December 2022
Canada’s Niagara Health will implement Oracle Cerner. (12/17/22)
Crook County Medical Services District (WY) will implement Cerner in replacing CPSI, which it says is a bottleneck to productivity, has created cash flow issues, and has tied up nurses by “wanting to know what someone’s shoe size is.” (12/17/22)
DHA Tidewater Market facilities in Virginia including Naval Medical Center Portsmouth, Air Force 633 Medical Group, and McDonald Army Health Center prepare to implement MHS Genesis, an Oracle Cerner system, next month. (12/14/22)
Oracle reports Q2 2023 results: revenue up 18%, EPS $1.21 vs. $1.18, beating Wall Street expectations for both. Oracle’s Cerner unit contributed $1.5 billion to the company’s quarterly sales of $12.3 billion. Oracle shares have seen a 33% increase since October 1. It acquired Cerner in June for $28 billion. From the earnings call:
-
Total revenue grew 9% even without Cerner’s contribution.
-
Cloud revenue was up 48% including Cerner and 25% without.
-
CEO Safra Catz says that five months post-acquisition, Cerner is performing better than Oracle projected.
-
CTO and chairman Larry Ellison said that while Cerner and Epic mostly automated hospitals, Oracle wants “to do national public health.” He added that several countries will be signing contracts with Oracle to build national healthcare early warning systems, concluding that “we, as humanity, have to do a better job of delivering healthcare to people than we have done historically.” (12/14/22)
The VA plans to hire 1,000 new employees to work on its Oracle Cerner implementation as it recruits from Silicon Valley. (12/12/22)
Marshfield Clinic Health System (WI) lays off its 18-employee telehealth department and shuts down the service, citing system-wide financial challenges. The health system launched the telehealth service in 2001. Primary care staff will take over the team’s duties, with IT absorbing the technology functions that include several telehealth platforms. The system has been transitioning from its 30 year-old homegrown Cattails EHR to Cerner over the last year. Marshfield Clinic said in its Q2 2022 report that the move to Cerner, in a project called One System EHR, has caused “greater disruption to reporting and revenue cycle billing and collections than anticipated and the realization of expected benefits from the system has been slower to materialize.” (12/7/22)
November 2022
Adventist Health Mendocino Coast (CA) will go live on Oracle Cerner December 1. (11/30/22)
Australia’s NSW Health chooses Epic to replace nine EHRs, six patient administration systems, and five pathology laboratory information systems to create a Single Digital Patient Record for the state’s public health system. Epic will displace Oracle Cerner and Orion Health for the EHRs, Oracle Cerner and DXC for PAS, and Citadel and OmniLab for LIMS. (11/28/22)
Labcorp will use Oracle Cerner’s laboratory information system to help manage the lab operations of a Catholic health system. (11/16/22)
The Bermuda Hospitals Board celebrates the arrival of the first baby with an entirely digital health record. Frances Ivy Edwards was born shortly after the King Edward VII Memorial Hospital and the Mid-Atlantic Wellness Institute went live on the Oracle Cerner-based Patient Electronic & Administrative Records Log (PEARL). (11/16/22)
Hugh Chatham Memorial Hospital (NC) will implement Oracle Cerner’s EHR via the CommunityWorks model. (11/11/22)
Clinical and IT staff at Fox Army Health Center (AL) are working through several issues that are associated with the facility’s September rollout of MHS Genesis, including intermittent access to the cloud-based messaging system and eventual online appointment booking and a backlog of medication requests that have put prescription fulfillment at 72-plus hours. (11/9/22)
A Madison, WI-based non-profit news site runs a well-written piece on Epic. Snips:
- Epic walked away gracefully from its $624 million VA patient scheduling pilot programs when the VA chose Cerner in a $16 billion no-bid contract, which may benefit Epic in the long run since Epic has since enhanced its market position instead of bogging down in government work.
- Epic has 12,500 employees and $3.8 billion in annual revenue versus Cerner’s 27,000 employees and $6 billion in revenue, but Cerner continues to lag product-wise, is losing premium customers to Epic while selling mostly to price-sensitive ones, and was laying off employees when Oracle pursued its acquisition.
- Epic has built all of its products and they integrate well, while Oracle Cerner grew by acquiring unrelated products that were bolted together.
- Epic says it’s too early to say if it will collaborate with Oracle Cerner on the national database of patient records that Oracle Chairman Larry Ellison has announced, with Epic saying that connecting to Cosmos can’t happen until Epic gains understanding about the reliability of Oracle Cerner’s data, its method of de-identifying patient data, and its willingness to legally agree not to sell patient data commercially.
- Observers say that Oracle Cerner prospects may be spooked by Cerner’s history and the Oracle acquisition and may buy Epic instead.
- Oracle has a history of making grand promises about developing new products when acquiring companies, but the end result is usually only that Oracle tries to sell more of its existing products to the acquired customers. (11/7/22)
Oracle will close the former Cerner world headquarters and its Realization Campus in Kansas City, MO, consolidating employees from those locations to its Innovations campus as it reduces its footprint as the city’s largest private employer. (11/2/22)
The local paper covers the planned Epic go-live of Albany Med Health System (NY) in 2024. I think that Albany Medical Center and maybe others in the group are using Allscripts, while Glen Falls Hospital had big revenue drops and layoffs in 2018 following its “catastrophic” rollout of Cerner, which resulted in a lawsuit that was settled. (11/2/22)
October 2022
National Oceanic and Atmospheric Administration confirms that it plans to go live on Oracle Cerner next year, although under the Department of Defense’s MHS Genesis project rather than the VA’s as initially reported. NOAA has 24 clinicians. (10/31/22)
A VA official says that the 12,000-employee National Oceanic and Atmospheric Administration may join the VA’s Oracle Cerner project. (10/28/22)
Penn State Health’s Milton S. Hershey Medical Center goes live on Oracle Cerner. (10/26/22)
The VA awards Oracle Cerner $956 million worth of task orders to continue its rollout. (10/26/22)
Oracle co-founder and CTO Larry Ellison tells CloudWorld 2022 attendees that the company will partner with other companies to build next-generation healthcare applications, saying that “there’s no way we can do this by ourselves.” Ellison again touted creation of a national health records database, warning that healthcare costs will bankrupt Western civilization unless efficiency is improved. He added that acquiring Cerner was “maybe the single most important thing we did in terms of expanding our own capacity.” (10/24/22)
Oracle EVP Mike Sicilia tells Oracle Cerner Health Conference attendees that healthcare is Oracle’s highest priority and primary mission. Oracle Cerner also previewed its Advance dashboard, says that its Seamless Exchange integration product is nearing release, and highlighted its RevElate patient accounting solution that will be released in the next few weeks. (10/19/22)
A KHN article says that federal law requires that government resources be accessible to patients with disabilities, but the VA’s Oracle Cerner system doesn’t support blind or low-vision users with text enlargement or text-to-speech options. The VA has received over 1,000 Section 508 complaints about Oracle Cerner, of which 469 have been accepted by the company to fix. A VA anesthesiologist complains of small icons and the need for multiple high-resolution monitors to display a patient’s entire record, while a team at one VA facility found that it doesn’t support text-to-speech. Unrelated to Oracle Cerner, a survey by the American Federal for the Blind found that more than half of respondents have struggled with using proprietary telehealth systems, especially hard-to-read chat sidebars, and some resorted to using FaceTime. (10/19/22)
The VA pushes back its next Oracle Cerner go-live from January 2023 to June 2023. VA Deputy Secretary Donald Remy says that the “assess and address” period is necessary because “the Oracle Cerner electronic health record system is not delivering for veterans or VA healthcare providers.” VA Secretary Denis McDonough announced in July that further deployments would be delayed until January 2023 while technical and system problems were resolved. The VA was set to roll the system out to 25 VA medical centers in 2023. The VA is sending letters to every veteran who may have been impacted by system problems at its five live sites, asking them to call the VA if they experienced delays in prescription filling, appointments, referrals, or test results. (10/17/22)
Two NHS trusts move to downtime paper recordkeeping after an apparent database error in Oracle Cerner required most of a day to resolve. During the downtime, Royal Free London, which was ironically in the middle of a “go paperless” campaign, nearly ran out of paper. (10/14/22)
Ascom works with Oracle Cerner to give nurses access to a patient’s EHR on Ascom’s Myco 3 VoWiFi smartphone. (10/12/22)
In England, County Durham & Darlington NHS Foundation Trust goes live on Cerner. (10/12/22)
Oracle Cerner engineers resolve an application package coding issue that caused the VA’s EHR pharmacy module to go down for 11 hours last week. In a separate incident, certain patients were unable to access the Defense Enrollment Eligibility Reporting System, a database of US military members, family members, veterans, and others eligible for military benefits. That issue resolved without technical intervention. (10/10/22)
Littleton Regional Healthcare (NH) goes live on Oracle Cerner’s Community Works EHR. (10/7/22)
Memorial Hermann Health System (TX) will switch from Oracle Cerner to Epic beginning early next year. (10/3/22)
Madigan Army Medical Center (WA) hosts a decommissioning ceremony for its Composite Health Care System. Science Applications International, now Leidos, was contracted to develop, design, and implement the system for the DoD in 1988. It rolled out across all military treatment facilities between 1992 and 1996, eventually running at 104 host sites with more than 100 interfaces with internal and external systems across the DoD and VA. It went live at Madigan in 1996, and experienced downtime only once, according to Col. (Dr.) David Owshalimpur, chief of nephrology at Madigan: “I always had it open during clinic days. If you knew the correct ‘cheat codes,’ you could fly through CHCS. It was also a much faster way to order labs, medications, and rads [radiological imaging] than AHLTA. So, CHCS was a nice backbone for both Essentris and AHTLA.” The medical center went live on MHS Genesis in 2017. (10/3/22)
September 2022
Keltie Jamieson (Horizon Health Network) joins the Bermuda Hospitals Board as CIO ahead of its Cerner go-live next month. (9/30/22)
VA Secretary Denis McDonough says it’s too soon to tell if an August EHR update by Oracle Cerner has finally fixed an “unknown queue” problem that caused thousands of clinical orders to disappear in an unmonitored inbox, causing patients to miss follow-up appointments. “We continue to have concerns about queues, unknown queues, unknown kind of areas where … veterans may end up,” he said. “I think that concern is significant enough that we’re not talking about a single, discrete issue that would suggest … a single discrete fix. But rather, they’re a pretty fundamental set of improvements. We’re continuing to make assessments about how big the challenge is.” (9/30/22)
VA Deputy Secretary Donald Remy tells Congress that its Oracle Cerner system is “not even close” to meeting patient needs and that “major improvements” are needed to resolve patient safety issues, which may force planned go-lives to be pushed back. The VA’s top contracting officer added in the Senate appropriations subcommittee hearing that the VA “shouldn’t blindly follow” DoD even though that’s why VA originally chose Cerner in a $10 billion no-bid contract. He added that the VA may renegotiate its Oracle Cerner deal when the base contract expires in May. Sen. Jon Tester (D-MT), chairman of the Senate Committee on VA Affairs, said that the implementation has been a “train wreck.” The VA’s Cerner project will cost $58 billion over 28 years, according to the testimony of Brian Rieksts, PhD of the Institute for Defense Analysis, which the VA asked to perform an independent life cycle cost estimate. Oracle EVP Mike Sicilia told the subcommittee that Oracle Cerner will “deliver a system that will leapfrog commercial EHRs” at no extra cost to the VA. “We intend to rewrite the Millennium EHR as a stateless cloud application which will deliver a modern user interface, ease of use, mobility, voice recognition, and self service. It will have machine learning-based clinical decision support and analytics that are built in from the ground up. We intend to deliver a beta of this new system in 2023 and we commit to deliver it across VA as a cost-free upgrade under the current contract.” Sicilia says that new modules will run in parallel with existing Millennium software, allowing VA to decide when to switch to the new ones without requiring data conversion. Asked by Sen. Tester where the VA’s project fits within Oracle’s priorities, Sicilia said, “This is the most important effort we have going on in the company. We have recast over 2,000 people, existing Oracle employees, to now work specifically on the VA EHRM program, in addition to the existing Cerner team.” He says the original 10-year timeline is still achievable. Oracle has contracted with Accenture for training, which Sicilia admits was managed better with the DoD’s project. Meanwhile, several members of the House Veterans’ Affairs Committee want to increase congressional oversight of the VA’s technology acquisitions, citing as examples its supply chain management system (adopted from DoD at a $2 billion cost, with OIG saying it meets less than half of VA’s needs) and Oracle Cerner, which Chairman Mark Takano (D-CA) calls “the poster child for major acquisition issues at the VA.” (9/23/22)
Anonymous US Army recruiters complain that the DoD’s Cerner system, which was supposed to speed up the time required to get new recruits processed and in uniform, has instead lengthened the timelines to the point that parents are complaining and recruits are changing their minds about enlisting. The recruiters say new policies and capabilities force them to wait to receive medical records relating to Cerner-flagged histories from providers, which can take weeks. Army officials say that the problem isn’t Cerner, it’s that recruits are often taking antidepressants and ADHD drugs and thus require a heath review that may get them disqualified for service. Anonymous online commenters complain that it was easier in the good old days because recruits could simply lie or plead ignorance about their medical histories. (9/21/22)
Oracle promotes Greg Aaron to group VP/GM of investor owned and emerging markets of Oracle Cerner. (9/19/22)
A paper in Spokane, WA profiles the healthcare plight of veteran Charlie Bourg, who discovered that his delayed cancer diagnosis was caused by a system defect within the Mann-Grandstaff VA Medical Center’s Cerner EHR that put his primary care doctor’s follow-up appointment and urology referral in a scheduling queue limbo for months. An Oracle Cerner rep says the EHR isn’t responsible for Bourg’s now-terminal condition: “Our findings show that nothing related to the EHR’s functionality or performance had anything to do with the care this veteran received and was unrelated to their diagnosis or treatment. The Oracle Cerner EHR is successfully in use at many thousands of health care facilities across the United States without incident. We remain a committed partner to VA to ensure its EHR system, and everyone who uses it, is able to provide the best possible care that our veterans deserve.” (9/14/22)
The 81st Medical Group at Keesler Air Force Base (MS) and the 96th Medical Group at Eglin Air Force Base (FL) will go live on MHS Genesis September 24. (9/14/22)
Oracle reports Q1 results: revenue up 18%, EPS $0.58 versus $0.89, meeting Wall Street expectations for revenue but falling short on earnings. Notes from the earnings call:
- Unfavorable foreign currency exchange rates cost the company $0.08 in adjusted EPS.
- Cerner contributed $1.4 billion of Oracle’s quarterly revenue, 12% of its total.
- Cloud revenue increased significantly, representing 30% of total revenue.
- CEO Safra Catz says that Oracle’s quarterly margin of 39% will increase “as we drive Cerner and its profitability to Oracle standards and continue to benefit from economies of scale in the cloud.”
- The company says it has migrated Cerner’s back office systems to its Oracle Fusion ERP system.
- CTO Larry Ellison says Oracle Cerner’s first newly developed application will be released within 12 months, developed with Oracle’s new Apex low-code tool and running on Oracle Cloud Database. He says Apex has security and fault tolerance built in, with the stateless application immediately failing over to another data center when problems arise.
