Katie the Intern 1/29/21
Hi, HIStalk! Hope you all are doing well. This column offers a different perspective, but speaks to working with IT and project management, surviving acquisitions, job termination, and how COVID-19 has paved this landscape of change. Hope you enjoy!

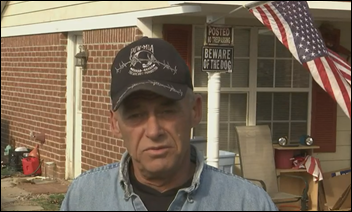
I spoke with Randy Burkert of Asheville, NC. He served until recently as manager of Mission Health’s Center for Innovation in Asheville. His early career was in engineering, but he moved to innovation work in 2013 to follow an interest in healthcare. While Randy did not work directly in IT, he described his job as working closely with stakeholders, IT resources, and tech companies.
Mission Health focuses on advanced medical care in western North Carolina. Randy used his experience with innovative processes, methodologies, and product development to manage the Center for Innovation. It worked to “promote and accelerate innovation opportunities that would have a transformational impact on our health system.”
“A lot of our time was problem seeking,” Randy said. “We successfully identified significant, measurable problems that we needed to be solved, that healthcare needed to be solved, and we went out to solve them.”
Randy’s team worked with vendors to apply solutions to problems. We talked about stakeholders and working with IT teams during this process through the lens of supporting an innovative process. I had little understanding of what “stakeholder” meant and how that played a role in project management, so Randy explained.
“An internal stakeholder is anybody who can provide valuable information relevant to the project that you’re going to work on who in turn will be impacted by that project,” he said.
Identifying stakeholders in a project is a critical first step. As an example, Randy told me of a solution for patients who are injured in hospital falls. The hospital pays those bills, which are not reimbursed by insurance in most cases. A vendor came to the Center with technology to reduce falls for inpatients. Stakeholders were unit managers, nurse leads, and CEOs, along with IT managers. In the early days when Randy worked with IT developers, their focus was supporting operations rather than working on innovation projects.
The innovation department created a devoted group of IT members who worked on multiple projects and had vast knowledge of all things IT. This team acted as a liaison to pull in other resources when needed, Randy said, and that model worked well for the Center.
Much of Randy’s work at the Center was done before Mission Health was acquired by HCA Healthcare in 2019. Randy offered advice about surviving an acquisition.
His first idea is that every employee should have an idea of their worth to the central network of a business. They should make sure their value is tied to that central or core network, as even though healthcare offers several models for innovation, there are greater values in healthcare services, such as a doctor’s services or IT’s problem-solving tech.
In the midst of the pandemic, the Center for Innovation was dissolved. In Randy’s opinion, this was due to innovation not being at the forefront of what the health system’s goals were. He stressed that innovation is important, but operational excellence was of higher importance after the acquisition. Over time, this meant that the Center was no longer essential to the functioning of HCA.
“We were able to operate for a pretty long period of time, but we didn’t know where or how to fit in,” Randy said. “When COVID came along, the financial pressures were significant to the health system, and they were making some tough decisions to cut back anything that was not a core function.”
HCA centralized a lot of roles, including IT support functions. Mission Health was a non-profit, community-run hospital, and HCA Healthcare is a national, publicly traded company. Adapting was tough, Randy said, but the center held on until COVID-19 hit the world.
“Having a dedicated set of resources in an organization that focuses on and drives innovation is a much more effective model,” he said. But, support and dedication are required even at the top level for innovation to be successful. Until that is done, innovation will not be successful no matter where it is.
Because of COVID-19’s impact on the healthcare system, Randy’s position was terminated in October 2020. He is looking for a job in which he can apply his engineering, innovation, and management skillset. He believes that COVID-19 has shown leaders that innovation can help organizations prepare for future disasters. “Technologies that have been around or have been moderately tested or applied or used, such as virtual care, really accelerated,” Randy said. “It has now become the new standard.”
———
TDLR; Katie the Intern spoke to a department manager of an innovation center about the importance of innovation and project management, acquisitions, and job termination.
That’s it for this week! I’ll back early February with my first virtual video interview / conversation. Until then, have a great one!
Katie The Intern

Email me or connect with me on Twitter.
































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…