Monday Morning Update 3/11/13
From Beth: “Re: athenahealth. My little brother just got a job at athenahealth in Boston. Should I congratulate him, or give him stolid advice on keeping a work-life balance? What are the differences between Epic and athenahealth for an implementer?” Good question, which I will defer to readers since I have no first-hand employee knowledge of either company having spent my working life in non-profit hospitals.
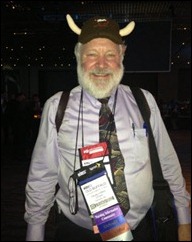
From Cat’s Eye: “Re: Neal Patterson. Let’s start a game of Where’s Waldo? with him. Here he is in the UpToDate booth.” I have to admit that I like Neal’s look.
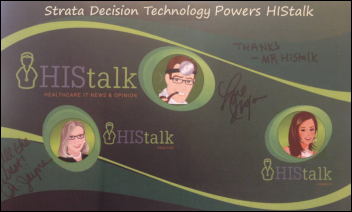
From Boy George: “Re: HIStalk. HIStalk has not been a HIMSS booster and I know as a fact that HIMSS is acutely aware (and envious) of your sponsorship exposure and HIStalkapalooza.” I would hope HIMSS has other HIT worlds to conquer without worrying about my microscopic corner of it. I’ve been writing HIStalk for 10 years while working in a non-profit hospital, so I work pretty hard for whatever success I get, and that success wasn’t (and isn’t) my motivation anyway. As for HIStalkapalooza, I’ll give credit to the companies that sponsor it and the folks who spend the evening with us each year. I do greatly admire the companies that sponsor HIStalk since for most of them, it’s not just a traditional ad buy but rather their interest in truly supporting what I do. I had none for the first few years of HIStalk and I don’t take any of them for granted. I seem to vaguely remember AMIA or CHIME or some group wanting to work with me years ago, but they realized that I’m a loose cannon.
From HIMSSed Out: “Re: booth experiences. Jeff at eClinicalWorks gave a very concise perfectly targeted presentation of their software doing a sore throat visit. No excess, no droning on, just answered my questions in a timely manner. Well done. Lyndsey at athenahealth did a very nice sore throat demo showing me what I needed and answering questions expertly. AND she blew me away when escorting me to be scanned and then handed me a KINDLE to read their material on. Put me down as impressed by the demo, low key attitude, and rocking gift!” I criticize the folks who use the booth as their employee lounge without naming names, but I like calling out those people who do a good job. There is no reason reps need to use their phones during booth duty – assign someone to monitor and return their calls and e-mail if need be, but if you give anyone under 40 a smartphone they’re going to be screwing around with it nearly constantly because that’s what they do off the job and they can’t resist its lure.
From Frank Poggio: “Re: MU. Farzad Mostashari recently said the MU Incentive bonus was safe. So much for political promises. The sequester cuts include an across-the-board reduction in Medicare payments of 2 percent effective April 1 and include cuts to MU bonus money. In my opinion, this will be just the beginning. Big deficits usually mean big cuts for providers. The Obama administration sold the HITECH act to Congress based on a projected savings of $800 billion per the original Rand study, which just a few months ago Rand said was full of errors.” Government doesn’t have “get smaller” in its vocabulary, so I’m pretty sure agencies will apply their sequester reductions in the most publicly visible way possible, i.e. shutting down national parks and closing offices early in the hopes of creating public outrage. There is no way that the government is so efficient that a 2 percent cut should even be noticeable, but they will make it so in protest.
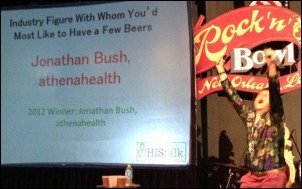
From Guy with the Funny Accent: “Re: HIStalkapalooza. No longer talking to Bonny Roberts as she wouldn’t let me wear the Mr. HISTalk ‘Secret Crush’ sash on the final day of the exhibition.” I like that my secret crush is protective of her regalia. I think I may have blushed a bit as she read her poem on stage and I’m not so sure Bonny didn’t as well since she wasn’t planning to recite her work in front of a bunch of people. She figured out who I am when I lauded her demo style in the Aventura booth a couple of years ago, and with minimal provocation, recited my comments verbatim as we were entering Rock ‘n’ Bowl. She is, as they say, a trip.
From A. Vendor: “Re: HIMSS. It was a wonderful experience for a first-time vendor. HIMSS staff were absolutely wonderful in making preparations and taking care of our needs during the show. It couldn’t have been more effortless. Other than a modest case of booth envy, things went very well and exceeded my expectations. People who were looking found us. We met many interesting colleagues and a number of old friends. In addition to a few good leads, we stumbled into some unexpected opportunities we hadn’t expected. I’m definitely up for 2014, and maybe a little wiser.” I think part of being happy with the exhibitor experience is setting reasonable expectations, like having a central location to meet with clients and prospects, maybe picking up some foot traffic even in the hinterlands, and having access to other vendors in the hall during off hours. Non-vendor HIMSS attendees miss the point that many deals are struck between vendors during the show – marketing agreements, signing up to help with consulting and staffing needs, and perhaps finding an investor if that’s on the agenda. One vendor told me that the VC folks were rapid-firing from one booth to another without regard to what company occupied it, barking out a series of questions about their business in hopes of finding companies to invest in.