Oracle offers a free OCI Cloud Tier that includes Apex Application Development and SQL Developer. It also offers a 10-minute tutorial on using Apex to transform a spreadsheet into a secure, scalable, multi-user web application. (9/14/22)
The Oracle Cerner Health Conference will return as an in-person event October 17-19, also offering a virtual track to those who prefer to attend remotely. (9/12/22)
Regional Medical Center (SC) is working with its auditors to adjust its financial reporting model following its year-ago conversion to Cerner CommunityWorks, which it says “is still not functioning as originally expected” as gross accounts receivable increased by 70% and bill submission slowed. (9/7/22)
The Ottawa Hospital in Canada recovers from an unspecified hardware issue that took its Epic, Cerner, PACs, Rhapsody, and Spok systems offline over the weekend. (9/7/22)
Moncrief Army Health Clinic at Fort Jackson (SC) will go live on MHS Genesis later this month. (9/7/22)
Biotech company Freenome launches a study of cancer risk factors using Oracle Cerner’s Learning Health Network and study enrollment technology from Elligo Health Research, in which Oracle Cerner is an investor. (9/7/22)
August 2022
Lyster Army Health Clinic at Fort Rucker Army Base (AL) and the 78th Medical Group at Robins Air Force Base (GA) will go live on MHS Genesis next month. (8/31/22)
VA data obtained by FedScoop under the Freedom of Information Act shows that the VA has had a least 45 days of Oracle Cerner downtime and 498 major incidents since its first rollout in September 2020. The VA itself was responsible for one-third of the incidents. The system issues caused 930 hours of incomplete functionality, 103 hours of degraded performance, and 40 hours of compete downtime. The VA lists five medical centers as being live on the Oracle Cerner system — Spokane, WA; Walla Walla, WA; Columbus, OH; Roseburg, OR; and White City, OR. It has paused deployments that were scheduled for 2022 until next year. VA Secretary Denis McDonough said in response to the FedScoop report, “The bottom line is that my confidence in the EHR is badly shaken … the system is not meeting those goals and needs major improvement. We at VA could not be more frustrated on behalf of Veterans and providers, and we’re holding Cerner, Oracle, and ourselves accountable to get this right.” (8/22/22)
The 6th Medical Group at Macdill Air Force Base (FL) and Fox Army Health Center (AL) will go live in the next wave of MHS Genesis deployments on September 24. (8/17/22)
Oracle Cerner executed 161 new, extended, or expanded contracts from April to June 2022, including 11 new clients. (8/15/22)
Cerner will pay $1.9 million in back pay and interest to 1,870 job applicants after the Department of Labor compliance evaluation found that the company had discriminated against Asian and black job seekers. The affected applicants were seeking employment as medical billing specialists, system engineers, software interns, and technical solution analysts at the company’s Kansas City, MO and Kansas City, KS offices. The review found that Cerner violated an executive order that prohibits federal contractors from discriminating in employment based on race, color, religion, sex, sexual orientation, gender identity, and national origin. (8/12/22)
Atrium Health (NC) wraps up its system-wide conversion from Cerner to Epic. (8/10/22)
The VA’s Cerner system goes down for several hours due to database corruption. The outage reportedly also affected DoD and Coast Guard sites. (8/8/22)
The VA names David Massaro, MD, MBA, MS as the functional champion of its Oracle Cerner implementation, on detail from the VHA’s Office of Health Informatics. (8/5/22)
Davis Health System (WV) and WVU Health will end their partnership due to a planned change in EHR vendors. DHS announced in February 2022 that it will implement Cerner under the CommunityWorks model, saying that while Epic and Cerner have similar functionality, Epic is unaffordable even when provided through WVU. DHS says WVU notified it immediately after it announced its EHR decision that it was ending the clinical affiliation due to lack of an integrated system. A DHS VP says, “It was a substantial difference of millions of dollars … we made the decision to go with Cerner, which will still speak to doctors at WVU or anywhere else in the state, it may just take an extra click … We went back to them and told them we would consider canceling our contract with Cerner if they could give us a new price that was more acceptable to our administration and the board. They said no.” (8/5/22)
The 42nd Medical Group (AL) at Maxwell Air Force Base and 1st Special Operations Medical Group (FL) at Hurlburt Field will transition to Oracle Cerner-based MHS Genesis next month. (8/3/22)
Oracle lays off staff in its marketing and customer experience divisions. Some Oracle Cerner employees also appear to be affected, according to this Reddit thread sent over by a reader, which includes rumors of the departure of several former high-level Cerner executives. Oracle is pursing $1 billion in annual compensation savings, which probably means the loss of 5,000 to 10,000 jobs of its 140,000. (8/3/22)
July 2022
Rep. Mike Bost (R-IL) warns that the House Veterans’ Affairs Committee may consider “pulling the plug” on the VA’s Oracle Cerner implementation if its larger sites don’t go live successfully early next year as the VA has promised. Bost also told a committee that the VA’s Cerner project is “a bad investment at any price” and that the project’s cost could be as high as $63 billion over 25 years “if everything goes wrong, and I see a lot of things going wrong.” (7/29/22)
Sources report that the Roseburg VA Health Care System’s Cerner-based EHR went partially offline for several hours last week due to a system overload that affected patient registration. (7/27/22)
Oracle EVP Mike Sicilia tells the US Senate Committee on Veterans’ Affairs that Oracle will move the VA’s Cerner implementation to the cloud and rewrite Cerner’s pharmacy module, completing both tasks within 6-9 months. Notes:
- Sicilia told the committee to consider that Oracle’s acquisition of Cerner gives VA, DoD, and the Coast Guard “a new, vastly more resourced technology partner overnight to augment Cerner.”
- Oracle says it will shift its top talent to working on the federal government’s Cerner challenges and is running the project from a war room that is staffed by senior Oracle engineers and developers.
- Sicilia says that Cerner, like its EHR competitors, is running on dated architecture using technology that is up to two decades old, making it hard to manage, support, and scale. Oracle says it will quickly move the Cerner application to a “modern, hyperscale cloud data center,” the same infrastructure that Oracle uses for critical industries in financial services and utilities. That conversion will be performed at no cost to the federal government.
- Oracle quickly fixed a database bug that caused 13 of the most recent 15 outages once the acquisition was completed and Oracle gained access to Cerner’s source code.
- The “unknown queue” was designed to account for human error rather than to mitigate it, so it will be redesigned.
- Sicilia says Oracle will “start over” with the Cerner pharmacy module, rebuilding it as a showcase of a cloud-optimized web application. (7/25/22)
The VA postpones this week’s planned Oracle Cerner go-live in Boise, ID due to system stability issues that the VA says make it unsuitable for larger-facility use. The VA has no other go-lives scheduled for 2022. The Spokane paper obtained a document from Mann-Grandstaff VA Medical Center that lists 180 incidents of system degradation and downtime since September 2021, a far larger number than the VA has acknowledged. Meanwhile, VA officials tell Congress that its implementation will cost $51 billion over the next 30 years, including maintenance and staffing, but it does not expect the $16 billion Cerner contract to run over budget unless the 10-year implementation timeline is extended. (7/22/22)
An internal email that was shared on Reddit – and confirmed by Oracle as authentic by the Kansas City business paper — outlines significant changes in the former Cerner business that is now owned by Oracle:
- The business is now called Oracle Health, one of Oracle’s Global Industry Units (GIUs), with no mention of whether the Cerner name will continue to be used.
- Former Cerner President and CEO David Feinberg, MD, MBA will become chairman of Oracle Health, with unstated responsibilities and reporting structure.
- Former Chief Client and Services Officer Travis Dalton, MPA, who led Cerner Government Services, will run Oracle Health as its general manager.
- Former CTO Jerome Labat and other Cerner technology executives will report to Oracle EVP Don Johnson, the company’s cloud executive who will now oversee Oracle Health engineering.
- Corporate functions such as IT, finance, legal, and HR will be moved to Oracle teams. (7/20/22)
Former Cerner CEO David Feinberg, MD will become chairman of the new Oracle Health Global Industry Unit, while former Cerner Chief Client and Services Officer Travis Dalton will become general manager. (7/19/22)
A VA OIG report concludes that the VA’s use of an “unknown queue” in its Cerner system caused multiple events of patient harm in which orders failed to reach their intended care location. Notes from the report:
- The system failed to deliver 11,000 orders in which clinicians chose a service location that didn’t match the type of service that they were ordering.
- The system did not notify the clinicians that their order had not been delivered, and in fact assured them that their order had been accepted.
- The VA learned of the unknown queue’s existence when it opened its first Cerner trouble ticket about the problem four days after go-live, after which the VA instructed staff to monitor the queue and cancel and re-enter the problem orders.
- Cerner says that a a VA leader had approved the use of the unknown queue in January 2020, but that leader and their supervisor say they weren’t aware of it.
- Cerner created a provider alert for their undelivered orders in February 2022, but the VA said that the solution wasn’t adequate.
- The OIG did not accept the response to its report from VA Deputy Secretary Donald Remy because it failed to address the report’s key finding that patients were harmed.
- Remy says that Cerner and the VA were both aware of the queue’s existence before go-live, but OIG says it was provided with no evidence to support that statement and that users weren’t informed about the queue until a year after go-live.
- OIG says it it is “troubling” that Remy absolves Cerner for failing to educate VA about the unknown queue and instead blames VA users for the negative outcomes it caused.
- OIG also notes that both the Deputy Secretary and EHRM IO executive director were aware of the patient harm that resulted, but in their testimony to Congress, they insisted that no harm had occurred.
A second new VA OIG report looks at the VA’s Cerner training:
- VA project executives sent misleading information to OIG in to a “careless disregard for the accuracy and completeness of the information.”
- VA showed OIG a training evaluation plan without disclosing that the plan had not been reviewed, approved, or implemented.
- OIG was given a slide that showed the user proficiency pass rate at 89% instead of the actual 44%, then explained the error as being due to removing a small number of outliers who had taken and failed the test up to 29 times. VA had not calculated the numbers until it received OIG’s request. (7/18/22)
A new report from the VA’s Office of Inspector General confirms that an “unknown queue” within the VA’s Oracle Cerner system led to 150 adverse patient events. (7/15/22)
An Oracle EVP says in a letter to two members of of VA’s Subcommittee on Technology Modernization that the VA’s Cerner system was “not operating as intended” at Mann-Grandstaff Medical Center, in which an “unknown queue” problem caused patient orders to be delayed or lost. The company says Oracle’s expertise and technology will be used to “rethink approaches not possible before the acquisition.” Cerner and the VA had agreed on how the queue would be used to detect incorrectly entered orders going back to January 2020, but the VA didn’t train its clinicians to monitor it. The letter was signed by Oracle EVP and company lobbyist Ken Glueck. This is good reporting from Orion Donovan-Smith of the Spokane Spokesman-Review. Meanwhile, Oracle is reportedly considering cost reductions of up to $1 billion that would result in the layoff of thousands of employees as early as next month. Its recent $28 billion acquisition of Cerner added 28,000 employees to Oracle’s headcount of 143,000. (7/11/22)
Astria Health and Cerner settle their legal dispute in which the health system blamed its 2019 bankruptcy on problems with Cerner’s billing system. Cerner disputed that claim, saying that Astria poorly managed its merger with two other hospitals. (7/11/22)
A new KLAS report on EHRs for practices of 11 or more clinicians finds that Epic and Meditech lead the the pack in finishing a close 1-2. Ease of use and workflow is by far the most pressing concern of practices of that size. Cerner users are frustrated with outpatient workflows and the company’s focus on resolving inpatient problems, while Greenway Health’s customers are an outlier in putting functionality improvements at the top of their list of needs. Allscripts has two of the three bottom-rated products, along with poor ratings for support, relationships, and overselling product capabilities. (7/6/22)
June 2022
KLAS says that Oracle Cerner’s go-forward RCM product RevElate won’t necessarily solve the company’s high-profile revenue cycle problems, as customer experience with implementation and training of its underlying Soarian Financials product has been mixed. Customers say that Soarian Financials is a solid system that drives good outcomes despite usability issues, but requires more add-on products than expected, has exposed customers to more nickel-and-diming since Cerner acquired the product in 2015, and won’t solve Oracle Cerner’s challenges of hiring and keeping employees who can facilitate successful outcomes. (6/24/22)
The 49th Medical Group at Holloman Air Force Base in New Mexico celebrates the launch of MHS Genesis. (6/22/22)
In Australia, the Queensland government will allocate an additional $200 million USD for the continued implementation of its enterprise Cerner EHR project over the next five years. Sixteen of a hoped-for 27 hospitals have gone live to some degree on the new system. Originally launched in 2011 with a budget of $288 million, the IEMR project ballooned to an estimated completion cost of $840 million. An audit in 2018 found the scheme to be 40% over budget. Further problems, including outages in 2019, physician complaints, and the departure of the director-general have hampered go-live timelines. (6/22/22)
VA OIG finds that at least 148 veterans in Inland Northwest were harmed by a Cerner software flaw that the company was aware of, but failed to disclose to the VA. The VA OIG’s draft report concludes that the Cerner system failed to deliver 11,000 orders for specialty care and lab work due to unrecognized locations that sent the mismatched orders to the “unknown queue.” Each order had to be reviewed and re-entered by VA employees. A statement from Oracle said the company will bring additional resources to the VA’s Cerner program. VA OIG contacted four Cerner employees for further information. Two of them, including a Cerner VP, did not respond to repeated requests, while the other two offered no reason that the VA wasn’t notified of the problem. Meanwhile, the VA will delay further Cerner rollouts until 2023 to ensure “adequate reliability.” Puget Sound VA’s go-live that was scheduled for August will now take place in March 2023, while VA Portland will move its implementation from November to April 2023. (6/20/22)
Eisenhower Army Medical Center at Fort Gordon (GA) works through patient portal appointment scheduling issues in its new MHS Genesis system, which went live over the weekend. The go-live marked the half-way point for the DoD’s facility-wide rollout of the Cerner-based system. The department anticipates wrapping up the enterprise deployment by the end of 2023. (6/15/22)
Oracle says in its earnings call that it will review Cerner’s product portfolio to find opportunities to move from third-party technologies to those of Oracle, including moving to Oracle’s cloud infrastructure. Larry Ellison added that Oracle’s plan for a national health records database is “clearly going to be our largest business.” (6/15/22)
Oracle Executive Chairman and CTO Larry Ellison says in a Cerner acquisition update that hospital EHRs – he names Cerner, Epic, and Allscripts – fragment records across providers because each hospital buys and operates its own, preventing providers from accessing a patient’s records in an emergency and limiting the value to public health researchers. Ellison says Oracle will create a national EHR database that is continuously updated via updates from provider EHRs. Providers will be able to access identifiable information if authorized by the patient, while public health researchers would be limited to a de-identified view. Ellison says Millennium will be significantly enhanced with voice UI, AI models, and automated clinical management. He mentioned the oncology decision support work of Project Ronin, of which Ellison is a co-founder. Much of the presentation touted Oracle’s other healthcare offerings, such as ERP, workforce management, clinical trials, and cloud services. Cerner will operate under the name Oracle Cerner, according to several references in the presentation. (6/13/22)
