News 5/5/21
Top News
R1 RCM will acquire digital payment solutions provider VisitPay for $300 million in cash.
R1’s acquisitions over the last several years have included Cerner’s RevWorks business and SCI Solutions, which it purchased for $190 million.
R1 says the acquired capabilities will allow it to lead the healthcare payments market in price transparency, flexible payment options, tailored communications, and analytics.
Reader Comments
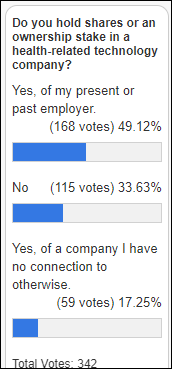
From PitViper: “Re: attrition. Are health tech companies experiencing it? What reasons are you hearing that staff are leaving?” I’ll let readers answer whether they see this as a trend.
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor NTT Data. Plano, TX-based NTT Data Services is a digital business and IT services leader, the largest division of trusted global innovator NTT Data Corporation, a top 10 provider and part of the $109B NTT Group. With the company’s consultative approach, it leverages deep industry expertise and leading-edge technologies powered by AI, automation, and cloud to create practical and scalable solutions that contribute to society and help clients worldwide. The Healthcare division within NTT Data Services is committed to improving patient outcomes by connecting the healthcare ecosystem. A recognized leader in healthcare, the global team delivers one of the industry’s most robust and integrated portfolios, including consulting, integration, interoperability, applications, data intelligence and analytics, hybrid infrastructure, workplace, RPA, cybersecurity, and business process services to help organizations accelerate and sustain value throughout their digital journeys. Thanks to NTT Data for supporting HIStalk.
I found this NTT Data overview video on healthcare digital transformation on YouTube.
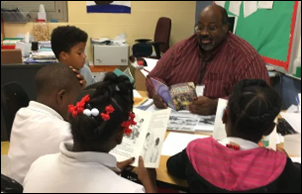
Reader Mike sent a generous donation from his COVID stimulus check to my Donors Choose project, which when paired with matching funds from my Anonymous Vendor Executive and other sources fully funded these teacher grant requests:
- Math materials from Ms. L’s elementary school class in Toppenish, WA.
- Acid rain test kits for Ms. H’s high school class in Cincinnati, OH.
- Multiplication flash cards for Ms. C’s elementary school class in Oklahoma City, OK.
- Biology and science resources for Ms. A’s high school class in Crewe, VA.
- Dinosaur learning activities for Ms. D’s special education class in New York, NY.
- Math games for Ms. V’s middle school class in Hosford, FL.
- Document camera for Ms. T’s first grade class in Buffalo, NY.
- Math games and books for summer learning kits for Ms. P’s third grade class in Tucson, AZ.
- Math manipulatives for Ms. T’s elementary school class of autism students of Staten Island, NY.
- 3D printing supplies for Mr. S’s second grade class in Cleveland, OH.
- A library of 13 read-aloud science books for Ms. H’s kindergarten class in Columbus, OH.
- Virtual whiteboards for Ms. S’s elementary school class in Indianapolis, IN.
Ms. V was among the majority of teachers who emailed their thanks almost immediately, explaining that her class has missed almost two years of in-person instruction due to Hurricane Michael and then the pandemic. She says, “Sending love and much appreciation for your support. We will start our summer program the first of June. These materials will go a long way towards helping our students recover academic loss due to Hurricane Michael, followed by the pandemic. Your support is a blessing for many. Thank you again!”
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Clinical documentation software vendor Provation acquires IProcedure, which specializes in cloud-based anesthesia documentation and perioperative data management.
Headway, which matches patients with mental health therapists in 11 states for virtual or in-person sessions, raises $70 million in a Series B funding round that values the company at $750 million.
Employer health benefits manager Collective Health raises $280 million in a Series F funding round, valuing the company at $1.5 billion.
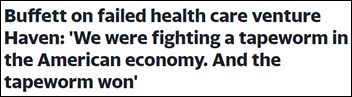
Berkshire Hathaway CEO Warren Buffett tells shareholders that Haven, the company’s joint employee-focused healthcare venture with Amazon and JP Morgan, failed due to its inability to overcome the challenges of working with so many different stakeholders on a problem that accounts for 17% of the country’s GDP. Buffett added that Berkshire Hathaway was able to identify inefficiencies and cost savings in its own healthcare pipeline, “so we got our money’s worth.”
Allscripts seeks to sublease 56,000 square feet of the nine-story building it occupies in Raleigh, NC for which it holds naming rights. The space is not needed since CarePort Health, which Allscripts sold to WellSky, won’t be returning employees to the building.
Sales
- Utah Navajo Health System will work with Emerge to consolidate its legacy EHR data with its Athenahealth system.
- St. Luke’s Health System (MO) selects automated operations software from Qventus to better manage patient throughput.
- Nexus Health Systems (TX), Grady Memorial Hospital (OK), and Duncan Regional Hospital (OK) select cloud hosting services for Meditech from Tegria companies Navin Haffty and Engage.
People

Moffitt Cancer Center (FL) hires Santosh Mohan, MMCI (Brigham and Women’s Hospital) as VP of digital.

