Monday Morning Update 1/14/13
From The PACS Designer: “Re: TPD’s list. The latest update of my iPhone apps lists is online. In addition to many new apps is a new section highlighting the apps of HIStalk sponsors.” TPD’s list is here. He’s always up for additions to it.
From Frank Poggio: “Re: Meaningful Use Stage 4. At the January 8 HIT Policy Committee meeting, Farzard Mostashari, ONC director, waxed eloquently about MU Stage 4. Hey, wait a minute — the original playbill said this was to be a three-act play! Does he think we can stay in this claustrophobic theatre all day and night? How many more acts will there be? One thing for certain — the bonus money will run out long before the last act, but you can be sure the ‘penalty’ clauses will not. This MU theatre of the absurd must be in the Hotel California… you can check in, but you can never check out.”
From Green Space: “Re: Judy Faulkner’s new company to generate electricity for Epic. Search the Wisconsin Department of Financial Institutions for Galactic Wind. Here’s a photo of the wind farm, about 15 miles north of Epic’s main campus.”

From Dragovitz: “Re: Peake Healthcare Innovations. The image sharing joint venture between Johns Hopkins Medicine and Harris Computer appears to be defunct. Rumor has it they found it hard to differentiate themselves from PACS vendors and underestimated the risk of trying to use MINT, a protocol that would have displaced DICOM.” Unverified. The JV was created on March 2011 and their “new approach to medical image management” was rolled out at HIMSS last year.
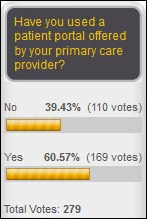
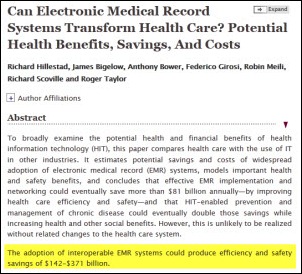
Sixty percent of us have used a patient portal offered by our PCP. New poll to your right: was the 2005 RAND study naïve, biased, decent but not useful for justifying EMR subsidies, or possibly accurate once more time goes by? Pick the best answer since you get only one.
Thanks to the following sponsors, new and renewing, that have recently supported HIStalk, HIStalk Connect, and HIStalk Practice. Click a logo for more information.
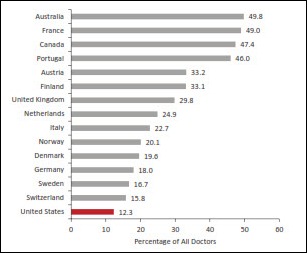
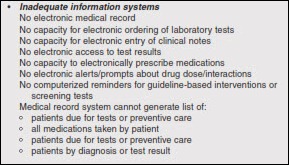
A new report commissioned by the National Research Council and the Institute of Medicine finds that despite the largest per-capita healthcare spending of all countries, the US ranks dead last among 17 developed nations in health. Most surprisingly, it’s not our also legendary number of poor and uninsured residents who are dragging our average down – our unhealthiness is equal opportunity by income and education. If you want your child to live to 50, move to another of those 16 other countries because they’re a target here for being murdered, dying in a car wreck, and not even living long enough to attend pre-school (we’re #1 in all those categories). We’re lucky that one other country beat us in the percentage of people dropping dead of heart problems and lung disease. We’re dead last in the percentage of doctors in primary care, and the graphic above shows IT as one of the “worse than average” items (the others being coordination of care, medical errors, patient dissatisfaction, and miscommunication). No single cause was identified, but it says a lot of the problem starts with being fat, overusing legal and illegal drugs, shooting each other, and wrecking cars, not to mention a healthcare non-system that’s superb at Rambo-style interventions but really bad at almost everything else. The authors found no silver bullet other than spending a lot of taxpayer money, which is another not-so-great #1 they didn’t bring up (the largest national debt at $16 trillion with the lead widening by the minute). Being rugged and self-determinant individualists, we’re not real big on public health programs in the US, so it’s ironic that excellent schools crank out thousands of public health stars who immediately head off to Africa or South America to find work despite a target-rich environment here.
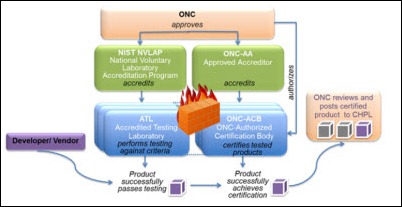
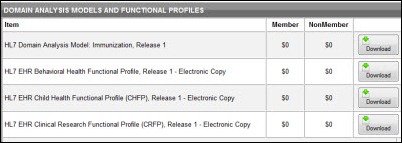
ONC announces that Authorized Certification Bodies are now authorized to test and certify EHRs using the 2014 Edition Standards and Certification Criteria.
My guilty pleasure is reading John Halamka’s “Building Unity Farm” posts on his Life as a Healthcare CIO blog. I skim his other IT-related posts on occasion, but I never miss an episode about how he uses his engineering and IT background to approach building a gentleman’s farm, like Oliver Douglas on Green Acres except he knows what he’s doing. I find myself fascinated by what kind of guinea fowl he favors, his hardwood management plan, and what was on his vegan Christmas menu.
The Illinois Department of Financial and Professional Regulation, the state’s overseer of physicians, will lay off 18 of its 26 medical unit employees next week because of a $9.6 million budget shortfall.