Plans to implement a Cerner-based EHR across facilities on Prince Edward Island in British Columbia have come to a halt due to usability issues. The province had hoped to have all sites live by 2020. Forty-three clinics and 118 physicians have been connected to the system, with 100 more clinicians still to go. The same software has been in use at Island Health hospitals for over a decade. Two independent reviews of that $178 million implementation have been conducted based on physician complaints of poor usability and patient safety risks. (6/8/22)
After more than a year of training, Martin Army Community Hospital at Fort Benning in Georgia will go live on MHS Genesis this weekend. (6/8/22)
Medical Center Health System (TX) rolls out a patient portal app incorporating EHR technology from Cerner and video visit capabilities from Amwell. (6/8/22)
Oracle shares see a slight uptick on the news that the company has closed its deal to acquire Cerner for $28 billion. (6/8/22)
A VA OIG report says that the year-ago implementation of Cerner at Mann-Grandstaff VA Medical Center (WA) has caused gaps in performance, quality, and access metrics, with employees questioning whether the hospital can pass an upcoming Joint Commission accreditation survey. Employees are performing laborious workarounds and making best guesses since the hospital is reporting only 13 of the VA’s 103 organizational performance metrics. OIG listed challenges such as Cerner’s failure to deliver metrics reports, lack of VA resources and training, and the VA’s failure to assess EHR metrics before go-live. (6/3/22)
Oracle clears regulatory review of its acquisition of Cerner, with completion of the tender offer expected on Monday, June 6. Oracle’s update emphasizes “our new, easy-to-use systems” whose primary user interface will be hands-free voice technology and the “huge growth engine” that will result from Oracle expanding Cerner’s user base to additional countries. Oracle Chairman and CTO Larry Ellison and other Oracle executives will discuss the acquisition in a June 9 webinar titled “The Future of Healthcare.” (6/3/22)
Oracle’s acquisition of Cerner is reported to be on track to close within the next couple of weeks. (6/1/22)
May 2022
The lab manager of the VA’s Walla Walla, WA medical center says its newly implemented Cerner system saves employees three hours per day by digitally tracking specimens. He says his goal was to ignore the negative narrative about Cerner and instead spend time preparing for the implementation. (5/27/22)
ChristianaCare will use a $1.5 million grant from the American Nurses Foundation to deploy five Diligent Robotics Moxi robots, integrated with Cerner to relieve nurses of delivery tasks and to use AI to predict when they will need equipment, supplies, and medications. (5/25/22)
The Roseburg VA Health Care System (OR) will launch its new Cerner EHR on June 11. (5/25/22)
The EU reportedly gives Oracle unconditional antitrust clearance for its proposed $28 billion acquisition of Cerner. (5/25/22)
Cerner will pay an unreported sum to Sweden’s Västra Götaland to settle complaints over Millennium implementation delays that Cerner attributes to the pandemic and to the region itself. Cerner says it is ready to proceed with the project, has 250 employees working in Sweden, and plans to bring up parts of the system this fall. The region was reportedly seeking payment of $50 million to offset its increased costs. (5/20/22)
Cerner, Elligo Health Research (in which Cerner is an investor), and Freenome will participate in an early cancer detection clinical trial using Cerner’s Learning Health Network, which sells de-identified patient data from participating health systems. (5/20/22)
DoD facilities including Naval Branch Health Clinic and the 3rd Combat Aviation Brigade, Hunter Army Airfield, both in Georgia, will transition to MHS Genesis next month. (5/18/22)
A VA Office of Inspector General report determines that lack of prompt EHR documentation and care coordination between a VA provider and private chiropractic clinic contributed to the spinal and rib fractures of an 87 year-old patient. The nearly century-old Ohio facility is one of 35 that the VA is considering closing within the next several years. (5/18/22)
DoD facilities including Naval Branch Health Clinic and the 3rd Combat Aviation Brigade, Hunter Army Airfield, both in Georgia, will transition to MHS Genesis, a Cerner project, next month. (5/18/22)
Cerner will issue the VA an unspecified credit for failing to meet the minimum system uptime requirements specified in the $10 billion contract. (5/13/22)
A survey of 701 DoD providers finds that 58% have identified inaccurate or incomplete data in the agency’s Cerner-powered MHS Genesis system, leading to inaccurate, delayed, or incomplete diagnoses; multiple patient visits to complete care; and longer patient visit times. Medical device integration with MHS Genesis was also found to be problematic, with respondents noting that “…eye care devices are not connected to the system and this creates significant delays and repeat imaging,” and “the process to get medical devices connected is CONTRARY to 21st century healthcare delivery. We just choose to ignore that equipment isn’t connected.” (5/11/22)
An OIG joint audit of efforts by the DoD and the VA to make their Cerner systems interoperable notes that migration of legacy data into Cerner could have been more consistent, that medical device integration could be improved, and that user access should be limited to information needed to perform job duties. (5/9/22)
The VA confirms that Cerner was unavailable 50 times for at least some users singe going live in its Pacific Northwest sites, but the outages were not widespread. The VA’s Oregon and Idaho sites will go live next in June. (5/9/22)
Cerner reports Q1 results: revenue up 4%, adjusted EPS $0.93 versus $0.78, meeting earnings expectations but falling short on revenue. (5/4/22)
Winn Army Community Hospital at Fort Stewart in Georgia will go live on Cerner next month as part of the DoD’s continued wave of MHS Genesis roll-outs. (5/4/22)
VA Secretary Denis McDonough says the agency will continue rolling out its new Cerner software despite five recent outages that have caused some lawmakers to call for a halt to implementations. The VA’s Central Ohio Healthcare System in Columbus went live on the EHR over the weekend. McDonough said he is “very concerned about the execution of the program to date” and added that the first of the downtimes was so “egregious” that Cerner CEO David Feinberg, MD, MDA issued a signed apology. (5/4/22)
April 2022
KLAS summarizes US hospital EHR market share activity for 2021 (click the graphic to enlarge):
- Epic gained four new customers representing 28 hospitals and 13,000 beds last year, losing four due to M&A.
- Meditech Expanse was chosen by 74% of the company’s legacy customers that made a replacement decision in 2021, compared to 38% retention in 2020.
- Epic has 33% of hospitals and 44% of beds versus Cerner’s 24% and 27%, respectively.
- Allscripts and CPSI lost ground in 2021.
- Cerner had the largest net decrease in bed count last year, with half of those hospitals choosing Epic as a replacement and the other half switching to Epic after being acquired.
- Cerner hasn’t had a net-new large health system sale since 2013. (4/27/22)
Spokane VA officials confirm that a veteran was hospitalized with heart failure in March after his heart medication prescription – which was ordered a year previously, before Mann-Grandstaff VA Medical Center’s conversion to Cerner – disappeared off his Cerner active medication list and was not renewed. The incident has been classified as a sentinel event that had the potential to cause significant patient harm, although in this case the veteran was discharged, apparently well, after a five-day inpatient stay. The VA expires all prescriptions after one year and suspects that the heart drug was already discontinued before Cerner was went live, adding that it remained visible on Cerner’s “historical medications” screen. Five Mann-Grandstaff clinicians say they have seen the problem of prescriptions expiring and disappearing from the meds list, but weren’t adequately trained on the process. The VA’s VistA system that Cerner replaced also expired prescriptions after one year, but left them on the active medication list to prompt providers to renew them when appropriate instead of dumping them onto a historical list of inactive meds that could go back years. (4/25/22)
Adventist Health Mendocino Coast Chief of Staff William Miller, MD outlines lessons learned from its implementation of Cerner in its clinics in a local newspaper opinion piece:
- Timelines were extended due to COVID-caused staff resignations and shortages.
- System bugs prevented the prescription refill function from communicating with local pharmacies and impeded referrals to specialists.
- The problems increased phone call abandonment and hold time.
- Moving data to Cerner required more time than expected, extending appointment scheduling time from weeks to two months.
- The hospital didn’t do a good job of communicating the transition to patients and the community. (4/22/22)
Puget Sound Military Health System, Madigan Army Medical Center, Naval Health Clinic Oak Harbor, the Air Force’s 62nd Medical Squadron, and Naval Hospital Bremerton upgrade their Cerner-powered MHS Genesis EHR software with Revenue Cycle Expansion features. The Washington-based providers were among the initial wave of facilities that went live on MHS Genesis in 2017. (4/20/22)
Oracle extends its Cerner acquisition deadline from April 13 to May 11, with no other changes of terms to the $28 billion deal. Oracle says that 11.5% of CERN shares have been tendered as of Friday. (4/13/22)
Allscripts and Cerner achieve top customer rankings for their integrated EHR and RCM technologies, according to Black Book’s latest survey of 1,700 community hospital end users. (4/13/22)
All federal Cerner systems – DoD, VA, and Coast Guard – went down for two hours Wednesday due to a server problem. The irony is that the server in question was running database software from Oracle, soon to be Cerner’s owner in giving CIOs their “one throat to choke.” VA Deputy Secretary Donald Remy says that the VA and Cerner will conduct a root cause analysis of the downtime. Meanwhile, the VA’s Walla Walla facilities went live as planned on March 26. Columbus is up next on April 30. (4/11/22)
Cerner hires former US Army Major General Patrick Sargent, MS (OptumServe) as SVP/GM of Cerner Government Services and promotes Alaa Adel, MBA to SVP/President of Cerner Global. (4/8/22)
A new KLAS report on the EHR market in Europe finds that Dedalus and CompuGroup Medical expanded their market share via acquisitions, with Cerner selling its Selene and Medico products to CGM in shifting its focus to Millennium and I.S.H. Med. Software Medical and Epic had the largest organic growth, while Epic’s performance score topped the list. Low-scoring vendors are ChipSoft and Cambio (Benelux and Northern Europe) and InterSystems and Dedalus (Western Europe), although InterSystems TrakCare has high user satisfaction in Southern Europe, particularly Italy. (4/6/22)
Cerner won’t require non-client facing employees to be vaccinated until June 6, when workers are expected to return to in-office work. (4/4/22)
March 2022
The VA launches its second site on Cerner as Walla Walla Health Care goes live. (3/28/22)
Bayne-Jones Army Community Hospital at Fort Polk (LA) goes live on Cerner as part of the DoD’s Wave Hood MHS Genesis deployment. Col. Aristotle Vaseliades, hospital commander, said the information management department did an amazing job, rolling out nearly 3,000 pieces of equipment, conducting 176 training sessions, and running countless miles of computer cable. He didn’t mention which department handled embroidering MHS Genesis baby onesies. (3/25/22)
VA Deputy Secretary Donald Remy says the agency is ready to launch a new Cerner system at the VA medical center in Walla Walla, WA this weekend. Several lawmakers have called for a halt to future deployments after the VA OIG issued several reports citing patient safety issues at the initial go-live site in Spokane, WA. (3/25/22)
The VA and Cerner promise to perform a thorough root-cause analysis of the software bug that caused Mann-Grandstaff VA Medical Center and associated clinics in Washington and Idaho to take their Cerner EHR offline and revert to paper records earlier this month. The troubled roll-out of the new system at Mann-Grandstaff, the VA’s initial go-live site in its projected $16 billion facility-wide Cerner implementation, has prompted several lawmakers to call for the postponement of future implementations. (3/23/22)
Carl R. Darnall Army Medical Center (TX) at Fort Hood, the 71st Medical Group at Vance Air Force Base (OK), and Womack Army Medical Center (NC) at Fort Bragg have gone live on Cerner as part of the DoD’s MHS Genesis EHR overhaul. The new system will be deployed in several more waves this year to 54 facilities, the DoD’s largest group in any calendar year. (3/23/22)
Naval Medical Center Camp Lejeune is among several DoD locations in North Carolina that are going live on Cerner this week. (3/21/22)
Cerner will integrate Nuance’s DAX ambient clinical documentation with Millennium. It’s interesting that a company that is about to be acquired by Oracle – which made integration of Millennium with its own hands-free voice interface as the acquisition driver — would tout integration with Microsoft-owned Nuance and its Azure-hosted voice solution. Somehow I doubt that this latest announcement will come to fruition unless the acquisition deal falls apart since I don’t see Oracle playing all that nice with Microsoft, Google, or anyone else. (3/21/22
Senator Patty Murray (D-WA) demands that the VA delay its planned March 26 Cerner go-live at the Walla Walla VA following VA OIG reports of continuing problems at the first live site at Mann-Grandstaff VA Medical Center in Spokane. VA OIG issued a report Thursday in which it substantiated several user complaints related to medication management at Mann-Grandstaff, along with deficiencies in migrating DoD patient information to Cerner. OIG substantiated reports that Cerner was not configured to accept future clinic orders for subsequent outpatient visits, so it cancelled them without notifying the provider. They also noted that if RNs entered multiple medication orders, only the first one was held pending physician authorization. (3/21/22)
Fisher-Titus Medical Center in Ohio has integrated RevSpring’s PersonaPay and IVR Advantage payment data and communications technologies with its Cerner system. (3/18/22)
Reynold’s Army Health Clinic at Fort Sill in Oklahoma will go live on Cerner this weekend as part of the DoD’s MHS Genesis deployment. (3/18/22)
Cerner will integrate Nuance’s Dragon Ambient Experience voice-enabled automated documentation software with its Millennium EHR. (3/18/22)
The VA will use medical imaging workflow technology from Laurel Bridge Software during its transition from VistA to Cerner. (3/18/22)
From the Oracle earnings call on Friday, following Q3 results that beat revenue expectations but fell short on earnings:
- CTO and Chairman Larry Ellison says that healthcare is “the largest industry on Earth” and Oracle has as ERP/HCM customers Tenet, Kaiser, Mayo, Cleveland Clinic, Northwell, Mount Sinai, and Atrium.
- He notes that Oracle is replacing Kronos in 83-hospital Community Health Systems.
- He says that hospitals are an Uber-like gig economy because doctors and now nurses are increasingly independent contractors, making workforce payment complicated.
- Ellison says that the company will be “going after the entire integrated ecosystem,” which influenced its decision to acquire Cerner.
- He also called out connecting clinical trials with hospitals and tracking hospital supplies by RFID.
ORCL shares are down 15% versus the Dow’s 6% loss since the December 20 announcement that it will acquire Cerner for $28 billion. (3/14/22)
The VA says last week’s unplanned, two-day Cerner downtime at its only live site in Spokane – in which admissions were halted because patient screens were showing the information of different patients – was caused by a Cerner programming error . A review has found only a few corrupted records so far, some of those at its Columbus location where Cerner is not yet live. The VA admits that it probably shouldn’t have been making programming changes so close to the system’s next go-live in Walla Walla, WA on March 26. (3/11/22)
A new KLAS report on healthcare AI finds that previous market share leader Jvion has lost many customers who report financial constraints and lack of outcomes, ClosedLoop.ai scores highly in customer satisfaction, while Health Catalyst has seen satisfaction jump as it offers more analytics-powered prescriptive guidance. Customers of Cerner and Epic report struggles to get their published models up and running, and while Epic customers complain about nickel-and-diming since prebuilt models are priced individually, they are increasingly licensing its Cognitive Computer Developer Platform that allows them to deploy their own models. Respondents provided some tips:
- Start with analytics before jumping into predictive or prescriptive models.
- Identify the problem you are trying to solve, then decide whether AI is the right tool.
- Set clear goals for use cases.
- Don’t obsess with perfecting incoming data. The machine learning should be applied to data in its current form.
- Model testing takes longer than you expect.
