the over $200 million cost category, with the Madison-based contractor that built it also winning a top award.
A female pediatrician in England accuses a gym chain of “blatant sexism” upon finding that she couldn’t enter the women’s dressing room because the gym’s security system assumes that anyone with a “Dr.” title is male.
An Internet domain company challenges a policy under which the new .doctor domain will be issued only to medical doctors who provide evidence of their credentials, saying it’s not fair to PhDs and companies with “doctor” in their name, such as Rug Doctor.
Sponsor Updates
- PatientSafe Solutions President and CEO Joe Condurso publishes “Liberate and activate EHR data with mobile tools for clinicians and patients.”
- InterSystems releases a white paper entitled, “Data Scalability with InterSystems Caché and Intel Processors.”
- Intellect Resources posts a new blog on “Identifying Your Career Motivators.”
- Hayes Management Consulting Offers “3 Ways to Minimize Anxiety During an EHR Implementation.”
- HDS posts “The Push for Pull Marketing in Healthcare.”
- InstaMed offers “Why Healthcare Needs Apple Pay.”
- E-MDs will exhibit at American Academy of Orthopaedic Surgeons 2015 March 24 in Las Vegas.
- Galen Healthcare Solutions introduces Web Access for VitalCenter in its latest blog.
- Ingenious Med blogs about “The Future of Innovation.”
- Healthwise will exhibit at the World Health Care Congress March 22-25 in Orlando.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.



































































































































































































































The New Yorker cartoon of Readers Write articles.