Readers Write 3/19/12
Submit your article of up to 500 words in length, subject to editing for clarity and brevity (please note: I run only original articles that have not appeared on any Web site or in any publication and I can’t use anything that looks like a commercial pitch). I’ll use a phony name for you unless you tell me otherwise. Thanks for sharing!
Sampling the Legislative Sausage
By Civics 101
Be careful reading the proposed Meaningful Use regulations. Note the “proposed” part. As a Notice of Proposed Rulemaking, it’s unwise to ignore any part of the document.
Every word in the document – even in the preamble — has survived numerous rounds of federal vetting. Every section is important, but especially so are those areas in which public comment is invited. Objectives may be added or removed, so don’t get hung up on those to the exclusion of the preamble or the overall intention.This is not a set of business requirements that is ready to be handed off to programmers to implement.
Read the NPRM as a big picture, keep an open mind, and try to understand the intention, not just the tentative objective list. And above all, don’t forget that while Stage 1 is locked in place, Stage 2 isn’t. My organization and yours need to study the NPRM carefully and comment on what we like or don’t like about what’s been placed before us. Remember all the changes that were incorporated between the Stage 1 NPRM and the final version? Every one of those came as a result of public feedback.
Using the iPad in Surgery
By Michael B. Peterson, MD
I use the iPad every day while rounding at work and connected to the encrypted hospital wireless network, finding web information for patients and showing educational videos. I use a Bluetooth keyboard and sometimes a stylus that fit into a netbook soft case when I need to do heavy typing.
We were doing a complicated vascular surgery, an axillary femoral femoral bypass. I had dissected out the blood vessels on the right groin, but the surgeon working on the left could not locate the critical arteries and branches. The patient did not have any pulses in the groins because of severe vascular disease.
I had the nurse drop the iPad into a sterile sleeve and seal it. I used it to pull up the CT scans on the table and paged to the proper level so we could compare the right to the left. Then we knew where to go. We could place the iPad right on top of the patient and visualize what we needed.
Then while my colleague and our PA completed the left side, I checked my Lotus Notes e-mail, went into the vascular econsult program and triaged some vascular consults to the appropriate clinics, and checked my inbasket in our Epic EMR to read labs and answer messages (the iPad runs Epic very well.) When I was done, we were ready for the rest of the surgery.
The x-ray viewing is an innovative project on which we are partnering with with Thinking Systems.
We are using the latest Citrix Receiver to host our version of Epic on the iPad and other devices as well. Since the rollout of Epic Summer ’09 across the country in all Kaisers, the old web address we used for Spring ’06 access no longer works for the iPad. In addition, there are additional video requirements for Summer ’09 that our current web servers need that the Citrix receiver cannot handle. Attempting access to the Summer ’09 environment will result in a connection failure with a “USKIN” error message.
Fortunately our Kaiser web engineers were aware of this and understood the need for iPad functionality. They created special web addresses for Kaiser iPad users in Northern and Southern California, Hawaii, and Pacific Northwest. The official term is PNAgent Site. Setting it up is complicated, but the iPad works very well.
Of course there are ergonomic challenges with a smaller screen, and accurate tapping is critical. But it is so fast and convenient — you don’t have to wander around looking for an unoccupied keyboard and computer. If I need to look up something, I just do it where I am. It has really spoiled me.
I don’t know if there is any way to demonstrate improved outcomes with the iPad. Kaiser is starting to roll it out to other medical centers with different specialties. My general feeling is that with the EMR, there is a 20% productivity hit with data entry and typing your note. It does take longer on the generic computer, but the the iPad is so much faster and it literally puts the medical record at your fingertips… or perhaps the patient’s.
I plop the iPad down in front of the patient and point out pictures, diagrams, and a quick graphic plot of their rising creatinine. I run the lymphedema pump movie to show them how it works, or review the online video again to remind me or others how that endovascular closure device works again before I actually do it.
I have invested the time it took to get comfortable with the iPad and arrange it the way I want. I could not do without it. I have very little specialized software on the iPad except for the VPN and the Citrix Receiver. And my medical apps, books, and games!
Michael B. Peterson MD is a surgeon with The Permanente Medical Group in Hayward, CA. His use of the iPad in the operating room was featured in the April 2012 edition of Macworld. Since Mike is an old friend of HIStalk, I asked him for more detailed information, which he provided above.