- Focus on defining the intervention more than perfecting the model. (3/11/22)
Oracle shares were down 6% in early after-hours trading Thursday as the company announced Q3 results that beat revenue expectations but fells short on earnings. Some analysts noted before the announcement that the company’s pending acquisition of Cerner has caused investor consternation and urged the company to explain its healthcare vision. (3/11/22)
Mount Desert Island Hospital and Health Centers in Maine implements Cerner. (3/9/22)
Spokane’s VA hospital warned users on Thursday to stop using its recently implemented Cerner system and to “assume all electronic patient data is corrupted / inaccurate.” The problem forced Mann-Grandstaff VA Hospital to stop new admissions, suspend the filling of prescriptions, and to review whether surgeries could be performed safely. The VA says the system went back online Friday morning. Rep. Cathy McMorris Rodgers (R-WA) says she was told that the problem was a VA database update that was performed to communicate patient demographics with Cerner, which suggests that the Cerner system itself might not have been the problem. At least one veteran reported seeing another patient’s information when they logged in to the patient portal. The VA’s second go-live is set for March 26 and another round is scheduled for June. (3/7/22)
Shares in the Global X Telemedicine & Digital Health exchange-traded fund dropped 4.5% in the past 30 days versus the Nasdaq’s 4% decline. EDOC shares are down 11% since the fund’s July 2020 inception versus the Nasdaq’s 26% gain. Its 10 biggest holdings are Illumina, DexCom, Agilent Technologies, Tandem Diabetes Care, Labcorp, Cerner, UnitedHealth Group, Nuance, Omnicell, and Change Healthcare. (3/7/22
Mann-Grandstaff VA Medical Center (WA) has taken its Cerner EHR offline after a service outage due to an issue with patient demographic data forced it to revert to downtime procedures. (3/4/22)
The Epsom and St. Helier Hospitals Group will implement Cerner at their four facilities in southwest London. (3/2/22)
February 2022
Cerner announces Q4 results: revenue up 4%, adjusted EPS $0.93 versus $0.78. The company’s acquisition for $95 per share by Oracle remains on track for sometime in 2022. Shares closed Tuesday before the announcement at $91.83. (2/23/22)
The US Social Security Administration contracts with Cerner to electronically transfer disability claims information the EHRs of its customers. (2/18/22)
VA Acting Deputy CIO Laura Prietula tells attendees at an AFCEA Bethesda health IT event that the department has made significant improvements to its EHR data transfer processes, adding that it has standardized the majority of the high-priority datasets that are being transferred from VistA to Cerner’s Millennium and HealtheIntent platforms. (2/16/22)
Little Rock Air Force Base Clinic (AR) will transition to the DoD’s Cerner-powered MHS Genesis system next month. The department plans on rolling out MHS Genesis at 54 facilities this year, which would see the technology deployed at more than half of all military hospitals and clinics. (2/16/22)
Davis Health System (WV) will implement Cerner across its three hospitals beginning this summer. (2/16/22)
KLAS reports that some Cerner customers are forming contingency plans in reacting to company changes that include hiring a new CEO, a revenue cycle management pivot, executive turnover, and an announced acquisition by Oracle. Notes:
- Cerner’s overall KLAS performance scores haven’t changed over five years and under three CEOs, while confidence in the company’s ability to deliver has declined.
- Some customers attribute their success to their own efforts rather than those of Cerner.
- CEO David Feinberg will need to improve overall customer success, break the company’s history of broken promises and nickel-and-diming, and establish its new revenue cycle product.
- Many customers question Cerner’s choice of the old Soarian platform to develop RevElate, noting that the product is rated only in the 60s and sometimes takes customers years to use effectively. They also question how the lack of native integration will work in an industry that has mostly moved away from standalone applications.
- Company acquisitions tend to work out well about half the time, and when they don’t, customers are twice as likely to abandon the vendor. (2/11/22)
Training issues still plague the DoD’s Cerner-powered MHS Genesis system, according to an annual oversight report from the DoD’s Office of the Director, Operational Test, and Evaluation. Nearly 75% of the report’s survey respondents consider the program’s computer-based training to be “poor,” though a new initiative to give users hands-on practice in a mock environment did see improvement. The report ultimately concludes that the system “is not yet survivable in a cyber-contested environment.” (2/9/22)
Highlights from the just-announced Best in KLAS awards:
- Epic, Nordic, Galen Healthcare, and The Chartis Group were named as overall best.
- Epic won Best in KLAS awards in 11 market segments.
- Most-improved products include Infor ERP and Greenway Intergy Practice Management.
- Epic was the top-rated physician practice vendor by far, followed by Athenahealth, NextGen Healthcare, Greenway Health Intergy, Allscripts, and EClinicalWorks.
- Topping the overall software suite rankings was Epic, followed by Meditech Expanse, Cerner, CPSI Evident Thrive, and Allscripts.
- Nordic led overall IT services firms, followed by Pivot Point Consulting, Bluetree Network, Experis Health, Impact Advisors, Engage, and Cerner.
KLAS also announced the global software (non-US) winners. Some highlights:
- Nearly all respondents have adopted virtual visit technology.
- Digital pathology is growing rapidly in Europe.
- Top acute care EMR winners are InterSystems TrakCare EPR (Asia/Oceania), Epic (Canada and Europe), Philips (Latin America), and Cerner (Middle East/Africa). (2/9/22)
A GAO report finds that the VA did not establish performance measures and goals for migrating data from VistA to Cerner Millennium and HealteIntent before initial go-live in October 2020. The VA concurred with GAO’s recommendation that it establish and use data performance measures and use a stakeholder register make sure reporting needs are addressed. The VA notes that any VistA data can be extracted, packaged, and sent to Cerner automatically even in the absence of a database model, 80% of critical reports are now using Cerner-generated data, and its data migration team is monitoring VistA for changes and patches that may require regenerating extraction code to keep data flowing. (2/2/22)
January 2022
The VA chooses Palo Alto Networks to secure its Cerner implementation and other projects. (1/28/22)
The DoD goes live on its Cerner-based MHS Genesis system at 100 locations in Texas, including Brooke Army Medical Center and Wilford Hall Ambulatory Surgery Center. BAMC is the Defense Department’s only Level 1 trauma center. The system is 38% deployed across the Defense Department. The MHS Genesis rollout is scheduled for completion by the end of 2023. (1/28/22)
Cerner lists the Golden Parachute Compensation that will be paid to its top executives if they are forced out in the Oracle acquisition:
- President and CEO David Feinberg $22 million (company tenure – less than four months)
- EVP/CFO Marc Erceg $11 million (company tenure – less than one year)
- EVP/CTO Jerome Labat – $11 million (company tenure – 19 months)
- Former Chairman and CEO Brent Shafer — $21 million
- Four other Cerner executives will potentially benefit from the change-in-control terms of their contracts.
Cerner’s SEC filing also provides a timeline of Oracle’s acquisition offer:
- Rumors of unsolicited take-private acquisition offers arose in May and June 2021.
- Cerner turned down a private equity sponsor’s request for acquisition discussion in July, an offer that was repeated and again denied in August 2021.
- Oracle made its initial inquiry on October 7 and due diligence followed.
- Oracle made a $92 per share offer on November 12.
- Cerner’s board discussed opening up the sale process to private equity buyers on November 20, but worried about long timelines, the risk of information leaking out, price uncertainty, and losing Oracle as a buyer. They also expressed concern that the deal size would require the participation of a consortium of private equity buyers that would complicate the sale process. They ruled out contacting potential strategic buyers for the same reasons plus a concern about “the potential lack of interest.”
- Cerner told Oracle that its per-share offer was too low on November 24, Oracle said it needed Cerner’s board to be specific about the price it sought, and Cerner gave a price of “the upper $90’s” on November 29.
- Oracle offered $95 on December 1. A Cerner executive was rebuffed when trying to increase the offer price, with Oracle saying its price was its “best and final offer.”
- Cerner received an email inquiry from a potential strategic buyer on December 17, but was operating under an exclusivity agreement with Oracle through December 20.
- No other potential bidders expressed interest after the Wall Street Journal reported the proposed Oracle acquisition.
- The board listed the risks of continuing to run Cerner as a standalone company as (a) competition and healthcare market challenges; (b) operating and product risks in a rapidly changing technology environment; (c) increased competition; (d) retention of key technical employees; (e) risks in government contracting; (f) hitting growth targets in foreseeable market conditions with few attractive acquisition targets to boost growth and enter new markets; (g) the risk of not hitting growth and profit targets; and (h) uncertainties around COVID-19’s impact on the company’s business.
- Terms of the merger agreement allow Cerner to consider unsolicited better offers. (1/26/22)
Hunt Regional Healthcare (TX) will implement Cerner Millennium via its CommunityWorks delivery model. (1/21/22)
Cerner SEC filings indicate that President and CEO David Feinberg and CTO Jerome Labat have waived their right to voluntarily leave the company within 12 months of the close of Oracle’s acquisition of Cerner. If Oracle terminates them, they will get $4.5 million and $2.3 million in cash, respectively, plus accelerated share vesting. Feinberg was hired in August 2021 and Labat in June 2020. (1/21/22)
The VA pushes back its second Cerner go-live from March 5 to April 30 at its Columbus, OH facility, which it says has experienced training delays because 200 of its 1,700 employees are absent. (1/17/21)
Cerner co-founder Cliff Illig is interviewed by former Cerner President Donald Trigg in a new episode of the latter’s podcast that covers health IT entrepreneurship (it was recorded before the Oracle acquisition announcement, so perhaps a follow-up is indicated). All three Cerner founders grew up in families of kitchen-table businesspeople and saw in the early 1970s how computers were starting to be used by businesses, then started selling custom built problem-solving software in a half-dozen industries, with healthcare being on the list of industries they knew nothing about until a medical lab engaged them. Illig says Cerner sought venture capital because they needed credibility, not money, then were reasonably pushed by the VCs into going public as a liquidity event. He says that entrepreneurs shouldn’t be scared of complexity, which is common in healthcare, because you can figure it out by breaking it down into pieces. He says Neal Patterson was the most biased toward action of any of Cerner’s leaders and had an intolerance for things taking too long, spending too much time on analysis, and studying market surveys to decide what to do. The Cerner founders said that rather than studying every possible course of action, they just picked one by “shooting real bullets” and learned from the results. (1/7/21)
The Bermuda Hospitals Board will go live on Cerner Millennium across its two hospitals and urgent care center later this year. (1/5/22)
December 2021
The executive director of the World Privacy Forum is concerned that the acquisition of Cerner will give Oracle – which runs the world’s largest third-party data marketplace – access to Cerner-stored patient data. She says that business associate rules might allow Oracle to use Cerner’s EHR patient data to train AI systems. (12/22/21)
Several investment firms and bond raters downgraded Oracle’s shares and debt Tuesday following its announced intention to acquire Cerner. They worry that the cash payout is large and Cerner’s offerings aren’t strategic to those areas where Oracle should focus. Oracle has $23 billion in cash and will likely need financing to complete the Cerner acquisition for its offer of $28 billion in cash. ORCL shares dropped 5% on the announcement Monday and were flat Tuesday. Oracle’s biggest previous acquisition was PeopleSoft, which it acquired for $10 billion in 2004. (12/22/21)
Oracle will acquire Cerner for $28.3 billion in equity value in an all-cash deal, the companies announced this morning. (12/20/21)
Cerner shares closed at Friday $89.77, up 13% on the rumor that Oracle will acquire the company in a $30 billion deal. ORCL shares dropped 6% on the Wall Street Journal report. (12/20/21)
Two Republication US senators introduce a bipartisan bill that requires the VA secretary to report the cost, performance metrics, and outcomes of its Cerner project quarterly to Congress. (12/17/21)
A new KLAS report that covers EHR vendors that offer a wide range of comprehensive solutions for ambulatory practices finds that Epic, NextGen Healthcare, and Cerner earn high user satisfaction with offering technologies that meet most or all of an ambulatory practice’s needs, although the virtual care offerings of those vendors are sometimes passed over in favor of best-of-breed tools. Cerner customers remain concerned about Cerner’s revenue cycle track record and don’t always choose its practice management solution, while all interviewed customers of NextGen Healthcare and Epic report lowered costs and/or increased revenue after implementation. (12/17/21)
Petersburg Medical Center goes live with Cerner, with the Cares Act for COVID-19 relief helping cover the $1.3 million cost of CommunityWorks. The hospital vowed to replace its EHR in March 2021 following discovery that an employee had viewed patient records inappropriately. (12/13/21)
A new KLAS report looks at how enterprise EHR vendors meet patient access requirements (address verification, cost estimates, coverage discovery, eligibility verification, medical necessity, prior authorizations, propensity to pay, registration QA, and scheduling). Epic customers reported the highest satisfaction, those of Cerner expressed dissatisfaction with use of integrated third-party partner tools, and Meditech’s customers are very satisfied with what they call a workhorse product. (12/13/21)
The Spokane, WA newspaper talks to local patients and employees about the VA’s implementation of Cerner at the city’s Mann-Grandstaff Medical Center, reporting these issues:
- Two former senior VA officials who were involved in the project say it was misguided and is unlikely to improve on the existing VistA system.
- One hour after VA Deputy Secretary Donald Remy assured a House subcommittee that “The Cerner system works,” the system went down for 80 minutes and had at least some downtime 10 times in September and October. The system has gone fully down four times since it went live in October 2020.
- Former VA deputy CIO and CTO Ed Meagher said it is “absolute malpractice” that the VA did not anticipate performance problems by modeling workload against infrastructure, adding that otherwise, “you’re working off of Cerner marketing material.”
- Several veterans said they were unable to navigate the patient portal and it sometimes locks up and fails to deliver messages.
- Prescriptions were not transferred to Cerner, requiring mistake-prone manual re-entry that left some veterans without psychiatric and other chronic care medications.
- Employees sometimes have to fax medication lists when patients are sent to other facilities for emergency treatment that isn’t offered 24×7 at Mann-Grandstaff..
- The VA, which was the subject of a national wait-time scandal in 2014, has removed Mann-Grandstaff from the wait time web page because it hasn’t figured out how to measure wait times on Cerner.
- The VA’s training did not include the referral management module and one veteran whose urology referral was lost was found to have an untreated, aggressive form of prostate cancer when finally seen nine months later.
- A chief of anesthesiology said EHRs are billing systems with text editors tacked on while VistA was written by clinicians whose goal was to provide the best care possible. He says that Cerner told him that one online form requires 90 minutes to complete, and when doctors told the company that the nurse had under five minutes to examine the patient and document the visit, Cerner said they should hire more people.
- Meagher concluded, “What Cerner does best is capture billable events via exhaustive questions and back-and-forth as you input things. That’s what ties them up. They’re answering questions that are meaningless to them. They’re very meaningful to a commercial organization, because that’s how they get paid, but they’re meaningless to the VA.” (12/8/21)
VCU Health (VA) was scheduled to go live with Epic over the weekend, replacing Cerner. (12/6/21)
Zoom is accepting beta customers for its integration with Cerner, which includes notification of patient arrival in PowerChart, clinician sharing of test results and documentation, sending links to additional attendees, and placing patients in the Waiting Room for continuity between multiple caregivers in a visit. (12/3/21)
The VA revises its Cerner implementation timeline to restart the project in early 2022 and complete the rollout in 2024. The VA will also create two new positions to oversee the project, a program executive director for EHR integration and a deputy CIO for EHR. It named VA executive Terry Adirim, MD, MPH, MBA to the PED position. A VA update on lessons learned includes:
- Creating an EHR sandbox for clinician training.
