Chris Klomp, MBA is CEO of Collective Medical of Cottonwood Heights, UT.

Tell me about yourself and the company.
I’m the CEO of Collective Medical. We are based in Salt Lake City. We operate the leading real-time care activation alerting and collaboration platform in the country. Our objective is to stitch together otherwise disparate hospitals, health systems, post-acute, clinics, primary care, specialty care, accountable care organizations, health plans, and others to understand where patients travel in real time, identify those who are facing imminent but avoidable risk, and then activate the most appropriate stakeholders to intervene on behalf of that patient to prevent this bad thing from happening to him or her.
We are in use by over 1,000 hospitals and health systems and several tens of thousands of other providers of varying types, including every national health plan in the country, loads of regional plans, and accountable care organizations.
The results are pretty extraordinary. We start with ADT data, but we augment that data with all sorts of incremental data types. Not for purposes of moving that data from point A to point B, which we think is the provenance of health information exchange, but instead leveraging that information in a secure and privacy-compliant manner to help providers intervene with those patients whose needs may go unmet.
Our objective is to improve patient-specific outcomes at the lowest possible cost. We find a tremendous amount of opportunity in the face of medically unnecessary, avoidable utilization.
How will the 21st Century Cure Act’s push for interoperability and ADT notifications affect health systems and medical practices?
A number of provisions within the rules are exciting. We are particularly focused on the recently modified Conditions of Participation, which require hospitals in their several forms, principally acute hospitals and critical access hospitals, to make downstream providers — primary care providers, post-acute facilities, and skilled nursing facilities — aware that a patient has been admitted or discharged. That’s a benign and simple ask, and yet it’s powerful.
We and others already facilitate this type of information awareness. But if you think about it in its most essential form, we as a country charge primary care providers with quarterbacking the care of their patients and coordinating that care across specialists in different acute and post-acute settings. Yet it’s as though we have been tying at least one, if not two, hands behind their backs while expecting them to call the play and throw the ball. They don’t even know when their patient is sitting in a hospital or why, and therefore they are not well positioned to intervene.
These rules are designed in a lightweight manner, right now with not much of a stick, for hospitals to just try a little bit harder to do more to help downstream providers coordinate care more effectively, to take the handoff from the hospital in a timely manner. I’m sure there will be more to come, where over time, additional data will be required to be shared, perhaps discharge plans, test results, or others. Penalties will probably be instituted, so that stick may get a little bit bigger. But the carrot is also getting bigger as we increasingly shift toward value-based care arrangements. All of this is in the spirit of collectively caring for patients, collectively caring for our most vulnerable members in the community.
This is highly aligned with the strategy that we have been pursuing as an organization for many years. Our name is not by happenstance. We believe that in the concept of better together, as care teams collectively care for one even if they represent different organizations or have never met one another, they are united by their common stewardship for that single patient in that moment. That requires some level of data and clinical interoperability to align their efforts in the most efficient and effective manner.
The rules are simply trying to remove a few barriers and provide a little bit of additional encouragement, in a light-touch manner, for hospitals and providers do this more effectively. We are excited about that.
What care coordination challenges or needs will be driven by the adoption of telehealth?
We have observed as a country this massive, singular, step-change function, where we shuttered brick and mortar care. I needed to go to a physician recently. All was fine and it wasn’t a big deal, but at the time, it was reasonably urgent and not something that telehealth could appropriately address. I had to pull out all of my powers of persuasion and negotiation to get seen by a provider in person. My family and I have been fortunate to be able to strictly self-quarantine over the last couple of months, and while recognizing that not everybody has that advantage, we were able to make that attestation. The provider acquiesced and agreed to see me and I was grateful for that.
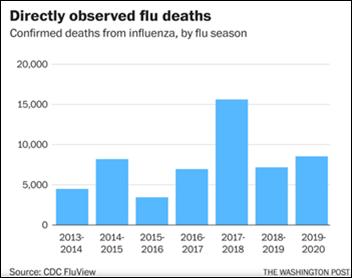
Broadly as a country, hospital revenue is down between 40% and 70% because volumes are down. It is not just electives that have been postponed, but also anything that is essential but non-urgent. Some of that it is being pushed to telehealth, but emergency and inpatient volumes are significantly down.
I would not have expected this step-change function to have occurred without massive external or forcing function externality, and yet it has. It is showing us that many things can be done remotely. Telehealth is here to stay in a much more significant way.
As a result, sending a bunch of faxes and working the phone lines with telehealth providers is not a scalable or cost-effective solution. That puts more emphasis on the need for not just technical interoperability — to get the data to those providers who are not necessarily connected directly to an originating provider’s office, hospital, or health system — but to also also understand what they are recommending and doing. Then, drive that workflow back to the community, to whoever is going to pick up the ball and continue to provide care for the patient, both virtually and in a brick-and-mortar location. It’s both technical and clinical interoperability.