From Data Sharing Optimist: “Re: CommonWell. Started six months ago when Arien Malec (now Relayhealth/McKesson, but remember he did a stint with ONC and developed Direct) connected with Dr. David McCallie (VP, medical informatics at Cerner) – they are both very good guys and they decided to create some standards for this type of data sharing. They just finished the standards a few weeks ago. Neal and John H. loved the concept, because even though it might have some competitive issues, they both truly want to see the healthcare system improved, as do all the major CEOs. They went to a small group of folks they believed would hop right on board so they could get a press release out by HIMSS. They did not ask everyone, including Epic, but are talking to them now. From what I heard, they didn’t mean it to sound like Epic refused. That was not their intent, but with two weeks to pull things together, they had to limit things. I talked to Carl about it and got the sense that Epic needs to learn more and see if it is real, but would likely join eventually. Use cases will involve a specialist being able to view and even accept data from an outside hospital on a shared patient, as well as pharmacists being able to bi-directionally communicate with doctors.” Someone who knows all the players told me the same thing – it had to be Malec and McCallie since those are the guys smart enough to make it happen and sell the idea to the suits. I think it was a mistake to rush the announcement and play up the participants without having even invited major vendors like Epic and eClinicalWorks, but apparently the PR urge was strong. So far its accomplishments involve press releases and a Web site. One might logically ask questions like: (a) who pays for the service since infrastructure is required? (b) does the EMR user have to buy or install anything? (c) what are the queries running against? and (d) how is this better than companies like Epic and others that already allow sharing information outside their systems? I like the idea of a standard way of doing things without having a particular vendor owning the platform, so we’ll see if it happens or gets smothered in the bureaucracy of these not-always-nimble big companies.
From Ole: “Re: We are in discussions with EmergeMD regarding telemedicine and would like your unbiased opinion.” I don’t know anything about the company, but perhaps readers who do will weigh in. I would have kicked tires on your behalf at HIMSS but I ran out of time. Actually I didn’t run out of time, but I was so tired of traipsing the exhibit hall by early Wednesday afternoon that I went back to the hotel well before the exhibits closed, had a very early dinner, and finally took my shoes off to write HIStalk. I was really tired, although I now know that I was coming down with a bug at the time.
Here’s to you, IT foot soldiers who will be wide awake at 2:00 a.m. Sunday to make sure systems don’t choke when their clocks spring forward. I’ve been there.
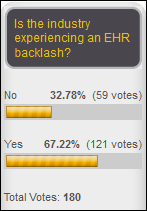
Two-thirds of poll respondents say we’re experiencing and EHR backlash. New poll to your right: why do you think several vendors formed CommonWell Health Alliance?
Speaking of CommonWell, I noticed that they’ve populated the FAQ section of their site. They say the organization won’t actually be established until a 12-18 month proof of concept is completed, making you wonder why it was necessary to announce so early other than to put a stake in the ground.
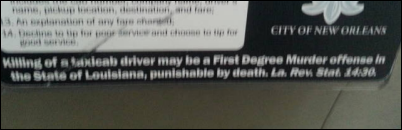
I hope everybody got out of New Orleans OK. I left Thursday afternoon and the airport was an absolute zoo, so I can only imagine what it must have been like Wednesday evening. Security and check-in lines wound throughout the terminal, the concession vendors ran out of pretty much everything (including cream for the coffee), and the little airport didn’t have enough seats so people were sitting on the floor. It is clear that New Orleans, for all of its virtues, just can’t handle a conference the size of HIMSS without a lot of snafus.
I got home only to be hit with a respiratory infection that sent my temperature soaring and kept me up hacking all night, so I’ll just clean up some loose ends and get back to my Tylenol and Halls cough drops.
UPMC goes to paper for three hours when its patient care systems go down due to human error.
Ernest Health will work with NTT Data to create new post-acute care capabilities in its Optimum product suite.
Heritage Groups makes an unspecified investment in coding services and software vendor Aviacode.
I mentioned several days ago that I received advance word that several EHR vendors would be announced as working with Michelle Obama’s Partnership for a Healthier America in adding obesity-related features to their products. “Several” turned out to be “three”: Cerner, GE, and Physician’s Computer Company. I like the idea and I’m not sure why other vendors didn’t sign on, except maybe because they’re already diverting much of their development budget into complying with federal requirements instead of delivering user-requested enhancements.
Just to clarify a reader’s comment last week: GE Healthcare sold its outsourced physician billing service, not software products like its EMR.