- Optimizing the rollout schedule within VISNs.
- Assessing the capability of Cerner’s patient portal.
- Convening a safety summit this month to review how the VA will collaborate with local clinical stakeholders on informatics issues.
- Addressing issues raised at Mann-Grandstaff.
- Implementing a new management and governance structure.
- Finalizing a data strategy between VA and DoD. (12/3/21)
November 2021
Cerner names Johnny Luu (Google Health) as chief communications officer. (11/24/21)
A review of the de-identified Cerner EHR records of 490,000 COVID-19 patients finds that the use of SSRI antidepressants was associated with a 28% lower relative risk of death. (11/19/21)
The US Coast Guard finishes its deployment of Cerner as part of the DoD’s MHS Genesis project. (11/19/21)
Nasim Afsar, MD, MBA (UCI Health) will join Cerner as its first chief health officer in January. (11/17/21)
Representative Kim Schrier, MD (D-WA), a former pediatrician and Cerner end user, shares her concerns with VA Secretary Denis McDonough about EHR usability and its impact on patient care after she toured a clinic that is connected to the VA’s first live Cerner site of Mann-Grandstaff VA Medical Center (WA). She notes that employees have told her the system frequently crashes, forcing them to re-type lost notes; and that its self-scheduling and prescription management features are so buggy that patients have resorted to calling the clinic, resulting in overwhelmed phone lines. “If they have to scrap this version of Cerner,” she says, “it’s probably better to do that and use something that’s tried and true than to try to fix a system that is just broken from within.” (11/12/21)
A VA OIG review of its implementation of Cerner’s patient scheduling system finds that while many schedulers prefer the more user-friendly Cerner system over that of the replaced Vista system, they didn’t receive adequate training on complex scheduling scenarios and weren’t given enough time for practice. The VA also went live without resolving significant lapses in functionality, such as Cerner’s inability to automatically mail appointment reminder letters and to switch a scheduled visit between telehealth and in-person. Scheduling supervisors also reported confusion over measuring wait times, a nationally critical problem that the Cerner scheduling system was supposed to help resolve. After going live, care was delayed as permissions issues limited the ability of schedulers to book certain types of appointments, data migration problems required some information to be manually deleted, and reminder calls had to be turned off because patients were being told to check in at the front desk for visits in which on-site care was not available. (11/12/21)
A VA-conducted anonymous survey of employees of Mann-Grandstaff VA Medical Center finds that 83% say their morale is worse since Cerner went live last fall, 81% report increased burnout, 62% aren’t confident about using Cerner to perform their jobs, and 63% question whether they should continue working for the VA. A Congressional committee questioned whether the VA has moved on prematurely from its first implementation to focus on the upcoming one in Columbus. VA Deputy Secretary Donald Remy says he will visit Mann-Grandstaff, the VA will create a new position for someone with large-scale EHR implementation to oversee daily decisions, and the VA may create a deputy CIO position to oversee the Cerner implementation directly. (11/5/21)
Cerner reports Q3 results: revenue up 7%, adjusted EPS $0.86 versus $0.72, beating analyst expectations for both.
From the earnings call:
- President and CEO David Feinberg, MD, MBA says that EHR vendors have done a good job of automating processes and digitizing medical records, but their products haven’t reached their potential to allow caregivers to spend less time on the computer. He says one of his top priorities will be to improve system usability, a theme he repeated several times in the call.
- Feinberg says that Cerner has historically tried to do too many things, often without involving other companies. He says the company will focus on high-value areas, sometimes in partnership with others.
- The company says it is making end-of-life decisions for some less-profitable products. It will also end some low-value partnership arrangements.
- Client satisfaction that has “not been as high as it should be” has limited Cerner’s ability to pass along the Consumer Price Index escalators that many of its customer contracts allow.
- Cerner’s data business that is now known as Enviza is generating $130 million in annual revenue.
- Feinberg says that while health system mergers and acquisitions may create customer attrition, losing a customer who is disappointed with Cerner’s products and services “is something that is completely unacceptable to me.” He will meet with any customers that have been identified as unhappy in his first 100 days.
- Feinberg said in response to an analyst’s question about layoffs that companies can’t shrink their way to greatness. He said, “I think it oftentimes is a reflection of management not predicting where the business is going and getting folks retrained for areas of growth so that this stuff doesn’t happen. We need to right the ship, and I think that’s part of the process here. But in some ways, to me, it’s been lack of discipline and lack of focus.”
- Cerner’s employee count dropped by 1,000 from the end of Q2 to the end of Q3, equally split between layoffs and managed attrition.
- Asked about revenue cycle product consolidation, Feinberg said that it should have been done earlier, but the mindset was that anything built outside of Kansas City couldn’t be the best.
- Feinberg says that HealtheIntent offers a good strategy for population health management, but it needs to be streamlined and some of it is falling behind competing systems. (11/1/21)
October 2021
Cerner launches Cerner Enviza, an operating unit that combines expertise from Cerner and its acquired real world data vendor Kantar Health. (10/27/21)
Cerner President and CEO David Feinberg, MD, MBA confirms an anonymous employee’s Reddit comment that Cerner will lay off 150 workers in early November. (10/25/21)
Cerner President and CEO David Feinberg, MD. MBA kicks off the virtual Cerner Health Conference with a call to “eliminate the noise in healthcare” by getting the right information to the right people at the right time. He mentioned the essential clinical dataset, defined by 12 Cerner clients in 2016 as the EHR data elements that are essential for providing quality care. (10/13/21)
The VA hires an independent body to review its Cerner implementation and to provide an estimate of the project’s full cost. It expects to see the results in 12 months. The VA hopes that the review will finally capture all of its project-related expenses, including infrastructure upgrades that were omitted from previous estimates due to inconsistent cost tracking methods across its organizations. Conducting the review is Institute for Defense Analyses, a non-profit that administers three federally funded research and development centers. The most recent cost estimate was $16 billion versus its initial $10 billion price tag. (10/10/21)
Cerner launches RevElate as its single go-forward patient accounting system following years of high-profile struggles with Cerner Patient Accounting. The company says it will begin phasing in the product to replace existing Millennium and Soarian systems in 2023. A hospital CIO sent along these notes they took during the announcement:
- RevElate is based on the Soarian Financials platform.
- Former Soarian customers were electing to keep Soarian Financials while migrating to Millennium clinicals.
- Cerner Patient Accounting support will be phased out over the next 5-6 years. New sales will stop immediately.
- Patient access, charge capture, and the charge master will remain in Millennium, while patient accounting, including contract management, will be in RevElate.
- HealtheEDW is the go-forward strategy for reporting and analytics.
- Key development partners BayCare and Charleston Area Medical Center will initially deploy the system .
- Cerner clients that are upgrading to RevElate will undergo a six-month project.
- The product will be available to the full customer base in Q1 2023.
- Demos will be offered during the CHC virtual conference next week. (10/8/21)
New Cerner President and CEO David Feinberg, MD, MBA will kick off the two-day virtual Cerner Health Conference 2021 next week. (10/6/21)
Cerner announces — on new CEO David Feinberg’s first day of work — that it will require all US employees to be vaccinated by December 8, 2021. The company also extended its return-to-office date to January 10, 2022. Cerner had said on August 1 that it would leave vaccination decisions up to individual employees. Meanwhile, Epic reports that less than 0.5% of its headcount – which translates to under 50 employees – left the company instead of being vaccinated by its October 1 deadline. (10/4/21)
David Feinberg, MD, MBA takes the helm as president and CEO of Cerner. Predecessor Brent Shafer ends his three years and eight months with CERN shares down 6% versus the Nasdaq’s 101% gain. (10/4/21)
Cerner CEO-in-waiting David Feinberg, MD, MBA says he decided to leave Google Health because he wants to disrupt healthcare, improve lives, and affect healthcare quality and accessibility. He didn’t mention the $35 million compensation package that he gets for leaving the dismantled Google Health. (10/1/21)
September 2021
A new KLAS segment insights report looks at how 27 health systems define the term “digital front door.” Click the graphic above to enlarge. Epic customers turn to Epic first for digital front door tools, while Cerner customers more likely look elsewhere to companies like Amwell, Kyruus, R1, and Well Health. Companies that have successfully carved out niches include Kyruus (provider search and match and self-scheduling), Krames (patient education delivered via existing platforms), and Zoom (video visits). Those health systems reported that a wide variety of their C-level executives oversee their digital front door programs, ranging from CEO, CIO, CMIO, chief digital officer, and chief experience officer. Only one-third of respondents sought outside help to create their program. (9/29/21)
Clinical research network vendor Elligo Health Research raises $135 million in a Series E funding round. The company recently acquired research practice management organization ClinEdge. Existing investor Cerner, which returned for this round, also acquired life sciences analytics vendor Kantar Health for $375 million early this year and created the Cerner Learning Health Network EHR-powered clinical trials service for participating health systems in 2019. (9/27/21)
Children’s Health of Orange County joins Cerner’s Learning Health Network research consortium. (9/22/21)
A new KLAS report on data and analytics platforms finds that Cerner, Epic, and Health Catalyst have the deepest adoption among established analytics solutions, while Innovaccer has high adoption as a newcomer. Dimensional Insight customers report high satisfaction and see the company as a partner, while Cerner has a 40% overall dissatisfaction rate mostly due to overpromising. (9/22/21)
A GAO review of the DoD’s Cerner implementation finds that the system is live in six of 24 planned waves, system performance has improved, and early issues have been addressed. However, testing and resolution of the issues it raises remain unresolved, users say the training system doesn’t match production, and system change information isn’t being disseminated well. (9/22/21)
Former Cerner president and Livongo CEO Zane Burke joins consumer-focused care coordination and navigation company Quantum Health as CEO. (9/17/21)
Powell Valley Healthcare (WY) goes live on Cerner. (9/15/21)
The VA awards Cerner an 18-month, $134 million task order for its EHR rollout. (9/13/21)
A new KLAS report on EHRs in the Middle East and Africa finds that Cerner leads in performance and has improved relationships and services quality, Health Insights has improved satisfaction by migrating all customers to its web-based platform but hasn’t made a sale since 2019, and the sales success of InterSystems has caused some growing pains as customers report challenges in reaching its experts. (9/13/21)
August 2021
Former VA CIO Roger Baker says in a FCW opinion piece that VA should not take risks in trying to hurry its Cerner replacement of the homegrown Vista. He notes:
- Cerner should replace Vista only when its use is associated with improved care quality metrics.
- The VA needs to consider that Vista investment has been frozen several times since 2000 as the VA attempted to replace it, but it will remain in use for at least seven more years, meaning that the last facility to go live on Cerner will have been running Vista without any enhancements for 10 years.
- Cerner is missing about one-third of Vista’s capabilities, including registries, support for government-specific reimbursement and billing requirements, and medical equipment supply and maintenance schedules. Those functions will need to be supported even beyond the 10-year Cerner timeframe.
- Vista is the only backup plan for veteran care if the Cerner project fails, which is concerning as schedules are slipping and given the government’s poor track record of big modernization projects.
- VA and its contractors are losing the expertise needed to maintain and upgrade Vista. (8/25/21)
Cerner SEC filings outline the compensation package that its board is giving incoming President and CEO David Feinberg, MD, MBA, which adds up to nearly $35 million in his first 15 months:
- $900,000 base salary.
- Target cash bonus of $1.35 million.
- $13.5 million in restricted shares for 2022.
- $3.375 million in shares for Q4.
- A one-time cash bonus of $375K.
- A new hire award of $15 million in restricted shares to offset his equity loss with Google.
- Use of Cerner’s jet.
- Generous severance terms, such as change of control — two years salary, bonus, health insurance, and equity vesting.
In addition, outgoing CEO Brent Shafer gets his existing salary, bonus, and $2.5 million restricted shares for helping out during the one-year transition. (8/23/21)
Cerner hires David Feinberg, MD, MBA as president and CEO, effective October 1, 2021. He has been VP of Google Health since January 2019. Before that, he was president and CEO of Geisinger from 2015 to 2019. Cerner also announces that President Donald Trigg will leave the company. Cerner’s board has separated the roles of chair and CEO with the hire. William Zollars will become independent board chair on October 1, while Feinberg will become a board member. (8/20/21)
Cerner hires Lisa Collins, MBA (Accenture) as SVP of global services and Nithya Narasimhan (ADP) as SVP of client relationships in the East region. (8/18/21)
Adventist Health joins Cerner Learning Health Network. (8/16/21)
Cerner announces a new solution, Cerner Determinants of Health, which includes a dashboard and tools that are integrated with Millennium. Jvion will also integrate its SDOH and behavior health insights with Cerner’s products. (8/9/21)
Cerner is named as the hospital category winner in the ECR Now FHIR App Challenge for electronic case reporting for COVID-19 and other diseases of public health interest. Cerner’s solution sends a near real-time Electronic Initial Case Report to the Association of Public Health Laboratories AIMS platform, whose development was funded by CDC. The solution is open source and has been made available by Cerner to non-Cerner clients and EHRs. (8/4/21)
Cerner announces Q2 results: revenue up 10%, adjusted EPS $0.80 versus $0.63, exceeding analyst expectations for both.
From the earnings call:
- The company is increasing its earnings outlook for the year.
- DoD is live at 42 commands and 663 locations with 41,000 activated users. The Coast Guard’s deployment will be completed this year.
- Cerner says the results of the VA’s strategic review focused on governance, training, and readiness rather than Cerner-caused problems, consistent with the findings of an internal assessment that Cerner conducted earlier this year. It also notes that the DoD’s initial go-live resulted in similar required work in the 12 months following.
- The search for a CEO replacement for Brent Shafer continues and “has been very active.”
- The company continues to look for acquisitions that enhance Cerner’s competitive position, exceeds its cost of capital, is accretive over time, and creates shareholder value. Areas being considered cybersecurity, technology to support provider networks operating in both fee-for-service and fee-for value arrangements, and data.
- Cerner will continue selling unneeded office space that represents half of its owned property.
- The company laid off 500 employees in the quarter and eliminated 300 open positions, which will deliver $70 million in annualized savings.
- Asked by an analyst about Amazon’s HealthLake announcement, Travis Dalton said, “There’s a long history of big cap entry and big cap exit from healthcare. There’s an inherent complexity at the intersection of healthcare and IT. I see market interest in areas that we’re focused on is very validating of the growth opportunity that exists.” He added that healthcare data is dirty and requires normalization around Master Data Management.
- Cerner expects to have 80 provider organizations selling data to life sciences via its Learning Health Network by the end of the year. (8/2/21)
July 2021
Cerner will announce Q2 earnings Friday morning at 9:00 ET, which will be a much-followed event given its CEO search and takeover speculation. UPDATE: Cerner reports that revenue was up 10%, adjusted EPS $0.80 versus $0.63, beating analyst expectations for both. (7/30/21)
Cerner will sell its Continuous Campus in Kansas City, KS as a predominantly hybrid work model reduces its real estate needs. (7/30/21)
The VA tells the House Veterans Affairs Committee that it won’t bring any more sites live on Cerner for at least six months. From the hearing (in addition to misstating the Eastern time zone as “EST” above):
- Rep. Matt Rosendale (R-MT) said that despite the VA’s assurance, “we’re going to find out the proof is in the performance. If the army of crackerjack management consultants, and tiger teams, and advancement teams, and adoption coaches, and change management experts can’t make headway with the situation in Spokane, the reason is probably pretty simple. The software just isn’t any good, folks. Either that or it isn’t good for the VA.”
