News 10/5/18
Top News
Cerner announces its VA EHR modernization team, with Leidos, Accenture, and Henry Schein taking on prominent roles as expected.
In announcing the 23 members, the company stressed that it will leverage investments already made by the DoD for its nearly concurrent Cerner-powered EHR revamp. VA Secretary Robert Wilkie and Defense Secretary James Mattis have said their departments will work together to ensure their new EHR systems are implemented on a unified schedule and are capable of seamlessly sharing data with civilian and government providers.
Cerner has promised to unveil a project timeline at its user conference next week.
I reviewed the list of companies Cerner has chosen as partners for its VA implementation. These are also working on the DoD’s Cerner implementation:
- Accenture
- Leidos
- Henry Schein
- Holland Square Group (Cerner-focused implementation consultants — acquired by Alku in December 2017)
- MedSys Group (EHR consulting)
- ProSource360 (government consulting)
These are the VA-only partners just announced:
- AbleVets (government consulting)
- ACI Federal (government IT contractor)
- B3 Group (government consulting)
- Blue Sky Innovative Solutions (government consulting
- Clarus Group (a Salesforce-focused consulting firm that offers government technology services)
- Forward Thinking Innovations (government health IT — seems to be a two-person consulting firm)
- Guidehouse (the former PwC Public Sector consulting group)
- HCTec (health IT and revenue cycle consulting)
- HRG Technologies (revenue cycle services)
- KRM Associates (government contract health IT contractor, a small husband and wife business)
- Liberty IT Solutions (government technology contractor)
- MedicaSoft (sells an EHR, PHR, and Direct messaging services with a founder who a lot of VA work with FHIR and is founder and board chair at the Open Source Electronic Health Record Alliance)
- MicroHealth (government analytics, engineering, integration)
- PM Solutions (project management)
- Point Solutions Group (consultant staffing)
- Sharpe Medical Consulting (health IT consulting, medical staffing)
- Signature Performance (revenue cycle consulting)
- ThomasRiley Strategies (consulting)
Reader Comments

From Plenary Session: “Re: UMass’s financial struggles. Isn’t this the kind of organization that has no business putting $700 million into Epic? Negative operating margins, historically financially strained … makes no sense.” The health system’s operating income has been all over the place, with capital renovation temporarily eating up some of its capacity. While I will defend my contention that a new EHR will amplify a provider’s existing levels of excellence (rarely moving a poor hospital to good), the mere act of choosing, buying, and implementing such a pervasive system (which requires more consensus and focus than many hospitals can muster) may either signal or create its resolve make overdue improvements. Epic also pushes its customers, steamrolling over incompetent or inertia-crippled hospital middle management with the full support of the hospital’s C-level, so don’t underestimate the motivational impact of your CEO demanding that you deliver $700 million worth of value in a rare example of holding executives accountable for true change and coordination across departments. In that regard, improved operational management and visibility may be a byproduct of implementing Epic, although it’s a shame that a software vendor that really doesn’t offer “management consulting” has to lead the charge against mediocrity. Still, hospitals happily pay to have consulting firms tell them what everybody else is doing, so at least an Epic implementation binds the organization to deliver measurable results. As much as we cheap-seaters might smirk about a health system spending hundreds of millions of dollars on software (and oh, I do), the fact is many of them are happy about their decision afterward and show improved results whether it’s Epic, Cerner, or Meditech.