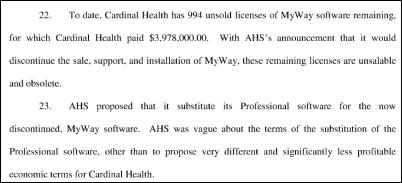
Another MyWay-related lawsuit is filed against Allscripts. Cardinal Health pre-paid $5 million for 1,250 MyWay licenses for resale in April 2009 and is stuck with the 994 of those licenses that it hasn’t sold and are now valueless since MyWay won’t be made ICD-10 and MU compliant. Cardinal looked at Allscripts Professional and passed because of cost, complexity, and the fact that Allscripts sells it directly and they don’t want any part of that as a substitute. Cardinal is suing for beach of contract and wants the $4 million back for its unsold MyWay licenses.
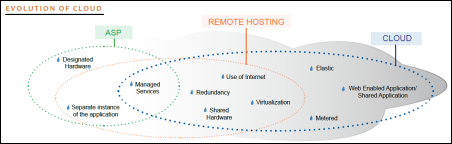
KLAS releases a very small study (100 providers) of cloud computing perception. It says vendors are sloppy with their terminology, calling products cloud-based that are really just hosted and using Citrix or other emulation services instead of true Web services. I like the graphic above.
TeraRecon introduces iNtuition Review, which I’ll describe in the company’s words since it’s a little over my head: “iNtuition has always complemented PACS with advanced functionality to resolve specialized use cases and workflow challenges not adequately addressed by existing PACS solutions. This role is now expanded and enhanced with the new, powerful iNtuitionREVIEW client, designed to complement PACS with multi-monitor display of multi-modality data, in specialized use-cases such as cardiac (CT, MR, Cath, Echo, EKG) or breast (MR, Mammo, Ultrasound). iNtuitionREVIEW is also designed with co-operation and collaboration in mind, with specialized features for the preparation and execution of physician conferences, demos, and multi-disciplinary team meetings.”
Weird News Andy titles this story “An Arresting Development.” A Florida OB-GYN e-mails a patient, threatening to have her arrested if she doesn’t come in for an emergency C-section for her week-overdue delivery. WNA also says he’s not surprised by this 30/70 rule: a third of VA primary practitioners say they’ve missed critical lab results in the EHR due to being overwhelmed with alerts. PCPs said they received an average of 63 alerts per day, with 87 percent saying that’s too many and 70 percent say they can’t manage them all.
Arcadia Software will expand the use of ICU patient monitoring software it developed for Boston Children’s Hospital by collecting data from a network of hospitals to develop insights into treatment decisions and outcomes.
Vince covers the origins of HIMSS in this week’s HIStory.
Final HIMSS Conference Thoughts

Inga liked this: the Vonlay folks prepared a welcome package for newly anointed HIStalk Queen Sarah, who works there (note the labeled cupcakes). Some companies were planning to frame the sashes their employees wore and some folks were supposedly going to wear their sashes to the conference on Tuesday although I didn’t see any first hand.
A low-key announcement during the HIMSS conference involves the formation of the HIMSS-backed accelerator Avia, which is supposed to help provider organizations implement innovative technologies. I don’t really understand what they’re trying to do even after reading the information on their site. Nor do I understand why HIMSS is involved. HIMSS might as well bite the bullet and just buy some vendors and peddle their products directly since they’ve encroached into almost every other aspect of the market.
Brian Ahier got Karl Rove to talk about healthcare IT on camera at the conference.
Vendors have told me that it’s so expensive to dismantle, ship, and store components of their HIMSS booth that a lot of the glitz you see in the exhibit hall goes right to the trash afterward. Good idea by Orchestrate Healthcare, which bought furniture for its new two-story booth and donated it after the show to the New Orleans chapters of Habitat for Humanity and Ronald McDonald House. There’s even a patient aspect: Ronald McDonald House was planning to convert part of its dining room into a conference room where and families can meet with caregivers and Orchestrate’s donation of tables and chairs made that room immediately available for its intended purpose since they had no furniture otherwise.
This reader-supplied HIStalkapalooza photo appears – by virtue of an optical illusion — to have captured Jonathan Bush ticking the chin of an unamused Farzad Mostashari.
The majority of people who left the conference Wednesday missed the most electrifying and informative presentation I’ve seen at a HIMSS conference. I was walking over Thursday morning and a fellow attendee warned me that Farzad Mostashari is a dry presenter because he’s a data guy. I could not disagree more – he is a really good speaker who uses data to support his statements. ONC posted his 2012 keynote on YouTube and I hope they do it again for the 2013 version since everybody needs to hear what he had to say.
Inga and Dr. Jayne are still swooning that the PatientPay folks sent them each a chocolate high heel, thus combining two of their most cherished vices into a single package.