- VA OIG told the committee that VA’s modernization committee reported that 89% of users passed proficiency tests with a score of at least 80%, but OIG found an earlier draft stating that just 44% passed at that level, indicating that the report was altered before submission. The VA says it will consider disciplinary action if its investigation shows it to be warranted.
- Acting Deputy Secretary Carolyn Clancy, MD told the committee that “we will not be scheduling any deployments in the next six months” as the VA reviews infrastructure requirements and develops a new rollout schedule that will be driven by site readiness.
- Rep. Mark Takano (D-CA) expressed skepticism that the VA gave Cerner the minimum passing grade of “satisfactory,” questioning whether it did so just to avoid having the contract cancelled.
- Rep. Jim Banks (R-IN) expressed frustration with the project’s overall cost, noting that VA OIG’s list of missed items could swell the budget to $21 billion and also recalling that former VA CIO Roger Baker originally gave a number of $30 billion. The original project estimate was $10 billion.
- The VA is reviewing Cerner’s patient portal and its contractual obligations, with Dr. Clancy predicting that the end result will be a combination of Cerner’s product and the aspects of My HealtheVet that veterans like.
- Rep. Rosendale pressed Cerner executive Brian Sandager on why Cerner’s bid was so far off the mark even though the company was the sole-source bidder and thus the presumed expert. Sandager blamed changing requirements and lack of access to VA staff because of the pandemic. (7/23/21)
The Senate confirms Donald Remy, JD as VA deputy secretary, its second-highest official. He will take charge of the VA’s Cerner project. Remy, who was confirmed in a 91-8 vote, is an Army veteran and COO / chief legal officer of NCAA. (7/19/21)
Baystate Health (MA) expands its Cerner implementation with HealtheIntent for its physician organization and unspecified revenue cycle solutions. (7/19/21)
VA Secretary Denis McDonough tells the Senate Veterans’ Affairs Committee that he is putting the VA’s Cerner implementation on hold. This follows completion of a three-month project review that found serious “governance and management challenges.”
McDonough says that the VA’s first implementation at Mann-Grandstaff VA Medical Center (WA) in October 2020 did not live up to its promise of “seamless excellence in VA care,” adding that the report found “numerous patient safety concerns and system errors” as well as significant negative impact on productivity.
McDonough said he commissioned the review after hearing firsthand about duplicated prescriptions at Mann-Grandstaff and a user’s complaint that a Cerner help desk employee was unable to answer a user’s questions because he had just one week’s experience. He added that clinicians tell him that most of the integration between the respective Cerner systems of the VA and DoD happens inside their heads, not on their computers.
McDonough vowed to improve training and testing, to increase its oversight of Cerner, and to make leadership changes to get the project back on track. He also says the original plan to roll out Cerner by geographic area was a mistake and scheduling of go-lives will now be based on evidence of readiness.
The cost of the project, which was originally estimated at $10 billion when Cerner was awarded a no-bid contract in 2017, has risen to over $20 billion. McDonough has ordered a new budget estimate for the entire project, which will include the several billion dollars of infrastructure upgrades that the original estimate missed.
Committee chair Senator Jon Tester (D-MT) told the group, “I’ve had the impression for some time there are folks out there milking the cow. Every day they go out and they see this cash cow, and they’re getting every dime they can get out of it. There’s been damn little accountability. I hope Cerner’s watching this. Cerner’s not up to making a user-friendly electronic medical record, and in fact what’s transpired here is we’re going in the opposite direction, then they ought to admit it and give us the money back so we can start over.”
McDonough identified specific project issues:
- The VA lacks a specific definition of a patient safety issue and how to manage open issues.
- The decrease in productivity includes problems in revenue cycle, where much of the claims and payments process requires manual entry.
- Cost estimates did not include any issues beyond the Cerner contract, infrastructure readiness, and the project management offices.
- The VA did not create key performance indicators.
- The patient portal experience was fragmented, leading the VA to study the user experience to support “decisions on the future of the portal” that takes legal and contractual obligations into account.
- Testing did not reflect real-world workflow. (7/16/21)
Cerner SVP of Client Relationships Ben Hilmes, MHA joins Adventist Health as SVP / chief integration officer. (7/14/21)
Industry long-timer and Cerner SVP of Consumer and Employer Solutions David Bradshaw resigns. (7/12/21)
VA OIG looks at training deficiencies in the VA’s first Cerner rollout at Mann-Grandstaff VA Medical Center, in Spokane, WA, noting:
- The VA Office of Electronic Health Record Modernization is charged with the implementation, but the involvement of VHA, which houses all of the system’s users, is not clear.
- Training design was internally called “button-ology” because it focused on telling users which buttons to push to get a desired outcome, with little context provided to users who then failed to understand how to use the system.
- Users struggled because the classroom training didn’t focus on workflow.
- The system that was made available for user practice did not match the VA’s actual system.
- Cerner’s classroom trainers were not capable of answering questions and raised facility concerns because they lacked a clinical background and EHR knowledge. Users complained that Cerner’s trainers would defer many basic questions to the “parking lot,” which became a running joke among employees being trained.
- All of the 30 super users said their training was a waste of time that left them demoralized, distrustful of Cerner and the VA project team, and less prepared to help users than before the training.
- Leaders did not fully understand Cerner’s role-based permissions and how to manage staff who required multiple role assignments, causing users to be assigned to the wrong training classes.
- VA contracting officials scored Cerner’s training work as “satisfactory,” the minimum level that meets contractual requirements.
- The post-live decrease in user productivity and morale was attributed to EHR training factors.
- The project’s change management group withheld some OIG-requested training evaluation data and altered other data before sending it. (7/12/21)
A second VA OIG review of the infrastructure cost of implementing Cerner adds another several billion dollars to the project’s likely final cost. OIG notes, however, that the two infrastructure cost reports its office performed were conducted separately, so overlap is likely. The cost of the project, which was initially estimated at $10 billion and then $16 billion, could be as high as $21 billion if the estimates for cabling, user devices, and interfaces do not overlap. The VA – which OIG says underreported costs in its poorly documented estimates — agreed to all of OIG’s recommendations, which include having an independent cost estimate performed and ensuring that any additional project funding that is required is made available. (7/9/21)
Saint Vincent Hospital (MA) CEO Carolyn Jackson cites an ongoing nurses strike as the reason for the Tenet-owned hospital’s decision to delay its Cerner implementation until early next year. The strike, which mostly involves concerns about nurse-to-patient staffing ratios, has been going on for nearly five months. (7/7/21)
VA Secretary Denis McDonough reaffirms its commitment to its Cerner implementation as a review of the project concludes, indicating that any changes to the VA’s program will be announced within two weeks. (7/2/21)
June 2021
California launches its digital COVID-19 vaccination record system, built on the open source SMART Health Card Framework of VCI, whose members include Cerner, Epic, Meditech, Allscripts, HIMSS, and The Sequoia Project. (6/21/21)
A Defense Department MHS Genesis roundtable lists care improvements enabled by its Cerner implementation – real-time clinical decision support for newborns, improved tracking of service member health between duty station transfers, a reduction in visits for prescription management, and enhancing recruit readiness. The military says that the system improves care by standardizing workflows and processes. (6/18/21)
Captain James A. Lovell Federal Health Care Center (IL), a joint facility used by both the VA and DoD, will be the first test of interoperability between their respective Cerner implementations. (6/14/21)
Cerner lays off what it says is “hundreds” of employees. Unverified workers posted on Reddit:
- Speculation of the total number let go ranges from 1,000 to 4,000. UPDATE: A Cerner spokesperson says the actual number is 500 employees of its 26,000.
- Some of those involved say they worked on the company’s DoD and VA projects, and at least one employee who claims to have been affected says their developer jobs are being sent offshore.
- One says that shared services engineering had a 22% workforce reduction, while another said that 15% of Healthe are gone.
- Others said that several VPs were let go.
- Several say that Cerner fired new hires in its development and technical academies.
- Some speculate that the layoffs are intended to boost profit to make a rumored acquisition of the company more attractive. (6/11/21)
VA Secretary Denis McDonough says governance, transparency, and management issues will be top priorities for the department as the review of its Cerner roll out concludes. (6/9/21)
KLAS distills its information on each of the four major health system EHR vendors into individual “Complete Look” reports, which conclude:
- Allscripts — C- in product, C- in loyalty, 18% of customers report deep interoperability as adoption of DbMotion wanes. Sunrise has 4% of US hospital beds. Sunrise is an integrated, highly customizable platform, but Sunrise Ambulatory Care and Sunrise Financial Manager are not widely used. For transformational technology, significant interface maintenance is required since each system has its own database.
- Cerner — C in product, C+ in loyalty, 28% of customers report deep interoperability as customers benefit from its CommonWell connection. Millennium has 25% of US hospital beds. Cerner offers a broad Millennium suite that reduces third-party integration and is proven in both large and small organizations, but patient accounting is a weakness and the company’s less-prescriptive implementations lead to variability in customer success.
- Epic — B+ in product, A in loyalty, 63% of customers report deep interoperability with Care Everywhere and its connection to Carequality. Epic has 42% of US hospital beds. The company’s fully integrated suite has topped all software suites for 11 years running, is proven in big health systems, and offers a widely used patient portal and population health management solution, although it has a high upfront cost and some modules require in-house expertise to build.
- Meditech — B+ in product, A- in loyalty, 10% of customers report deep interoperability as most customers use point-to-point interfaces or HIEs, although its CommonWell connection is used by some early adopters. Expanse has 4% of US hospital beds. Meditech offers consistent development on Expanse, integrated offerings, and affordability that has made it the leading product for community hospitals, but Expanse costs more than the company’s legacy solutions and larger health systems have been historically hesitant to choose it. (6/9/21)
McLaren Bay Region (MI) goes live on Cerner. (6/7/21)
Cerner will offer its employees a hybrid working environment in the fall, with individual teams choosing their own time frames for returning to in-office work. (6/4/21)
Cerner is named to the Fortune 500. (6/4/21)
Syracuse Area Health (NE) will convert to Cerner this fall. (6/2/21)
May 2021
Six hospitals in Ontario, Canada go live on Cerner Millennium, which will provide a common patient chart across the four groups involved. Some of the hospitals went live without onsite help last fall since Cerner’s US employees were not allowed to enter Canada because of COVID-19. (5/28/21)
Another new KLAs report on application management and help desk services says that Nordic, Tegria-owned Cumberland, and HCTec execute strongly and communicate well in the “expansive” offerings category. NTT Data is transitioning to larger customers with a sharp drop in satisfaction due to staff quality and low executive involvement, while Cerner satisfaction has improved. Strong performers in the “broad” category include Ettain Health, GuideIT, and Pivot Point Consulting, while in the “niche” category, the top performers are Talon Healthy IT Services (Epic help desk), ROI Healthcare Solutions (ERP), Tegria-owned Bluetree Network, and Avaap (Infor). (5/28/21)
A VA OIG review says the VA underestimated the $16 billion budget for its Cerner implementation by $1 billion to $2.6 billion by failing to account for physical infrastructure costs, such as for electrical work and cabling. OIG also noted that the VA did not obtain the required independent cost estimate that would have allowed the omission to be identified. (5/28/21)
A new KLAS report on EHR market share in US hospitals finds that Epic gained the most in 2020, adding 101 hospitals representing 19,000 beds. Cerner saw its second consecutive year of net market decrease in losing 19 hospitals and 10,000 beds, which KLAS attributes to big-hospital concerns about its revenue cycle functionality. Epic’s market share is 31% of all hospitals and 42% of all beds, while Cerner has 25% and 27%, respectively. All the hospitals that Meditech added in 2020 were under 100 beds and 62% of its legacy customers that made EHR decisions in 2020 moved to other vendors, Epic in almost all cases. (5/21/21)
Cerner announces that Chairman and CEO Brent Shafer will leave the company. The company has hired a search firm to identify external candidates. Shafer will remain in the role until his replacement has been hired, then will serve as advisor for a year. Shafer, who was previously CEO of Philips North America, took the top Cerner role in January 2018. CERN share price is up 4% since Shafer took over. The Nasdaq composite index has risen 92% in that period. Cerner also announced Q1 results: revenue down 2%, adjusted EPS $0.76 versus $0.71, beating consensus expectations for earnings but falling short on revenue. From the earnings call:
- CFO Mark Erceg said that as a recently hired newcomer looking back at Cerner history, he thinks that the company’s lack of focus and sub-optimal execution hindered revenue and margin growth, placing it in the bottom quartile of shareholder return among its peer group.
- Brent Shafer said that he expects the new CEO to focus on operations rather than strategy development or portfolio management.
- Providers engaging patients at home has emphasized the need for a unified communications strategy for reaching consumers.
- President Don Trigg says that the entry of life sciences data competitors to Cerner’s Learning Health Network validates Cerner’s strategy and its investment in Kantar Health, also noting data opportunities with the federal government that go beyond DoD and VA.
- Cerner thinks that the federal government’s TRICARE program will provide opportunities in value-based care for data aggregation and longitudinal records. CDC is also a prospect and signed a real-world data contract in Q1.