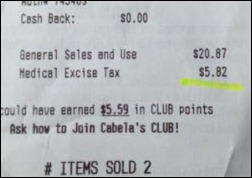
An interesting Alabama Supreme Court ruling allows patients who claim injury from a generic drug to sue the manufacturer of the brand name drug they didn’t take. The court ruled that generic drug makers are required to use the approved labeling of the patented drug, so a lack of warnings isn’t their fault. Alabama high-end real estate values will probably benefit as out-of-state trial lawyers shop second homes there.
Academic Ranking of World Universities, assembled by researchers at a university in China, ranks the world’s best clinical medicine and pharmacy universities, with US schools taking all but four spots in the Top 20, counting ties. In order, Harvard, UCSF, University of Washington, Johns Hopkins, Columbia, UT Southwestern, UCLA, Stanford, University of Pittsburgh, University of Michigan, University of Minnesota, Mayo Medical School, University of North Carolina at Chapel Hill, MD Anderson, Yale, and Vanderbilt.
BCBS’s Blue Health Intelligence acquires Tampa, FL-based Intelimedix, which offers employer and payor analytics from its medical claims database covering 110 million patients.
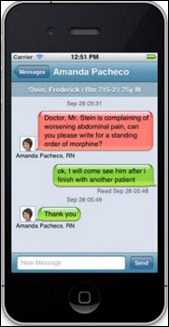
Miami Children’s Hospital receives a hospital association’s marketing award for sending urgent care wait times via text messages. The hospital uses a service from ER Texting.
RAND Corporation’s admission in a Health Affairs article that its own 2005 study predicting vast savings from EHRs was dead wrong gets major space in The New York Times, even scoring a quote from original National Coordinator David Brailer, MD, PhD, who now says HITECH was a “colossal strategic error” that encouraged providers to earn government checks by buying EHRs quickly and worrying later about actually using them for anyone’s benefit. The new analysis says the original vendor-funded report was “enthusiastically embraced,” but that now “critics of the RAND team’s analysis can claim a measure of vindication.” Some quotes from the new article:
- Lack of interoperability means systems function “less as ATM cards, allowing a patient or provider to access needed health information anywhere at any time, than as frequent flier cards intended to enforce brand loyalty to a particular health care system,“ with the huge amount of information stored by Kaiser and the VA “essentially useless if the patient seeks out-of-network care.”
- EHR adoption is still arond 40 percent instead of the 90 percent threshold RAND said was needed despite billions of HITECH payouts, which it described as, “Most of the action is concentrated among facilities that were already planning to implement or upgrade their health IT systems. Federal incentives have not yet closed the health IT gap between small, rural, and nonteaching hospitals and larger, urban, and academic ones.”
- Patients share the blame, with few of them even signing up to view their electronic records and most of those never actually looking at them.
- “Considering the theoretical benefits of health IT, it is remarkable how few fans it has among health care professionals.” The article says market forces aren’t working to demand more usable systems since comparative system information is not readily available and HITECH encourages just buying whatever’s out there anyway.
- The “do more, bill more”healthcare payment system provides no incentives to use IT to reduce costs or improve outcomes.
- The article concludes, “The optimistic predictions of Hillestad and colleagues in their 2005 analysis of the potential benefits of health IT have not yet come to pass. This is not because of shortcomings in their analysis but rather because of shortcomings in the design, implementation, and use of health IT in the United States. When the preconditions these authors posited are finally realized, the benefits they predicted will be realized as well.”
I bet most readers saw this coming when the exuberant 2005 study started putting stars in the eyes of vendors and the federal government. People who put their hopes in a tool rather than tool users are usually wrong, and it’s almost always true that those tool users will do whatever it is that they’re paid to do, like cranking out procedures, stealing each other’s profitable patients and doctors, and buying EHRs quickly without a lot of thought or commitment.
My take is that the original article was more naïve than biased. The new article, however, puts a lot of the blame on HITECH — which wasn’t implemented until four years after the original article — and not enough blame on a screwed up healthcare system whose technology reflects that unfortunate reality. A vendor could easily develop a usable, interoperable, patient-centered EHR if they didn’t have to deal with mountains of billing rules (most of them coming from the same federal government that’s complaining about complex systems), insurance companies, regulators, and market-force competitiveness, following the specifications of users dedicated to a framework of standardized and repeatable processes. They would, however, have no customers. That’s why only the VA has done it, and they developed their own VistA system having the luxury of a vacuum to work within.
The worst thing about the original RAND study is that it was quickly co-opted by special interests as validation for spending billions of taxpayer dollars to subsidize fast-tracked sales of systems to providers who had already declined to buy them with their own money. We have good providers, good electronic systems, and good patients — we just can’t seem to put the policies in place to move the needle on the marginal ones.
Vince has a great look-back this week, getting some first-hand history of Sphere Healthcare Information Systems as it eventually became NextGen’s financial system.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.




















































































The $50 billion Rural Health payout is welcome. In context, it's less than the total cost of the F22 raptor…