What Do You Do Regardless? Five ICD-10 Steps To Continue
By Torrey Barnhouse
The AMA lobby is strong. US government program delays are common. The two came together on February 16, 2012 when Health and Human Services Secretary Kathleen Sebelius announced a potential delay in the October 1, 2013 deadline for ICD-10 implementation.
The announcement, made just before the start of the HIMSS12 Annual Conference, left a lot of attendees scratching their heads and asking themselves, “Now what?” Most agreed a delay of one year or less gives everyone more time to prepare, train, and test. However, a delay of greater than one year spells chaos for healthcare providers and payers.
While at HIMSS, TrustHCS had the honor of sponsoring an executive roundtable on ICD-10. During the roundtable, speakers discussed five ICD-10 projects that should continue full steam ahead despite the delay. It’s a good list and worth sharing.
In general, the panel’s advice was to identify ICD-10 tasks that have collateral benefit for ICD-9 coding. These are the tasks that should be continued until such time as HHS makes another announcement regarding their plans, intentions, and deadlines.
Vendor and Payer Assessments
Continue checking with vendors and payers to see when systems will be ready for testing. Know what the ICD-10 upgrade will cost your organization, if anything. If your vendor simply can’t accommodate, start evaluating new systems to replace them. Conduct ICD-10 testing with your payers whenever and wherever possible to help reduce backlogs and denials upon go live.
Clinical Documentation Improvement
Any improvement in clinical documentation specificity and granularity will help support better, higher quality coding and reduce time wasted querying physicians. Coders can only code what is documented. This same core principle applies in ICD-10. CDI programs must be continued regardless of a delay.
Coder Biomedical Training
While educating coders in the finer nuances of ICD-10 coding can be postponed, strengthening their knowledge of the basics can’t. Many coders graduated from programs 10, 15, or 20 years ago. Medical science and our knowledge of anatomy, physiology, and disease processes has grown exponentially. Now’s the time to make sure your coders are brilliant at the basics. Anatomy and physiology training should continue to be conducted: online through a service provider or at a local community college.
Computer Assisted Coding (CAC) Technology
Coder productivity is predicted to drop by 50% during the implementation of ICD-10 and perhaps remain 10-20% below normal output for ICD-9 coding. CAC systems help offset this productivity loss by electronically “reading” the record and suggesting codes to the human coder. While CAC systems don’t replace coders, they do make them more productive and efficient. The delay provides more time for organizations to evaluate and implement this technology.
Assess and Refine Your Work Plan
Conduct a methodical step-by-step review of your initial plan. This process will identify which tasks can be pushed out and which cannot. The review will also uncover other tasks that have collateral benefit for ICD-9. For each task in your work plan, ask yourself, “Does the delay impact this task?”
Industry experts are already predicting the cost of an ICD-10 delay. Other experts are predicting lawsuits by providers to help recoup monies already spent. This expert simply suggests that you stay the course and keep working toward ICD-10 preparedness. We will all have to get there eventually. Better to be early than late on this one!
Torrey Barnhouse is CEO of TrustHCS of Springfield, MO.
Viva la CPOE!
By Daniela Mahoney

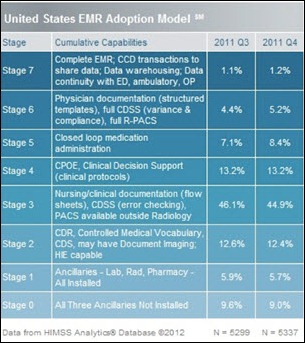
According to the HIMSS Analytics EMR Adoption Model , CPOE adoption remains steady at a rate of 13.2% for the past two quarters. And in recent months, many hospitals achieved the first stage of Meaningful Use. Congratulations to all!
However, looking at the story behind CPOE implementations reveals that adoption struggles continue —regardless of the vendor system. Many community hospitals expend great effort and many dollars meeting Meaningful Use criteria, but additional time and money is also spent avoiding a full-blown revolution within their provider community because of CPOE implementation.
Technology is really only 15-20% of a CPOE implementation. Process, acceptance, culture, and constant transformation are the parts that truly define the difference between CPOE failure and success.