- Shafer says Cerner is doing everything it can to be an attractive employer given the global competition for technology talent, emphasizing to prospective employees that they can make a difference in the world since their work involves healthcare. (5/7/21)
A new KLAS report finds that non-US EHR activity was strong in 2020, with 135 net new deals and 23 migrations, although 30% less than in 2019. The biggest winners were Epic, Dedalus, InterSystems, and Cerner. Epic’s market share in Canada has grown from three hospitals in 2016 to 146 now, but migration to Meditech Expanse is becoming more common. (5/5/21)
April 2021
The US Army’s General Leonard Wood Army Community Hospital (MO) goes live with MHS Genesis / Cerner, the first facility to use the system for in-processing of newly arrived trainees. Above is Major Cynthia Anderson, chief nursing information officer, overseeing use of the mass readiness module that was developed for military medicine and is used at GLWACH to process 100 trainees per hour. (4/30/21)
Northern Maine Medical Center goes live on Cerner. (4/28/21)
Black Book Research names Cerner as its top-rated inpatient EHR vendor as well as earning the highest client experience scores in academic medical centers. (4/28/21)
Leidos Partnership for Defense Health brings 10,000 clinicians live on MHS Genesis / Cerner in a wave deployment that covered locations in 12 states. (4/28/21)
Cerner chooses life insurance data vendor MIB Group to sell consented access to its 54 million patient medical records, adding to MIB’s list of EHR partners. (April 4/23/21)
The Patent Trial and Appeal Board upholds most of CliniComp’s data-sharing patent, as challenged by Cerner and Athenahealth. (4/21/21)
In England, London North West University Healthcare NHS Trust and The Hillingdon Hospitals NHS Foundation Trust will implement Cerner Millennium. (4/21/21)
CHIME, which recently ended its participation in the HIMSS conference, partners with the HLTH conference to offer Vive, an annual “reimagined health technology event” whose first conference will be held March 6-9, 2022 in Miami Beach. It will offer digital health innovation content, CHIME’s Spring Forum, an exhibit hall, and a matchmaking program that pairs potential buyer attendees with vendors. Some of the 18 title sponsors are also exhibiting at HIMSS21, but notable companies that will be only at Vive, at least according to HIMSS21’s exhibitor list so far, include Allscripts, Cerner, and Meditech. In an interesting adjacency of time and space, Vive will convene eight days before and 230 miles away from HIMSS22 in Orlando. (4/16/21)
The VA reaffirms that it will not bring its second Cerner site live in Columbus, OH until it has completed a strategic review of the project and shared the results with Congress, following concerns from users at the first site in Spokane, WA. (4/16/21)
Federal News Network digs into the problems VA clinicians have been dealing with during the transition to Cerner Millennium – a process that, despite initial reports of success, has prompted congressional leaders to call for a review before further rollouts are initiated. Users have noted an excessive number of clicks for certain tasks, data migration failures, dropped community care referrals, and needing to use Microsoft Teams to communicate with other users about EHR problems. The House Veterans Affairs Technology Modernization Subcommittee will meet later this week to review the $16 billion, 10-year project. (4/14/21)
Cerner wraps up its $375 million acquisition of Kantar Health, a data, analytics, and real-world evidence and research consulting subsidiary of New York-based Kantar Group. (4/2/21)
March 2021
VA Secretary Denis McDonough says in a House hearing that he is concerned about user productivity at its first live Cerner site, Mann-Grandstaff Medical Center (WA), raising the issue that the project’s cost could run over its $16 billion budget. (3/31/21)
Astria Health (WA) blames Cerner for its bankruptcy and the closure of Astria Regional Medical center in bankruptcy court, contending that Cerner fraudulently misrepresented that Millennium would integrate seamlessly with its revenue cycle offerings. Astria Health says its collections went from 97% of net revenue to 54% after Cerner’s billing system went live and the Medicare and Medicaid claims of its clinics were frequently rejected. Cerner denies the allegations. Cerner previously objected to the health system’s planned bankruptcy because Astria Health had $10.7 million in unpaid bills that it did not plan to pay because it said Cerner problems had cost it $150 million, but the parties resolved that issue in December 2020 and the bankruptcy proceeded. (3/26/21)
Cerner will enable EHR data retrieval to New York Life to reduce life insurance application processing time. (3/26/21)
VA Secretary Denis McDonough orders a strategic review of the VA’s Cerner EHR implementation. He said in an announcement that while the VA is committed to Cerner Millennium, problems with its use at Mann-Grandstaff VA Medical Center make “a strategic review necessary.” The VA says its ongoing post-deployment analysis at Mann-Grandstaff has necessitated a rollout schedule change, although Columbus remains as the next go-live site. The VA’s 12-week review will include optimizing productivity and clinical workflow and looking into patient-facing functions such as the patient portal, data syndication, and revenue cycle. Rep. Cathy Rodgers (R-WA) asked McDonough last Wednesday to launch an inquiry following reports of problems with prescription ordering, the patient portal, and user training. She calls the system “broken” and suggested a review of Mann-Grandstaff staffing, productivity, staff morale, training resources, and remaining infrastructure improvements. The GAO recommended in a report last month that the VA delay going live at additional sites until it resolves call critical problems at Mann-Grandstaff, which was its first center to go live in October. The VA responded that it agreed in principle, but would not delay further rollouts. Cerner provided a statement in response to the VA’s review announcement, saying that it supports the decision, that the company’s priority remains veterans and delivering solutions that drive care transformation in the VA, and that it is proud of its successes that include one of the largest health data migrations in history and deployment of a joint HIE between the DoD, VA, and community partners. (3/19/21)
The Defense Health Agency works with Cerner to develop MassVax, a COVID-19 vaccine management system the DoD is incorporating into MHS Genesis. (3/17/21)
Northern Inyo Healthcare District (CA) will implement Cerner Millenium through the CommunityWorks program. (3/3/21)
Naval Medical Center San Diego goes live on Cerner in the fourth wave of the DoD’s MHS Genesis rollouts. (3/3/21)
February 2021
General Leonard Wood Army Community Hospital (MO) employees prepare to go live on Cerner as part of the DoD’s MHS Genesis Cerner roll out. (2/24/21)
A new GAO report recommends that the VA stop its implementation of Cerner until all known critical issues have been addressed. The VA agrees in principle, but says it won’t stop the rollout and instead will test and mitigate risks. Most of the GAO’s data came from work performed last fall. VA has since closed most of the high-severity issues that GAO noted. Just 55 of the previous nearly 400 issues remain open.The VA says it will have all issues resolved by January 2022. Next up for go-live is Puget Sound Health Care System in Q4 2021. (2/15/21)
The IT director of 15-bed critical access hospital Syringa Hospital (ID) urges its board to stick with Cerner instead of following its plan to use Epic from Kootenai Health. The hospital says it is switching to gain cost savings and better connectivity to other Epic hospitals, but the IT director says it would “really grieve me” to re-do the work and warns that not all information will convert. She adds that Epic isn’t in the top five EHRs for small hospitals. A board member said she appreciates the input, but the IT director’s view is slanted because “that’s her baby,” adding that the board expected the hospital’s leadership to come to them with a recommendation and instead they were divided. (2/12/21)
In England, West Hertfordshire NHS Trust signs a 10-year, $41 million contract for Cerner. (2/12/21)
Cerner reports Q4 earnings: revenue down 3%, adjusted EPS $0.78 versus $0.75, meeting earnings expectations and exceeding on revenue. CERN shares dropped slightly on the news and down 1% over the past 12 months versus the Nasdaq’s 46% gain, valuing the company at $24 billion. From the earnings call:
- The company says it has reduced annualized operating expenses by $300 million in the past two years and has reduced its product set from 25,000 features to 400 products.
- Cerner expects to create a $1 billion health network business by 2025.
- Asked by an analyst how the company can simultaneously address losing market share to Epic as well as convincing customers to choose Cerner in innovative areas where it competes with new companies, President Don Trigg says Cerner was built to work on the current business as well as to identify new growth opportunities that may be adjacencies or new markets. They are looking at new buyer types beyond providers, such as payer, employer, government, and pharma.
- Trigg said in response to a question about how it will work with pharma contract research organizations following its acquisition of Kantar Health that Cerner’s differentiators are data as well as access to patients and providers. The acquisition allows linking data to support capabilities needed for late-stage drug trials.
- Cerner expects the acquired Kantar Health to generate about $150 million in revenue for 2021 even with COVID-19 slowdowns.
- The company may divest a limited number of assets in 2021, but is mostly interested in acquisitions.
- Health systems that participate in Cerner’s Learning Health Network share the revenue that Cerner earns from drug companies.
- Cerner’s federal business generates $1 billion per year and is growing at a mid-teens percentage rate. It sees opportunity in contracting with new agency work, especially on the network side, and the company will become more efficient with its experience as a prime contractor.
- The company took a $20 million charge that was due to an entity in the Middle East declaring bankruptcy. That entity wasn’t named, but I assume it was Belbadi Enterprises, a sole proprietorship that was formed by Abu Dhabi’s former health minister that signed a deal in 2008 to provide Cerner to UAE hospitals. Cerner was awarded $62 million, but was never paid, and then failed in its attempt to seize Oregon real estate that was owned by a related company. (2/12/21)
The 377th Medical Group at Kirtland Air Force Base in New Mexico will go live on Cerner Millenium in April as part of the DoD’s continued rollout of MHS Genesis. (2/10/21)
Cerner wins “Best in KLAS Software & Services 2021” distinctions in the top software suite and behavioral health categories. (2/3/21)
Four hundred Cerner employees will help administer COVID-19 vaccines at company headquarters later this week as part of the Operation Safe coalition in North Kansas City, MO. The coalition, which includes local hospitals and governments, hopes to vaccinate up to 4,500 people every other week. (2/3/21)
January 2021
A Black Book population health management poll of hospitals, practices, and payers finds that most expect to spend more for systems and integration, while one-third expect the government to offer incentives for providers who participate in information blocking rule fixes. Some of the PHM system vendors that score tops in customer satisfaction and loyalty are Azara Healthcare, Inovalon, I2I Population Health, Cerner, Datarobot, Casenet Trucare, and Epic MyChart. (1/29/21)
Consulting firm ReMedi Health Solutions assists a Northeastern health system with a virtual Cerner go live across 23 facilities. (1/27/21)
Cerner hires Mark Erceg (Tiffany & Company) as VP/CFO. He replaces Marc Naughton, whose departure was announced last fall. Cerner’s entire executive team has now been replaced since Brent Shafer was hired as chairman and CEO in January 2018, with the exception of Don Trigg, who was then president of Cerner Health Ventures and is now president of Cerner. (1/22/21)
New York State Office of Mental Health chooses Cerner’s hosted revenue cycle management solutions in a 10-year contract that covers 23 inpatient and 155 outpatient facilities. (1/22/21)
Cerner announces that Chief Client and Services Officer John Peterzalek and Chief Legal Officer Randy Sims will leave the company. They will be replaced by Cerner Government Services President Travis Dalton and SVP of Cloud Strategy / Chief IP Officer Dan Devers, respectively. Cerner Chairman and CEO Brent Shafer said in the internal announcement that the company’s annual client survey results require a greater sense of urgency in strengthening relationships, delivering on promises, innovating faster, and executing on strategies. (1/18/21)
AdventHealth’s replacement of Cerner, Athenahealth, and Homecare Homebase with Epic will cost $370 million in capital cost plus $290 million in operating cost, according to its J.P. Morgan Healthcare Conference presentation. AdventHealth, the former Adventist Health System, says Its first go-live will be in Q4 of this year and the last will be finished a year later. The Florida-based system has 50 hospital campuses in nine states, 2,300 employed physicians, 80,000 employees, and $12.5 billion in annual revenue. (1/15/21)
A Department of Defense annual review of its MHS Genesis Cerner implementation (thanks to reader Vaporware? for sending the link) finds that:
- MHS Genesis “is not operationally suitable because training remains unsatisfactory, dissemination of system change information is inadequate, and usability problems persist.”
- The system is operationally effective for basic operations in conventional clinics, but not for some specialty clinics and business areas.
- Performance scores increased from 45% of tested performance measures to 78%, with improvements needed in medical readiness, provider referrals, business intelligence, billing, coding, and reporting.
- System usability improved from “unacceptable” to “marginal-low.”
- The project has 158 open high-priority issues.
- Information exchange with required external systems was “sporadic, and the data were sometimes inaccurate and complete.” AHLTA-housed patient allergies, meds, and immunizations didn’t transfer to Cerner 13% of the time and care was sometimes delayed because of the manual reconciliation that was required.
- Cybersecurity experts found the system to be “not survivable in the complex, cyber-contested environment of a major medical facility.”
- Testing has not yet been performed to determine if the system can sustain the expected number of users at full deployment. (1/1/5/21)
Virginia Department of Behavioral Health and Developmental Services chooses Cerner’s EHR for four additional behavioral health facilities. (1/15/21)
Cerner says in its J.P. Morgan Healthcare Conference investor presentation that it will create a billion-dollar data business in selling de-identified patient data as real-world evidence to drug companies, partly driven by its $375 million cash acquisition last month of Kantar Health. (1/15/21)
Signify Research says the EHR market in Europe and EMEA in 2020 was better than in the US, which declined due to COVID-related financial challenges. It also notes that consolidation is picking up in Europe, with Dedalus acquiring Agfa’s HCIS business, CompuGroup Medical buying parts of Cerner’s non-Millennium assets, and the merger of big Nordics vendors Tieto and EVRY. (1/15/21)
Health and technology leaders announce the Vaccination Credential Initiative, which hopes to provide digital access to COVID-19 vaccination records using the open SMART Health Cards specification. Individuals could obtain an encrypted digital copy of their immunization credentials to store in a digital wallet or could receive a paper form containing a QR code. The goal of the initiative is to connect to The Commons Project Foundation’s CommonPass, which is being used for travel and return-to-work vaccine verification. Participants include CARIN Alliance, Cerner, Change Healthcare, The Commons Project Foundation, Epic, Evernorth, Mayo Clinic, Microsoft, Mitre, Oracle, Safe Health, and Salesforce. (1/15/21)
KLAS takes a look at the hospital EHR market in Canada, which in many cases involves group- or province-led collective decisions that are intended to keep costs down. Meditech leads Epic in hospital count, but has lost some market share as 88 big-system hospitals have replaced Meditech with mostly Epic from 2015 to 2019, while 31 legacy Meditech hospitals have upgraded to Expanse. Customers report satisfaction with Expanse, but say they could have used more guidance and best practices before going live and a better idea of the maintenance requirements afterward. Satisfaction with Cerner is stable, but customers say the Citrix-heavy client-server footprint requires a lot of maintenance, although experience with Cerner’s recently introduced remote-hosted option is good. Allscripts hasn’t had a new Sunrise sale in Canada in the past 10 years, Harris Healthcare is rarely considered in new deals, and Telus Health’s Oacis is rarely considered and hasn’t sold since 2015. (1/11/21)
Cerner VP of strategic growth Amanda Adkins leaves the company after losing her bid to unseat Rep. Sharice Davids (D-KS) in the November US House election. She had been with Cerner for 15 years, but took a leave of absence a year ago to campaign. She lost by 10 percentage points as the Republican candidate. (1/8/21)
December 2020
LRGHealthcare (NH), the bankrupt two-hospital, 162-bed system acquired by Concord Hospital, says it was paying $342,000 per month – 9% of its total revenue – to run Cerner. (12/30/20)
The Defense Health Agency awards Cherokee Nation Operational Solutions a one-year, $42 million contract to support DoD’s MHS Genesis rollout of Cerner. (12/30/20)
Cerner announces four new rural hospital clients of CommunityWorks. (12/28/20)
Washington-based Astria Health resolves Cerner’s objections to its bankruptcy reorganization plan, in which Cerner said it was owed $10.7 million that the health system it wasn’t said it wasn’t paying because its problems with Cerner billing caused at least $150 million in damages. (12/23/20)
A newly updated KLAS report on EHR interoperability finds that “deep interoperability” (access to outside data, easy location of patient records, visibility of outside data within EHR workflow, and positive impact on patient care) has improved considerably since 2017 except in the most important “impact on care” category. Epic is the clear leader in record-sharing, while Cerner is improving significantly and EClinicalWorks is doing well but isn’t proactive. Little progress has been seen for Meditech, Greenway Health, and Allscripts. Cerner has the highest adoption rate of APIs, especially FHIR ones, while Epic is being selective on which vendors it will work with and is less focused on APIs. (12/23/20)
Banner Health is using Cerner integration with Xealth to allow providers to order digital content and services from a single location in Millennium. (12/11/20)
Cerner invests in Elligo Health Research and will use its technology to offer clinical trial opportunities to providers and patients. Allscripts has offered Elligo’s services since 2017. The company was awarded an FDA grant in October 2019 to work on real-world data harmonization for 21st Century Cures Act data sharing use cases. (12/9/20)
November 2020
Cerner offers CommunityWorks clients a video visit platform that will be free through 12/31/21. (11/20/20).