At the same time, I worry, even in the absence of good data or studies, that if you postpone something that needs to be done, it often gets worse and more costly. If you have been diagnosed with cancer or are delayed getting a mammogram, the longer you wait, the harder it is to treat. I worry about that. We have no data, so we don’t know the implications. If this lasts just 60 to 90 days, hopefully the damage will not be particularly acute, and telehealth will have been able to fill that gap along the way. Clearly they are seeing their volumes surge as a subsector. But if we continue to have waves of the pandemic and a vaccine doesn’t come into play, we may find that we have a bigger issue as a country, which is worrisome.
Governments and public health experts are trying to manage the pandemic with voluntarily emailed hospital capacity worksheets. What would be the benefits and challenges involved in providing a real-time view of cases and capacity?
I don’t think that the federal government needs an identified surveillance system that understands where individual patients are going, why they are there, and what care they are receiving. That feels like a big brother surveillance state that as a country, certainly as a citizen and as a patient with my own patient rights, I don’t want. I don’t think that we as a country need that. I have not heard anyone at the state or federal government level ask for an identified surveillance system, and certainly we are pretty close to a lot of folks in state and federal government.
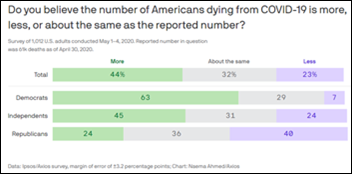
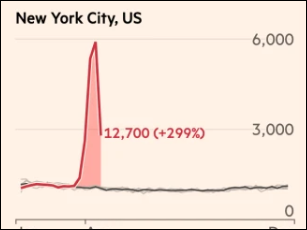
The ask has been for a de-identified solution that would allow not just capacity planning, but real-time evidence of what is happening with disease’s progression. As we ramp up the volume of testing, it will look like we have a second wave of the pandemic. That will lead to all sorts of potentially poor policy decisions, because we now think that there’s an onslaught, when in fact there is not. Nothing has changed except our improved ability to measure.
If you can’t rely on testing until it’s at some sort of a steady-state stasis, with sufficient scale to accurately depict the representation of the infection fatality rate and case fatality rate, what then might you use as a proxy? ADT data is incredibly valuable in that regard. We can understand in true real time — on a de-identified basis that fully protects patient rights or that is even rolled up to the metropolitan statistical area or state level – if we are seeing increased or decreased volumes of both suspected and confirmed cases. We can pull in the lab data to augment this ADT data, which we are doing for a collective of several states across the country on a de-identified basis.
This is not surveillance, but rather simply an aggregate macro view of what we are seeing from a trending perspective. It allows public policy leaders to make decisions about how to allocate scarce resources, such as ventilators and beds.
What is an entirely unacceptable and insufficient manner would be collecting things by paper, email, and Excel file. There are systems in place right now, including in government, that are trying to rely on that information. The resulting information is, at best, patchy, incomplete, and delayed by many days. We are hearing this from government leaders.
Just like we said about primary care providers having their hands tied behind their back, imagine being a policy leader. You are trying to decide if you should ease social distancing, reopen restaurants, or start to widen the aperture of what constitutes an essential business, because you are also worried about people starving out from massive economic decline. Yet you have, at best, a patchwork set of data that is not representative of what is actually happening with this hidden enemy. That’s a really difficult position.
You could make better decisions with a a highly privacy-compliant solution that has nothing to do with individual surveillance, but that instead shows de-identified, aggregated suspected and confirmed cases with an accurate denominator of total volumes presenting to an emergency department or inpatient care setting. That’s what is being asked for by folks in federal and state government. As a citizen, that makes me feel a lot better.
Do you have any final thoughts?
The pandemic marks a turning point in healthcare along many dimensions. It has many silver linings. States will be better enabled to build public health infrastructure that we previously could only dream of. We have a catalyst to understand the importance of this and to understand the importance of preparation.
We need to align on a set of clear objectives. Those should obviously be patient safety and outcomes, provider safety, and guiding public health response to inform policy to allocate scarce resources broadly. But the very nature of our response is showing the entire country the need for a more comprehensive and logically tuned health IT infrastructure that works together and is not operating in silos, whether it’s data silos, provider silos, or equipment provider silos. As a country, we need to come together. Slowly, I think we are starting to see that, even though we’ve had some gaps in our response efforts.
I’m hopeful that we will make the changes we need to make once we move past the acute or attenuated point of this crisis. A vaccine may not be our answer. We may go back to old-fashioned masks and social distancing to starve the disease out. Regardless, we need good data to understand how to proceed. That will happen only if we come together and continue to work on things such as what is being promulgated in the 21st Century Cures Act.
I’m hopeful. I’m optimistic. We are a country that tends to rise together in times of crisis. I have no reason to believe that this will be any different. We are certainly seeing evidence of that across the country with all of the stakeholders with whom we partner.
Comments Off on HIStalk Interviews Chris Klomp, CEO, Collective Medical









































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…