News 7/17/19
Top News
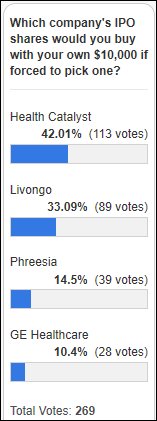
Livongo Health’s revised IPO filing values the diabetes management technology company at up to $2.4 billion.


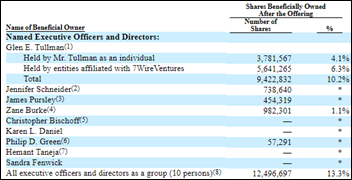
Livongo shares that are owned by founder Glen Tullman and his venture firm are potentially worth over $200 million. CEO Zane Burke – who joined the company in December 2018 after seven years as president of Cerner – holds shares worth up to $23 million.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor TransformativeMed. The Seattle-based company offers the interface-free, MPages-embedded, Saas-based Core Workflow Suite that turns Cerner Millennium into a modern, workflow-focused EHR that adapts to the way a doctor practices. The company — which was founded in 2011 and just completed a $6 million Series A funding round — has 120 large-hospital customers, including big names such as Ascension, Dignity Health, Tenet Health, and MedStar Health (which just renewed its contract and signed on as an innovation partner). Apps within the suite include Core Work Manager (automating scheduling of multidisciplinary rounds, results tagging for dynamic documentation, assessment and plan management, “discharge before noon” workflows, and workflow-integrated handoffs); Core Notify (continuous EHR monitoring with real-time notifications, configurable notification rules, and one-click result to task follow-up); and Core Messaging (secure texting with image sharing, convert messages to EHR task, care team messaging directly from the chart, and on-call schedules). It offers workflows for specific conditions like diabetes that include patient lists, flowsheets, advanced ordering, safety alerts, and decision support. A Seattle Children’s doctor says, “This ability to customize is a huge benefit for us. It’s made our handoff processes both faster and safer. As medicine becomes more of a shift-work model, and we don’t have these crazy 36-hour shifts anymore, we have more handoffs. More handoffs mean more opportunities for things to fall through the cracks. You must have a really robust tool to control for that. For us, that’s Cores.” Thanks to TransformativeMed for supporting HIStalk.
The industry lethargy created by the slow summer months (aka “The Doldrums”) motivates me to find new sponsors to replace those that have sold out, gone broke, or assigned an unresponsive marketing person as our only contact. Contact Lorre for a deal on webinars, new sponsorships, and a special offer for success-focused start-ups that are anxious to let the health IT world know they are out there. I like to think of this as my Temporary New Operating Model.
Volunteers help me review the recorded rehearsals of upcoming HIStalk-produced webinars (the videos are usually 30-40 minutes long) to offer the presenters suggestions about content, delivery, etc. I gratefully send them a $50 Amazon gift card in return. Let me know if you work in provider-side IT management and can help out occasionally.
Listening: new angry but melodic punk from Bad Religion, which punches hard for a band whose 40th anniversary is next year and whose 54-year-old, Madison-born singer Greg Graffin has a PhD in the history of science, lectures at UCLA, and wrote a book titled “Population Wars: A New Perspective on Competition and Coexistence.”
Webinars
July 18 (Thursday) 2:00 ET. “Healthcare’s Digital Front Door: Modernizing Medicine’s Mobile-First Strategies That Are Winning Patient Engagement.” Sponsor: Relatient. Presenters: Michele Perry, CEO, Relatient; Michael Rivers, MD, director of EMA Ophthalmology, Modernizing Medicine. Providers are understandably focused on how to make the most of the 5-8 minutes they have on average with a patient during an exam, but what happens between appointments also plays a significant role in the overall health of patients. Modernizing Medicine is driving high patient engagement with best practice, mobile-first strategies. This webinar will describe patient engagement and the challenges in delivering it, how consumerism is changing healthcare, and how to get started and navigate the patient engagement marketplace.
July 25 (Thursday) 2:00 ET. “Meeting patient needs across the continuum of care.” Sponsor: Philips Population Health Management. Presenters: Cindy Gaines, chief nursing officer, Philips Population Health Management; Cynthia Burghard, research director of value-based healthcare IT transformation strategies, IDC. Traditional care management approaches are not sufficient to deliver value-based healthcare. Supplementing EHRs with advanced PHM technology and a scalable care management approach gives health systems proactive and longitudinal insights that optimize scarce resources in meeting the needs of multiple types of patients. This webinar will address the key characteristics of a digital platform for value-based care management, cover the planning and deployment of a scalable care management strategy, and review patient experience scenarios for CHF and diabetes.
July 31 (Wednesday) 1:00 ET. “Modern Imaging Technology for the Enterprise: Mercy’s Approach That Improved Imaging Cost, Speed, Capacity, and Care Quality.” Sponsor: Mercy Technology Services. Presenter: Jim Best, executive health IT consultant, Mercy Technology Services. Enterprise imaging has become as critical as EHRs for transforming patient care, but many health systems are struggling with the limitations and costs of dated, disconnected PACS even as imaging volumes grow and radiologists report increasing levels of burnout. Radiologists at Mercy were frustrated by its nine disparate PACS, which required them to toggle between workstations, deal with slowdowns and poor reliability, and work around the inability to see the complete set of a patient’s prior images, even as demands for quick turnaround increased. In this webinar, MTS — the technical backbone of Mercy — will describe the lessons they learned in moving to a new best-of-breed PACS platform that increased radiology efficiency by 30%, with the next phase being to take advantage of new capabilities by eliminating third-party reading services and distributing workload across radiology departments to improve efficiency, capacity, and timely patient care.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Sales
- Philippines-based, two-hospital St. Luke’s Medical Center chooses Allscripts Sunrise.
- Eight Prime Healthcare hospitals in California join the non-profit Manifest MedEx HIE, joining the seven Prime hospitals that are already members.
- The Reliance EHealth Collaborative is deploying the virtual health record of Imat Solutions to enhance provider engagement and to add claims and pharmacy fill data for care coordination.
People