From Expat Investor: “Re: Cornerstone Advisors. Allegations are that officials of its corporate owner 8K Miles forged auditor documents to move money to a sister company mostly owned by the CFO, who resigned.” The India-listed company’s external auditor also quit over the transfers between the companies, which share a CEO. 8K Miles acquired healthcare IT consulting and implementation vendor Cornerstone Advisors Group in late 2016.
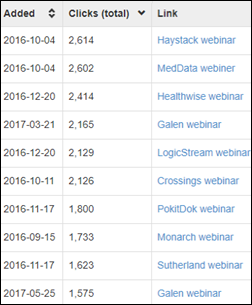
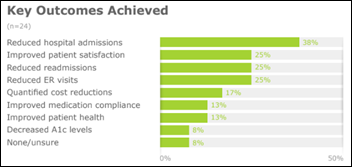
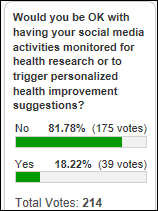
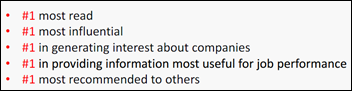
From Zeke Avarice: “Re: webinars. Why would someone watch a recording, such as on your YouTube channel?” Live webinars have just one advantage, and that’s being able to ask the presenter questions. The disadvantage is that you have to be available at the designated time, you have to pay attention at what might be an inopportune moment, and you can’t fast-forward or rewind. That’s why we archive the recording — those get more views than the live sessions due to the long tail of people discovering them after the fact. Still, we get a lot of interest in webinars (example click counts above), although the quality of the program and the speakers drive whether people actually sign up after reading the description and not everyone who signs up is able to attend (which is why we send absentees a link to the video and a PDF of the slides).
HIStalk Announcements and Requests
Welcome to new HIStalk Gold Sponsor Atlantic.net. The Orlando-based secure hosting solutions vendor provides HIPAA-compliant, PCI-ready, and cloud hosting from its state-of-the-art data centers in New York, London, Toronto, San Francisco, Northern Virginia, and Dallas. The company just won a “Best IoT Healthcare Platform” awards. Organizations choose the company – founded in 1994 in Gainesville, FL — for its 100 percent uptime SLA, its emphasis on security and compliance, and its award-winning service backed by support engineers with decades of experience, all at competitive prices. It offers the eight items required to deliver HIPAA-compliant hosting – firewall, encrypted VPN, offsite backups, multi-factor authentication, private hosted environment, SSL certificates, SSAE 18 certification, and a signed business associate agreement. Thanks to Atlantic.net for supporting HIStalk.
Webinars
October 30 (Tuesday) 2:00 ET. “How One Pediatric CIN Aligned Culture, Technology and the Community to Transform Care.” Presenters: Lisa Henderson, executive director, Dayton Children’s Health Partners; Shehzad Saeed, MD, associate chief medical officer, Dayton Children’s Health Partners; Mason Beard, solutions strategy leader, Philips PHM; Gabe Orthous, value-based care consultant, Himformatics. Sponsor: Philips PHM. Dayton Children’s Health Partners, a pediatric clinically integrated network, will describe how it aligned its internal culture, technology partners, and the community around its goal of streamlining care delivery and improving outcomes. Presenters will describe how it recruited network members, negotiated value-based contracts, and implemented a data-driven care management process.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock

Change Healthcare hires underwriters for an IPO that could value the company at up to $12 billion. The prep work comes nearly a year after McKesson CEO John Hammergren said he wanted to take the company public. McKesson owns a 70 percent stake of Change, which was formed last year through the merger of its IT business and the former Emdeon.
People

The MacArthur Foundation awards Deborah Estrin a fellowship, including a $625,000 “genius grant,” for her work on determining how data generated by smartphones, wearables, and online interactions can be used for mobile health while still maintaining user privacy. Estrin is a professor of computer science at Cornell Tech and of healthcare policy and research at Weill Cornell Medicine. She directs Cornell Tech’s Small Data Lab; and founded the Health Tech Hub at the Jacobs Technion-Cornell Institute, as well as the nonprofit, open-source software architecture startup Open mHealth.
Announcements and Implementations
Frost & Sullvan names Medicomp Systems the winner of its 2018 North America EHR Optimization Technology Leadership Award for its Quippe productivity enhancement solutions for reducing documentation burden.

Datica announces GA of its Cloud Compliance Management System for developers.
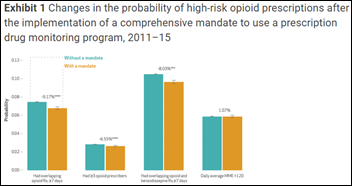
Collective Medical will deliver its real-time event notification and care collaboration tools through Appriss Health’s PMP Gateway integration software, used by the prescription drug monitoring programs of 43 states.
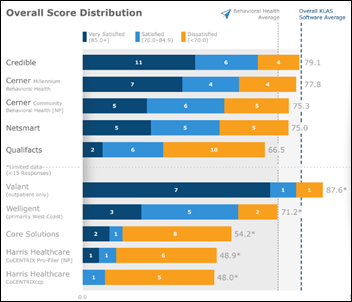
A new KLAS report says behavioral health EHRs are one of the lowest-performing segments it measures due to slow development, vendor over commitment, and state-specific reporting needs. Still, frustrated customers are likely to keep their existing systems due to lack of money and competitive alternatives. Valeant would have topped the list (over Credible and Cerner, which has two offerings in Millennium and its acquired Anasazi) had it generated enough responses. No vendor scored above a 7 in “keeps all promises.”
Buoy Health, which offers an AI-powered chatbot, wins the Robert Wood Johnson Foundation’s AU Challenge Award for patient education. I’m not really a fan of the many available online symptom checkers and I’d like to see their results validated against a an actual visit with a clinician, but this one seems OK if you like them. Startups obsess over the problem they think exists in misdiagnosis or underdiagnosis, packing PCP offices and EDs with people who need more information, have been given bad information by the computer, or who can’t afford further diagnostic work or treatments anyway. We have endless problems with our healthcare services delivery and social policies, but not diagnosing enough symptom-free problems doesn’t top the list.
Privacy and Security
Scripps Health patient Danielle Sullivan tells the local news the health system has sent her the medical records of other patients three times in the last seven months. She has filed an HHS complaint but expects no change since Scripps hasn’t apologized and she thinks they just treat mistakes as a cost of doing business.
Other

Healthcare celebrity Atul Gawande, MD will keynote HIMSS19 on Tuesday, February 12 in Orlando.

Stat digs into the business case behind Mindstrong, a predictive mental health app that’s high on hype but low on clinically valid results. Founded by Paul Dagum, MD, the Silicon Valley startup has raised $30 million in funding and secured implementation agreements with a dozen California mental health departments, but has yet to publish peer-reviewed data that back up its claims. With the Theranos fallout barely out of the headlines, industry analysts have been quick to pump the brakes on panacea-like expectations and the company itself has said the app will be rolled out with caution.
Police in San Jose, CA use a combination of video surveillance footage and Fitbit data to charge Anthony Aiello with the murder of his stepdaughter. Investigators say her Fitbit shows her heart rate spiking, rapidly slowing down, and then ceasing at the same time neighbors say Aiello was visiting. After being confronted with the data, Aiello said, “I’m done.”
Sponsor Updates
- Frost & Sullivan honors Medicomp Systems with the EHR Optimization Technology Leadership Award for its Quippe suite of solutions.
- FDB and PetIQ develop the industry’s first veterinary medications database that will deliver codified, up-to-date information on pet medications, structured for integration into pharmacy systems.
- Elsevier Clinical Solutions will exhibit at the College of American Pathologists meeting October 8 in Chicago.
- EClinicalWorks will host its 2018 National Conference October 5-7 in Nashville.
- Healthwise and Imprivata will exhibit at the Cerner Health Conference October 8-11 in Kansas City, MO.
- Lutheran Senior Services (MO) becomes the first Netsmart customer to exchange health data with its local health system through the Carequality framework.
- EClinicalWorks and Healthfinch will exhibit at the AAFP Family Medicine Experience October 10-12 in New Orleans.
- EPSi will host its Visis National Summit October 10-12 in Amelia Island, FL.
- FormFast will exhibit at ASHRM 2018 October 7-10 in Nashville.
- CHIME interviews The HCI Group CEO Ricky Caplin.
- Hyland will exhibit at AHCA/NCAL 2018 October 7-10 in San Diego.
- InterSystems will exhibit at the DoD/VA Gov Health IT Summit October 10-11 in Alexandria, VA.
- Kyruus will exhibit at SHSMD Connections 2018 October 7-10 in Seattle.
- Surescripts honors five EHR vendors with its 2018 White Coat Award for improving e-prescribing accuracy.
- Pivot Point Consulting parent company Vaco hires Phillip Noe (The Adecco Group) as CIO.
Blog Posts
- Enhancing the User Experience with Encrypted Push Notifications (PMD)
- The Impact of Informed Consent – Part 2: Satisfaction (FormFast)
- Want to Ensure Greater Compliance? Look at Things from a Provider’s Point of View (Hayes Management Consulting)
- Top 5 Nonprofit Healthcare Organization Troubleshoots and Resolves Issue Impacting Meditech Users with Goliath Performance Monitor (Goliath Technologies)
- Clarity on Artificial Intelligence and Patient Privacy (Iatric Systems)
- 5 Keys to a Successful Healthcare IT RFP (Influence Health)
- Innovating Our Way to High-Resolution Healthcare (InterSystems)
- A Series on Chatbots: Leveraging Technology to Meet Consumer Expectations (Kyruus)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.










































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…