EPtalk by Dr. Jayne 6/11/20
CMS Administrator Seema Verma blogged for Health Affairs last week, sharing a discussion of CMS payment model flexibilities that stem from COVID-19.
The healthcare system in the US was broken to begin with and the pandemic has pushed many organizations past their breaking points. Many of my physician colleagues have retired, closed their practices, or been downsized by their employers in the name of cost savings. Hospitals and health systems have laid off countless employees from everywhere in the process. Very few job classifications have been spared, and I suspect we’ll see a number of CEO, COO, and CFO heads start rolling before long.
Although it was a well-written read, I was disappointed that it mostly rehashed the changes that have been ongoing for the last several years in attempting to transition us from a fee-for-service to a fee-for-value model. She mentions the concept of providers taking financial risk as “the cornerstone of value-based care,” but over the last few months, most providers have figured out that financial risk is the cornerstone of all of fee-for-service as well. Plenty of providers and hospitals who counted on a certain number of procedures or encounters have been hobbled, if not sent to bankruptcy. It’s not clear if they would have been better off under value-based care arrangements since they don’t fit every specialty and situation. Verma notes that such arrangements “provide stable, predictable revenue,” but that doesn’t really apply to urgent and emergent care situations or unpredictable needs for things like cancer surgeries.
She goes on to talk about flexibilities CMS is adding, but a quick look at the summary table shows that many of the changes are extensions of existing models or delays to the start of upcoming or changing models. A handful of models have changes to their financial methodologies. Verma also mentions flexibilities with telehealth, which I hope become permanent. Nearly every patient I’ve spoken with has been happy with their telehealth visits and not having to experience the hassle of visiting an office.
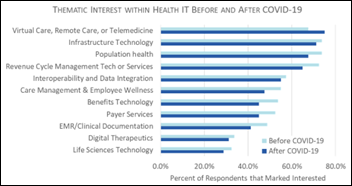
Congress is paying attention to telehealth, with a bill recently introduced that would require HHS to study how telehealth has been used during the pandemic and to deliver a report back to legislators within one year after the emergency ends. The bill is HR 7078, the Evaluating Disparities and Outcomes of Telehealth During the COVID-19 Emergency Act of 2020.
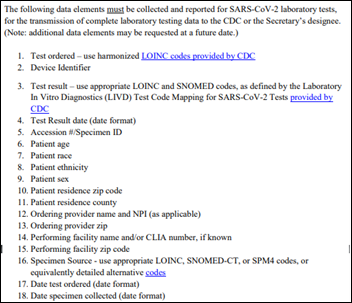
I didn’t have time to dig deeply into the federal register since I’m in the middle of a couple of big projects, but I’d be interested to see how they define telehealth and how data points would be gathered. Many physicians I know haven’t been using proper billing codes while they deliver telehealth, instead performing what is essentially a free visit in the name of ensuring patients are cared for. Some of the major telehealth vendors don’t use standardized billing codes, especially if they offer a direct-to-consumer option. The bill would require analysis of the types of telehealth platforms used as well as the locations where care was delivered (hospital, physician office, health clinic, private home, etc.) I wonder how they would classify the RV flying down the highway, which was my patient’s location the other night.

ONC announces its all-virtual Tech Forum for August 10-11, 2020. Sessions will include a mix of keynotes, panel discussions, and breakout sessions. The full agenda isn’t available, but I registered anyway. How can you not like a conference that gives you more than an hour for lunch plus two 30-minute breaks and you can do it all from the comfort of your own home? Get your fuzzy bunny slippers ready and I’ll see you there.
News of the weird: A surgery professor in California leverages telehealth and maggots to treat a patient’s wound, saving his limb and likely his life. David Armstrong, DPM, PHD is co-director of the limb salvage program at the University of Southern California Keck School of Medicine. The maggots in question, which he refers to as “nature’s microsurgeons” are larvae from the common green bottle fly. The patient had experienced tissue death after a surgical procedure, but also had diabetes and recurrent pneumonia and was high risk for an emergency department visit due to COVID-19; the necrotic tissue in his arm placed him at high risk for sepsis. Armstrong shipped a package of larvae to the patient then instructed a home care nurse via video on how to apply the larvae and dress the arm. Two days later, they used a telehealth encounter for a dressing change. After another course of treatment, the necrotic tissue was reduced from 46% to less than 1%.
I worked with the best scribe this week. He was geeking out on ICD-10. With the nice weather and lifting of stay-at-home orders, we’ve been seeing plenty of orthopedic injuries and trauma. At the end of the day when reviewing and signing my notes, I was glad to be surprised by entries that went well beyond the usual sprains, strains, and lacerations:
- W29.3XXA Contact (accidental) with hedge-trimmer (powered).
- Y92.832 Beach as the place of occurrence of the external cause.
- Y93.G2 Activity, grilling and smoking food.
- Y92.828 Other wilderness area as the place of occurrence of the external cause.
My recent shifts haven’t been much to smile about, so I was glad for the distraction. Needless to say, I rewarded him handsomely via our on-demand bonus system. He’s leaving soon for medical school, so he’ll definitely need the extra dollars.
Although emergency physicians aren’t expressly there to deliver preventive care, I’d like to offer some guidance based on my recent experiences. First, if you’re going to be using an electric hedge trimmer, may I suggest not “rushing to beat the heat of the day” and also wearing a pair of sturdy work gloves. Second, if you’re going to engage in a beach barbecue, follow the instructions on the charcoal lighter fluid and don’t squirt it on the coals beneath the already-cooking food. Third, if you’re going to use the hunting knife you just sharpened to open the cheese and sausage packages on your picnic table, please wear shoes. That’s a wrap on today’s safety moment, folks.
What’s your favorite summertime ICD-10 code? Leave a comment or email me.
Email Dr. Jayne.








































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…