Ashley Womack is CEO of Aptarro, the newly renamed Alpha II.

Tell me about yourself and the company.
I started my career about 25 years ago. I was originally in corporate restructuring. I did turnaround work for companies, both in and out of court. I’ve spent most of my career in finance leadership roles.
About a decade ago, I decided to make the jump to running high-growth businesses. There’s a surprising overlap between distressed businesses and high-growth businesses. You have to make fast decisions and execute with a maniacal focus on results, which is near and dear to my heart. The important thing for us is to look for unique opportunities that may not have already been fully realized, which can cause people to either fail or grow. I find the growing part more fun than failing parts and it has been a good move for me.
Aptarro is our new brand after we brought Alpha II and RCxRules together as a software company. We help healthcare organizations break through the complexity of billing and help make it easier for people to get paid for the care that they’ve already provided.
What are the advantages of your products over those of competitors?
Our core products are around claim scrubbing and claims accuracy. The legacy product is called Claim Staker. The RCx products are revenue cycle engine and we have an HCC coding platform.
From a competitive perspective, everybody has some kind of solution for claims accuracy. Some kind. Doesn’t mean they have a good kind. They just have a kind of solution. Because we are very clearly fully focused on that little slice of the midsection of revenue cycle, we’re really good at it. We have great accuracy in terms of content and staying up to speed hourly on content changes.
We have a workflow automation tool that helps billers and coders be more efficient. It autocorrects a lot of things that we know with certainty should be changed, and helps prioritize other problems that need to be worked by people so they can stay focused on the more interesting, complex stuff and that with the biggest ROI.
From a competitive perspective, we overlap with specific point solutions, but the biggest competitor is that people just use the thing that’s the freebie that comes with their PM or EHR. Because it’s like one of a list of things, it’s not necessarily as focused on accuracy or automation as we are.
What are the most significant recent or upcoming RCM technology developments?
The revenue cycle business is ripe for technology disruption. Everybody talks about AI and other kinds of advanced learning technology. Those work best when you have a lot of complexity and a lot of volatility, which is what revenue cycle is all about.
We are focused on thinking about ways to both improve the accuracy of content, which is important for what we do, and how to be more efficient. Staff efficiency and reducing repetitive or low-value work stresses out the people who do revenue cycle and makes that job less fun than it should be. We are thinking about how to use next-level technologies to target both of those areas.
Will we see more linking of provider and payer systems to address RCM-related workflows?
Why not? That’s the issue that is frustrating to all of us just as patients. I recently had ankle surgery, and I’ve had a lot of frustrations with the healthcare system as a patient. For providers, those of us who are in the revenue cycle, and maybe or maybe not on the payer side, is it just takes too long. It’s too complex. It’s too disjointed. People are not on a level playing field.
It would be a great end state if we could figure out how to make sure that everybody has the access to the same information and the same decision-making tools. If we create more clarity and transparency, things could move faster, people could get paid more quickly and fairly for the work that’s being done, and patients could get the treatment they deserve.
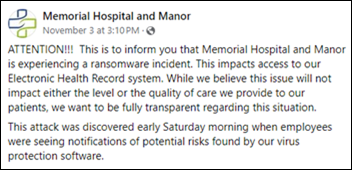
What were the lessons learned from the Change Healthcare cyberattack?
So many lessons. I have near and dear to my heart cybersecurity, governance, and thinking about making sure that we are safeguarding all of the information that we’re stewards of in this business. I’m sure that is top of mind for everybody. But if we step beyond that, it’s about making sure that you understand your technology ecosystem and avoid being too single threaded. As the buyer of these technology solutions, you have to understand what your choices are, how to make the right choices, and where you have opportunities and options.
Folks were forced to make big changes after Change. Those changes should be a little bit easier. Technologies should plug in with each other a little bit more easily and be a little bit more standardized. It goes back to the earlier point about should or shouldn’t we shouldn’t we connect providers and payers. There needs to be more standardization and a better understanding of what’s happening with the data and not relying so much on third parties.
One of the great things about our technology is that we are agnostic to which PMs or EHRs that our providers use. We can plug in anywhere. Our goal is to provide the best accuracy and the best staff efficiency regardless of what your other ecosystem choices have been.
Did it raise issues around switching costs, especially for smaller practices?
Doctors didn’t go to medical school to be IT guys or medical billers. It’s understandable that it has been a challenge. Even running a software business, making a big change like that is a challenge. To me, the lesson learned is maybe a bigger global thought about the industry. People maybe are not as forward thinking. Technology has obviously changed tremendously over the last 20 years. People have gone to more cloud -based systems. Things are a little bit easier to plug in, implement, and change.