Northern Health in Melbourne, Australia, will implement Cerner towards the end of 2022. (11/18/20)
A KLAS study of health system connectivity to post-acute care organizations finds that only Epic and Meditech provide solutions in all areas, as Cerner offers long-term and behavioral health modules but resells home health and hospice technology from strong performer MatrixCare. Netsmart has significant market share in standalone organizations that aren’t connected to health systems, having acquired solutions from Allscripts, Change Healthcare, DeVero, and HealthMedx, but customer satisfaction has dropped following post-acquisition lapses in support, development, and integration. PointClickCare is the strongest performer in long-term care, but no vendor consistently meets behavioral health needs. Records-sharing with acute care organizations from which referrals are sent is inconsistent, with Cerner and Epic having a high percentage of customers connected to CommonWell or Carequality, Meditech and Allscripts having low interoperability adoption, and the majority of users of all four systems reporting faxing as the most common method of exchanging information. (11/16/20)
Cerner incorporates Well Health’s app-free clinician-patient interaction capabilities into its HealtheLife patient portal, which will allow provider organizations to deliver health information, reminders, and virtual visit scheduling. (11/13/20)
The 673d Medical Group in Alaska, including the Eielson Air Force Base and Joint Base Elmendorf-Richardson, goes live on Cerner as part of the DoD’s MHS Genesis program. (11/11/20)
Naval Hospital Camp Pendleton (CA) goes live on Cerner as part of the DoD’s MHS Genesis program. (11/4/20)
October 2020
Cerner reports Q3 results: revenue down 4%, adjusted EPS $0.72 versus $0.62, beating Wall Street expectations for earnings but falling short on revenue. From the earnings call:
- EVP/CFO Marc Naughton will leave the company in 2021 after 29 years.
- An analyst noted that two recent high-level hires came from Leidos, suggesting an interest in getting more federal business, which Cerner hinted is the case. It was mentioned later in the call that Cerner is looking at “adjacencies” to its DoD and VA business, such as Indian Health Service, and “looking at ways that we can use data proactively with different branches of the government.”
- President Don Trigg says the next focus in its relationship with Amazon Web Services will be CareAware, also noting that Amazon’s PillPack pharmacy will play into pharmacy trends.
- Cerner had 22,000 people register for this month’s virtual Cerner Health Conference, with an advantage of the virtual format being able to see which sessions attendees choose and compare that to company focus and investment. Cerner mentioned interest in real-time workforce management, hospital operations, and consumer focus.
- Data opportunities include release-of-information for life insurance, legal, and workmen’s comp; the Learning Health Network; and clinical trials identification and enrollment for non-academic medical centers.
- Cerner will consider making acquisitions, but will also focus on repurchasing shares and paying dividends. (10/30/20)
A new KLAS report on health system AI purchases finds that that they are seeking specific solutions rather than concentrating on a single AI vendor, with the expected results taking longer than they expected. Jvion has a large client base but declining client satisfaction; Epic Cognitive Computing is growing fast, especially with readmission and sepsis prediction, but organizations need to drive outcomes on their own; and Cerner’s HealtheDataLab is early in its life cycle, with few live sites and little consideration in the market. Among products that allow customers to develop their own models, KenSci has high client satisfaction, DataRobot’s customers express concern about lack of completeness and the company’s lack of healthcare expertise; and Health Catalyst has weak customer satisfaction as its product is slowly maturing. Big tech firm offerings are seen as average, with Microsoft’s healthcare expertise and partnerships taking it to the top of the list, as Google and Amazon are perceived as light on healthcare knowledge and IBM Watson Health is seen as over-promising, under-delivering, and offering low value. (10/28/20)
Mann-Grandstaff VA Medical Center (WA) goes live on Cerner as the VA’s first implementation site. (10/26/20)
Cerner is seeking health systems to help test its Nuance-powered Voice Assist technology for clinician EHR interaction, joining St. Joseph’s Health and Indiana University Health. (10/21/20)
Intermountain Healthcare chooses Vynca for Cerner-integrated access to advance care planning documents for clinicians, patients, and caregivers. (10/9/20)
The VA tells a House subcommittee that it is considering retiring the My HealtheVet portal in favor of Cerner’s MyVAHealth, but that move would cost $60 to $300 million since it isn’t included in its Cerner contract. The VA will initially run the two portals in parallel, with Spokane-area veterans getting the Cerner portal by default after the Cerner go-live there this month, while all others will continue to access MyHealtheVet. (10/5/20)
The VA plans to go live with a first round of Cerner EHR capabilities on October 24 at the Mann-Grandstaff VA Medical Center in Spokane, WA, with a second round scheduled for next spring. (10/2/20)
Banner Health reduces unnecessary medication-related decision support and dosing alerts by one-third, working with Cerner Continuous Improvement Delivery to by studying its own alert history and implementing best practices from other Cerner clients. (10/2/20)
September 2020
Cerner will integrate Vynca’s advance care planning system with Millennium to display end-of-life preferences to clinicians and in the patient portal. (9/23/20)
In the UK, the Hampshire and Isle of Wight Integrated Care System will implement Cerner’s HealtheIntent population health management software and HealthEDW analytics. (9/16/20)
Adventist Health (CA) adds provider look-up and patient self-scheduling capabilities from Kyruus to its website, and embeds them within its Cerner-powered patient engagement software. (9/16/20)
Cerner hires Ron Lattomus (DRS Global Enterprise Solutions) to head its federal programs, including the VA’s EHR modernization project. (9/15/20)
Cerner will integrate AxiaMed’s patient payment solution with Millennium and other products. (9/14/20)
Four of Finland’s regions will work with Cerner to develop a digital platform to support moving municipal healthcare services under a regional authority. (9/11/20)
FCW reports that the VA’s implementation of Cerner’s scheduling solution in the Midwest’s VISN10 region will be followed by the full Cerner rollout there. VISN10 will go live on the VA’s 1.1 capability set for small and medium-sized hospitals. (9/7/20)
William Mintz (Leidos) joins Cerner as chief strategy officer. (9/4/20)
Cerner’s government services business receives a $161 million order to implement an enterprise healthcare services network at four VA medical centers in Ohio. (9/1/20)
August 2020
Cerner integrates its systems with Amazon’s new Halo, a health and wellness wearable, app, and membership program. (8/28/20)
The VA launches its Cerner appointment scheduling system at the VA Central Ohio Healthcare System, with a VA-wide rollout to follow. (8/26/20)
Baptist Health South Florida President and CEO Brian Keeley says the health system will spend upwards of $100 million on a digital transformation over the next several years that will include adding new scheduling and registration capabilities to its Cerner system; investing in analytics; upgrading its website with more patient engagement tools; and bolstering its Amwell-powered Care on Demand telemedicine app. The search for a chief digital officer is underway. (8/21/20)
The bond rater of Wise Health System (TX) says that one reason the health system’s margin has slipped is the cost of replacing Cerner with Allscripts, which in addition to staffing expense, created $12 million worth of revenue cycle inefficiency. It notes, however, that Wise Health Surgical Hospital improved its revenue cycle performance in 2019 following the EHR implementation. (8/19/20)
Starboard Value, the activist investor whose purchase of just 1.2% of Cerner shares convinced the company to give it four board seats in April 2019, reduces its CERN holdings to 2.6 million shares, about 0.8% of the outstanding shares, worth less than $200 million. CERN shares have gone up 16% since the day Cerner capitulated, although the Nasdaq has moved up 38% in the same timeframe. (8/17/20)
Cerner-sponsored Life Aid, which was launched in March to address veteran and first responder suicide, will be featured in a Discovery Channel special on August 30. (8/17/20)
Politico reports that the VA will re-commence its EHR overhaul with a rollout at an unnamed facility in October. The conversion from VistA to Cerner was halted earlier this year as VA facilities focused on preparing for and treating COVID-19 patients. The VA has switched its go-live plans from facilities in bigger metropolitan areas to those in smaller cities in the Pacific Northwest and Midwest, citing a lack of access during the pandemic to clinical experts who had been expected to help with system customizations for the larger facilities. (8/7/20)
Cerner and VC firm LRVHealth invest $6 million in Xealth, a Providence Health & Services spin-off that has developed software to help providers find and prescribe digital health apps and programs. (8/7/20)
July 2020
Nacogdoches Memorial Hospital (TX) and Cerner agree on partial payment to settle the $20 million the hospital owes for an implementation it delayed repeatedly and finally cancelled. (7/31/20)
Cerner will add Nuance’s virtual assistant technology to Millennium, allowing users to navigate by voice for chart search, order entry, and scheduling. (7/31/20)
Cerner reports Q2 results: revenue down 7%, EPS $0.44 versus $0.39, beating consensus earnings expectations but falling short on revenue. From the earnings call:
- The company says its revenue came in lower than expected because the pandemic impacted sales or timing of some low-margin offerings, such as technology resale and billed travel.
- Q3 revenue expectations have been reduced because of divested businesses and a larger-than-expected pandemic impact, but the company expects earnings to grow due to cost reduction.
- The company says it won’t cut R&D spending.
- Cerner says that while virtual go-lives work for simple implementations, the future model will be a hybrid, with fewer people on site who are supported centrally, which also reduces billable travel for the client. The company notes that employees are 25% more productive working remotely because avoiding two half-days of travel during the work week means they have five days billable per week instead of four.
- Cerner is looking beyond its Amwell virtual visit partnership to virtual hospitals and ICUs that would involve its CareAware platform.
- An analyst asked about a $35 million acquisition that he saw on the cash flow statement, which Cerner says was for a cybersecurity company that it can’t talk about otherwise.
- Cerner is interested in acquisitions related to research data and analytics.
- The grating phrase “new operating model” thankfully wasn’t uttered even once. (7/31/20)
Cerner announces CommunityWorks Foundations, a fixed-fee, cloud-based version of Millennium for Critical Access Hospitals that can be brought live in six months. (7/24/20)
Banner Health signs up for Cerner’s revenue cycle system, expanding its Millennium implementation. (7/17/20)
Cerner says it will keep employees working from home for at least several more months, pushing back its phased plan to bring up to 50% of employees back to office-based work. (7/17/20)
A new KLAS report that looks at advanced users of clinical communications platforms finds that Epic, Halo, and TigerConnect have the greatest breadth of workflows; PerfectServe and Telmediq have fewer workflows and are more widely used in inpatient settings; and Cerner, Hillrom (Voalte), Mobile Heartbeat, and PatientSafe Solutions focus on inpatient settings and have less use in outpatient. Cerner and Epic have tight integration with their own EHRs, as Epic Secure Chat provides fully embedded functionality and Cerner offers CareAware Connect Communications as a separate app. (7/8/20)
The White House’s 2021 budget request includes $105 billion for the VA, including $4.9 billion for IT and $2.6 billion (versus $1.5 billion this year) for its Cerner project. (7/8/20)
June 2020
Cerner conducts another round of layoffs, this time involving 100 employees. The nails-on-blackboard corporate phrase “new operating model” was uttered yet again as an explanation. (6/24/20)
The VA gives Cerner a $99 million task order for sustainment support of hardware and software associated with its $10 billion EHR modernization project. (6/12/20)
A GAO review finds that the VA has implemented effective configuration decision-making in its Cerner implementation by holding national workshops and creating 18 EHR councils, but needs to improve representation at local workshops. The report also notes that while the VA and DoD both user Cerner, coordination is needed to allow sharing of information and tasks, such as VA’s requirement to maintain durable orders for life-sustaining treatment across patient encounters that is not supported by the DoD’s Cerner configuration. (6/8/20)
Congressional sources say the VA probably won’t restart its Cerner rollout until the fall because of COVID-19 demands. (6/5/20)
RCM company R1’s shares jumped over 9% on the news that it will acquire Cerner’s RevWorks business in a transaction valued at $30 million. As part of the deal, Cerner will offer R1’s software and services to customers and prospects. In an April 2019 earnings call, company reps said RevWorks had grown stagnant, contributing $200 million in annual revenue. Cerner had been using its RevWorks offerings “to more tightly align the client to Cerner” for additional sales of its software and services. (6/5/20)
North Central Health Care (WI) will implement Cerner’s Behavioral Health EHR in three multi-specialty behavioral facilities. (6/3/20)
Cerner hires Jerome Labat (Micro Focus) as CTO. (6/3/20)
May 2020
Forty-nine municipalities in Sweden’s Västra Götaland region will implement Cerner Millennium. (5/29/20)
Cerner develops COVID-19 re-opening and social distancing projections for 60 countries using data from sources that include CDC, Johns Hopkins, Definitive Healthcare, and the COVID Tracking Project. (5/29/20)
Cerner joins the Fortune 500 largest US companies by annual revenue, coming in at #498. (5/20/20)
Cerner will begin moving employees back on campus Monday, starting with 10% of its workforce and aiming for no more than 50%. Employees will be encouraged to wear masks, fitness centers and cafeterias will be closed, elevators will be limited to two passengers, and staircases will be designated as one way. The company says positions in its consulting and client support areas may remain virtual permanently. (5/18/20)
Cerner announces that its annual conference, scheduled for October 12-14, will be conducted as a virtual event. The conference, one of Kansas City’s largest, is among 78 that have cancelled so far during the pandemic. City officials estimate that the cancellations will cost the local economy $137 million in lost hotel room bookings alone. (5/15/20)
Comments Off on Cerner News










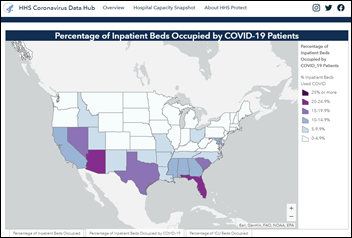



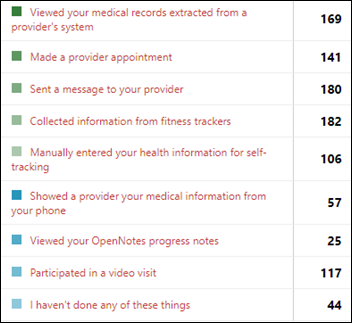


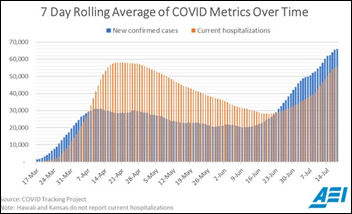












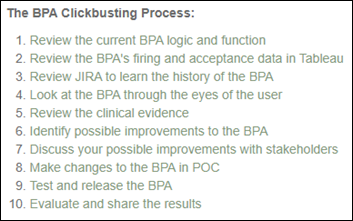


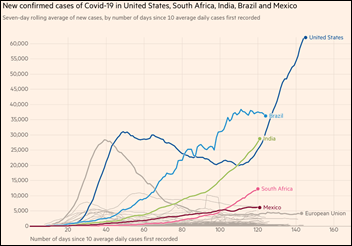












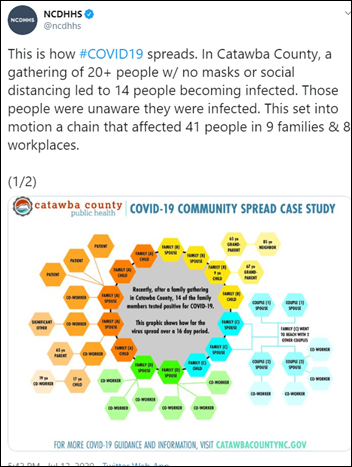
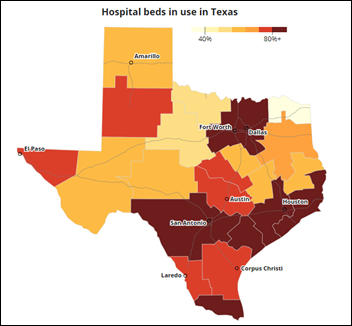

Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…