Clinical decision support vendor EvidenceCare hires Shawn Kircher (Idemia) as CTO and Steve Starkey (Medhost) as CIO.

Tom Neufelder (Philips) joins MaxQ AI as CTO.
Announcements and Implementations
In England, NHS’s digital service manual team will hold a show-and-tell Thursday on YouTube (and live in London) to describe its work so far in developing design principles, accessibility, content style, user interface style, and prototyping. That’s a 6 a.m. ET start for US YouTube live-streamers, although I expect they will archive the video.

Optimum Healthcare IT completes the Epic go-live of North Mississippi Health Services.
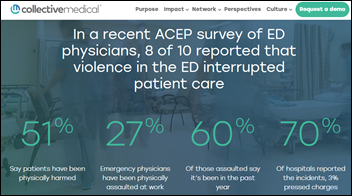
Collective Medical’s care collaboration platform will alert providers when a patient who has a documented history of threatening or assaulting other providers presents at a hospital, ED, or other point of care.
SimplifiMed goes live with its NextGen-integrated chatbot that allows providers to engage patients (appointment reminders, recall, no-show follow-up, reviews) via two-way SMS in over 100 languages.
Government and Politics
India’s health ministry publishes a draft of its National Digital Health Blueprint for public comment, proposing to use the government’s identifier for healthcare and giving citizens access to their heath data within five clicks. The government also hopes to publish de-identified data from its new health insurance program as it moves toward universal health coverage.
Other
UCSF researchers post an open protocol describing how they plan to study the effectiveness a particular treatment, which is notable because (a) it uses the Protocols.io open collaboration platform to create and manage the protocol and to solicit feedback; (b) it spells out in detail how UCSF plans to extract information from Epic to perform the study; (c) the study will be performed using EHR data; and (d) the completed protocol can be downloaded and used by any other organization.
Memorial Sloan Kettering Cancer Center researchers find that unsupervised AI that looks only at whole slide pathology images and patient diagnoses can accurately identify the 75% of slides that do not require manual annotations. Recent work on unsupervised AI has delivered fascinating results in simply letting the machine “learn” by figuring out the data thrown at it rather than having a human tell it what to look for.
In Sweden, a self-guided drone completes its first delivery between two hospitals, choosing its landing spot visually at the end of its three-mile journey since the courtyard is between tall buildings and is thus GPS-denied (not mapped by GPS).
I missed this a couple of weeks ago. A new Florida law that took effect July 1 allows out-of-state doctors to conduct virtual visits with in-state patients for a one-time $150 registration fee. As a result, Humana has launched a telemedicine-heavy health plan for Florida residents that reduces premiums by 20%, provides free video consultations, and raises the co-pay for office visits. MDLive’s Lyle Berkowitz, MD was quoted as saying that virtual visits are like Netflix compared to the Blockbuster-like experience of going to a doctor’s office.
Sponsor Updates
- Atlanta-based Advanced Technology Development Center will offer startups in its health technology program access to Redox’s integration platform.
- Health IT reseller Microwize Technology offers Aprima EHR and practice management software from EMDs.
- CoverMyMeds will exhibit at Integrated 2019 July 22-23 in Philadelphia.
- Diameter Health will exhibit at the NCQA Digital Quality Summit 2019 July 16-18 in Boston.
- Docent Health publishes a new report, “Patient Navigation: Leading the New Wave of Healthcare Consumerism.”
Blog Posts
- Is the Juice Worth the Squeeze? How to Justify an EConsent Solution for your hospital (Access)
- Why patient experience matters in healthcare collections (AdvancedMD)
- Top 5 Ways to Speed Up a Slow Website (Atlantic.Net)
- Innovation is a Matter of Mindset (Avaya)
- Our take on D&I: A word from our Chief of Staff (Bluetree)
- Want enterprise-level talent and productivity? Focus on integrated collaboration technology (Burwood Group)
- CMS Seeks to Improve Patients Over Paperwork Initiative 2019 (ChartLogic)
- Informonster and Sparky the FHIR Dog Go To DevDays (Clinical Architecture)
- Hot Topic: Skyrocketing Pharmaceutical Prices (Dimensional Insight)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.























































I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…