Not all providers are quite there yet, and there are many reasons. Some of it is security reticence. Some is the cost of making the change, both the economic cost and the heartache, which is not to be discounted. But I think that folks are realizing that they need more flexibility, and with on-premise, highly complex, or highly unusual setups, it’s not as easy to make a change.
How are investor-owned provider groups using technology and doing RCM differently?
There’s not one way to do things. There are definitely pros to having a variety of types of providers in the community for different folks, but I think some lessons can be learned from those investor-backed practices. The whole reason that investors are rolling those practices up is to try to make them more efficient and make them more profitable. That’s how they ultimately make money on them. If people can leverage those same types of tactics to make their own independently owned business more efficient and more profitable, why not?
One of those is definitely around technology. How to simplify the tech stack, how to make it more efficient, and how to focus on ROI and think about making sure that you are making the right choices in vendor and choosing solutions that have a pretty clear ROI. Revenue cycle is obviously where all the money is moving back and forth. It’s important to think about you make that more accurate and faster so that your working capital cycle is shorter, you get paid more quickly, and you get paid for all of the work that you do. There are lessons to be learned there in choosing the right tech stack and getting the bang for your buck.
How do you as a company determine how to use ever-changing AI to improve administrative functions?
We have started by thinking about defining our strategy, creating governance around it, and creating a high-level, principle -based strategy around what we think AI should be doing and what should it not be doing. With medical billing and coding, and certainly around patient care, some decisions need to be made by humans Even when it comes to stuff like claims processing, claims accuracy, changing codes, and things like that, we’ve taken a big step back and thought about what we want to outsource to the computer and what we think is important to leave to human judgment.
We started with those principles to then create a map of the biggest problems that we think exist in the universe that we’re operating in and how technology can support us in solving those problems, either with better answers or less expensive answers for our customers. That’s how we are laying out an AI roadmap around what we build and how we potentially partner with other businesses that we can go to market with.
How do you as a former CFO run a business differently than someone whose background is operations, sales, or technology?
I grew up working with businesses that were in some type of transformation. Not always in distress, but some kind of transformation. Every business leader, regardless of their discipline, needs a strong foundation in understanding the finances of the business. That’s what it’s all about. How do we solve a problem in a way that is valuable to the customer and is also valuable to the business?
If you can’t get a good handle on thinking through the numbers, it’s hard to make good business decisions, good strategic decisions, good decisions about how to invest, how to grow the business, how to build new technology, how to hire new folks, how to scale. I would hope that it’s not that different because a lot of executive leaders, and certainly the best ones, are well steeped in thinking about the numbers.
I think about building a business as building a team. I’m kind of a healthcare newbie, and certainly there are challenges to that. But I think it’s really important to surround ourselves with good people who are both industry experts and experts in their discipline. Coming up through finance is a little bit unusual, but it reinforces that it takes a team to win.
What does the next three or four years look like for the company?
We’re on the doorstep of the first big change. We’ve just done a significant rebranding and, changed the company’s name to Aptarro. The purpose there was to reposition ourselves and clarify our position in the market. The businesses that we brought together have all been around for quite some time, and there are pros and cons to that. But as we are approaching this next phase, we want to make sure that people understand the problems we’re solving, which are around breaking through the complexity of healthcare billing and making it easier for providers to get paid accurately and easily for the work that they are already doing to care for patients.
This rebranding is about being able to clarify that across a couple of different offerings. We’ve brought three businesses together over the last couple of years and expect that we’ll continue to buy businesses and grow. We’re focused on that mid segment of the revenue cycle and helping make sure that claims are right and people are getting paid. That’s going to be a combination of product innovation, some of what we talked about around AI and technology, and traditional product innovation. We will be building things and potentially buying businesses and buying new products that make sense to help our customers solve the problems that are out there.
I think it’s an enduring health care trend that it’s hard to get paid. Providers did not go to medical school to become billers or coders, and that’s why we have RCM businesses. We are thinking about how we can make that easier. How do we tackle the complexity for them? The rebranding is part of that. We will continue to scale, both in terms of products offered and the rest of our footprint.
Comments Off on HIStalk Interviews Ashley Womack, CEO, Aptarro













































Fear not Epic sycophants. If real interoperability and patients owning their records on a standard uniform file that could be…