HIStalk traffic was heavy during the conference as it usually is, with visits and page views peaking on Tuesday at 11,000 and 19,000 respectively. Inga, Dr. Jayne, and I were posting and occasionally tweeting from New Orleans, of course, while Lt. Dan kept the home fires burning with daily HIStalk headlines and HIStalk Connect posts. It’s a bit of a potpourri during HIMSS week since we cover whatever is interesting to us, which is almost everything.
More HIStalkapalooza pictures by Istrico Productions. Lots of smiles. I always feel strange seeing my logo (the new one in this case) put on buses, shirts, signage, and electric lights.

HIMSS Takeaways
Attending the HIMSS conference is like trying to simultaneously watch every channel on satellite TV. You choose what looks good in the guide, but invariably there’s a lot of crap among the good finds in both the education rooms and the exhibit hall. Even then you’ll see maybe 5 percent of what was offered. At any tableful of people, the only shared experiences may well be the keynotes and perhaps a large social event (looking at you, HIStalkapalooza).
That makes it really risky to summarize the experience and draw relevant inferences from it. Here are my thoughts, which may differ wildly from yours.
- The CommonWell Health Alliance announcement delivered the burst of fireworks that everyone expected, but whether it’s a new commitment to patients or simply an expedient anti-Epic marketing strategy developed by marginally committed members remains to be seen. We don’t really know what will be delivered, whether it will work as described, and how hard it will be for providers to connect to whatever communications infrastructure is developed. If it succeeds, will it put yet another nail in the HIE coffin? Can it be successful without the participation of vendors like Epic, eClinicalWorks, and others? Can vendors really deliver the needed technology along with their ICD-10 and Meaningful Use enhancements, and if so, how will they prioritize the work? It’s easy to get wrapped up in the feel-good, patient-friendly marketing prose and characterize non-participants as patient haters, but let’s see what they can deliver and which companies dominate the process before waving the CommonWell flag.
- Analytics doesn’t make good booth demos, so it’s hard to have a solid takeaway. Everyone knows they need better data, but approaches range from technical toolkits to turnkey systems complete with algorithms and reports for common requirements. We’re past the multi-year, big-expense data warehouses of just a few years ago, but it would still be easy to make a misstep in the zeal of preparing for ACOs and other delivery changes for which the data requirements are still fuzzy. This may be yet another area where providers will wish they had measured twice and sawed once.
- New Allscripts CEO Paul Black has wasted no time in trying to erase the painful memory of a series of Keystone Cops-like corporate gaffes that left the company as a punch line. Remarkably, some recent Sunrise sales and the acquisition of Jardogs and dbMotion provides validity to their claims as a serious player, although it’s early in the recovery.
- The industry is quickly transitioning from the traditional hospital and practice system model, which emphasizes transaction entry and charging, toward a public health focused emphasis that requires heavy consideration of non-episodic patient activity and cost management. This will require yet another round of vendor technology investment on top of ICD-10 and Meaningful Use requirements, polarizing the market even more into those vendors positioned for the future vs. those just trying to milk what market is left selling old-school systems.
- HIMSS finally recognized the role of patients in the healthcare system, at least superficially. You’ll know the movement is real when real patients and their advocates lead significant sessions, hold non-token HIMSS roles, and are actively represented on vendor advisory groups and even company boards.
- More and more of the healthcare IT market direction is driven by the government in general and ONC in particular. Vendors and customers aren’t talking a lot about incremental enhancements or product tweaks. It’s all about analytics, transparency, interoperability, and outcomes. It will be a challenge to turn these somewhat vague concepts into concrete development plans.
- The audience for usability seems to be selective. Lots of people are talking about it, but nobody’s doing much despite government report emphasizing the need to make systems safer and easier to use.
- The market for consulting services is going to be very strong, but it will shift from system selection and implementation to system optimization. That will drive consulting firms to further specialize into specific practices, most notably for Epic and Cerner. IT systems are necessary but not sufficient to drive the needed changes, and that will favor CIOs who have a good working relationships and reputation outside of IT.
- mHealth has a decent chance of improving health in nations where the problem is lack of basic health needs and medical services. It doesn’t seem to have the required impact in countries challenged by prosperity-fueled problems like obesity, lack of exercise, and time-challenged citizens who don’t put their health first.
- The HIMSS conference keeps getting bigger, but nobody knows if the proportion of actual practicing caregivers (rather than former caregivers turned IT cheerleaders) is increasing or decreasing. It’s easier to be irrationally exuberant when the front-line naysayers aren’t in the building.
- My assessment of the educational program and the CE submission process is that it continues to go downhill, making it almost an afterthought to the cash cow, the exhibit hall.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.









































































































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…