At the end of the day, technology’s golden purpose is to support the infrastructure: devices, performance, remote access, integration/interoperability, streamlined single-sign-on, and ease of navigation. But even when working flawlessly, it’s still an uphill battle capturing provider adoption on that much-needed “voluntary basis.”
I can always hear the physician protests, even when left unsaid: “Why should I use it?” “What is in it for me?” “Show me the money, Jerry.”
The question remains: why? Why won’t providers embrace new CPOE technologies and take advantage of the wonderful features, such as clinical decision support or evidence-based order sets that streamline the admission process?
Truthfully, there is nothing wrong with the providers’ feelings here. They simply know what’s at stake. And the odds are not in favor of CPOE, despite the benefits we may see through our own rose-colored glasses: “Oh, how it benefits the patient! Why don’t you providers just snap out of it and embrace CPOE for the people, or at least for the children?”
Kidding aside, what a new CPOE system takes away from providers is TIME.
… at least for a while.
Time is a provider’s most precious commodity. A new system changes the way they work and takes time away from office hours and family. Time is irreplaceable and invaluable.
But the Meaningful Use mandates say “so what” and to just do it and accept it. CPOE is a reality and must be part of every provider’s future in the hospital or in the office. With that, I sympathize. Providers may have cause to rebel.
I spent some time researching literature while preparing this article, looking at provider efficiency with CPOE. Many studies are relatively old, done in the ‘90s or early 2000s. Not to dismiss their importance, but many issues experienced then have been since resolved with today’s systems. In retrospect, they really aren’t relevant.
But one thing overlooked then and now, to me, is the most important question: what is the right value proposition to the provider?
The answer? One that fits a provider’s community and meets their conditions to accept CPOE into their domain.
With 22 years invested helping providers through CPOE adoption , I found only one simple and effective system pitch. Be truthful and realistic. That’s what works. That’s what opens door and also ears.
For example, we can’t deny that it typically takes significant time to adopt and adjust to a new system, and that efficiency improves only with consistent use. Additionally, never overpromise that CPOE is faster than handwriting an order or checking boxes on a pre-printed order set. I can tell you, that approach doesn’t work.
Once providers are engaged, gather the value proposition’s building blocks by talking and listening to them – eliciting their concerns, needs, and requirements — and also identify opportunities for compromise.
Usually during interview sessions, similar things are voiced. And believe it or not, it’s less about Meaningful Use (understanding the “benefit” of hospital reimbursement is typically demonstrated by only a few) and more about the direction of technologies in healthcare and reporting requirements and how it affects the way they practice medicine.
For example, for some it is important to have remote access, and not just to CPOE, but to also do other tasks, such as signing their charts. And from others, I often hear how they would prefer using their own laptops or iPads, so they do not need to compete for devices.
Here are some very telling interview quotes from providers about CPOE adoption:
- “Access from outside of the hospital, home access would be great.”
- “CPOE should be a resource for us. It should not make us work harder to accommodate it.”
- “Ease to use and quicker order entry is most important.”
- “Online view of medications administered would be a great value.”
- “Reduces errors and provides clarity of medical orders. There must be a safety net if errors are made, especially with residents. Incorrect orders need to be stopped.”
- “A quick-pick list for providers would be nice.”
In the end, the right value proposition delivers the commitment of the hospital’s leadership to respond to what providers say and need. It engages all providers and can convince them to fully adopt CPOE as part of their workflow—especially with respect to efficiency in daily operations.
Providers become very reasonable and willing to compromise if engaged and their voices heard. Realistically, you cannot fulfill every need, but it is still important to listen and respond. The hospital’s leadership must be proactive and have a solid communication plan to manage expectations at different levels before, during, and after implementation. The direction of CPOE within the organization must be clearly defined, from the adoption and training to the deployment strategy. Lastly, completing a cultural evaluation the provider community provides tremendous insight into defining the value proposition which is the foundation of your CPOE success.
Let them eat cake, because we’re having crepes …
Here is a simple but delicious nutella-banana crepe recipe enjoyed by our family. Bon appetit!
Daniela Mahoney, RN BSN is vice president of Beacon Partners of Weymouth, MA.





Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…