Angie Stevens (Kaiser Permanente) joins Iron Bow Healthcare Solutions as chief strategy officer.


CereCore names Paul Fabrizio (NTT Data) and Mark Rowland (Nutanix) as regional sales VPs.

David Carr, RN (DeliverHealth) joins HC1 as executive director of high-value care.

Palantir Technologies hires William Kassler, MD, MPH, MS (IBM Watson Health) as its first US Government chief medical officer.

Ken Levitan, who was the CIO of Einstein Health Network from 2005-2015, is named president and CEO of that organization.
Announcements and Implementations
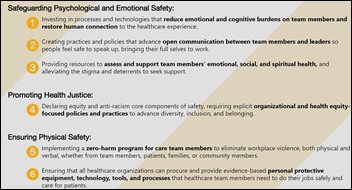
CEO Coalition — founded by Vocera Chairman and CEO Brent Lang and Chief Medical Officer Bridget Duffy, MD – develops a Declaration of Principles that has been signed by 10 health system CEOs who agree to principles that improve safety, well-being, and equity for healthcare workers.
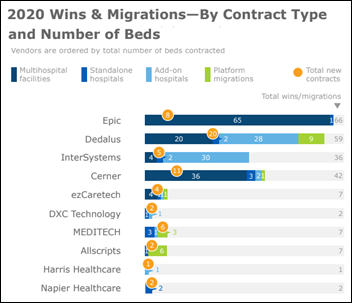
A new KLAS report finds that non-US EHR activity was strong in 2020, with 135 net new deals and 23 migrations, although 30% less than in 2019. The biggest winners were Epic, Dedalus, InterSystems, and Cerner. Epic’s market share in Canada has grown from three hospitals in 2016 to 146 now, but migration to Meditech Expanse is becoming more common.
Government and Politics
The State of Connecticut launches a statewide HIE dubbed “Connie.” The exchange is the fifth such project attempted over the last 14 years, to the tune of nearly $40 million. Forty-four organizations, including Hartford HealthCare, Yale New Haven Health, and the Pro Health Physicians network, have already signed on.
COVID-19

Public health experts say that the US will probably never reach the COVID-19 herd immunity of 80% given the circulation of variants and vaccine hesitancy, but even smaller numbers will make coronavirus a manageable threat that hospitalizes and kills far fewer people. They also say that while herd immunity is a national target, disease transmission is local, and areas with lower vaccination numbers will see more spread. Meanwhile, President Biden says federal focus will shift away from mass vaccination centers to drugstores and mobile clinics in hoping to vaccinate 70% of American adults with at least their first dose by July 4.
The federal government says it will redirect COVID-19 vaccine supplies that are allocated to individual states who don’t order them to other states that want more. This variability in demand, often along political party lines, means that hospitals in low-vaccination areas will likely see a hard winter as COVID-19 infections selectively ramp back up.
FDA will reportedly authorize use of Pfizer’s COVID-19 vaccine in people aged 12-15 years as early as next week.
New York City will resume 24-hour subway service in two weeks and will also lift all capacity restrictions, including museums, concert halls, restaurants, and Broadway theaters.
Other
Scripps Health (CA) continues to recover from a weekend cyberattack – apparently ransomware that also infected its backup servers — that forced it to divert some critical care patients, postpone appointments, and take several systems offline.
A Wall Street Journal reports says that corporate benefits executives are being overwhelmed by richly funded digital health startups for which they are the target audience. Those prospects say that too many startups are offering redundant or overpriced services and urge the companies to consider merging with others or offer deals to stand out in the crowd.
Sponsor Updates
- Built In honors CarePort Head of Product Sara Radkiewicz with its 2021 Moxie Award.
- Cerner publishes a new client achievement, “North Kansas City Hospital leverages Cerner technology to expedite COVID-19 vaccine distribution.”
- A Kyruus survey finds that two-thirds of consumers think virtual care will play a role where they receive care, cost and convenience are the most common decision criteria, and 60% say their preferred method for scheduling COVID-19 vaccine appointments is online.
- Clinical Architecture releases a new episode of The Informonster Podcast, “mCODE, CodeX, and Accelerating Healthcare Innovation – Part 1.”
- The Cyber Pro Podcast features CloudWave CTO Matt Donahue.
- Modern Healthcare includes Optimum Healthcare IT on its list of largest IT consulting firms.
- KLAS rates Divurgent as a market leader for speed and matching of resources in its “April HIT Staffing 2021 Performance Report.”
Blog Posts
- Celebrating healthcare heroes During Nurses Month (Ability Network)
- How charge aggregation technology can help billing companies (AdvancedMD)
- Leeds Hospitals go live with Agfa HealthCare’s Enterprise Imaging to improve image sharing across Yorkshire (Agfa HealthCare)
- Protected: Conditions of Participation for Medicare and Medicaid Hospitals: CMS’ ‘Carrot and Stick’ Approach to Bolster Real-Time E-Notifications (Audacious Inquiry)
- Considerations for Multi-Site Research Collaboration Data Collection (Bluetree)
- Health IT Infrastructure: Tips for Ensuring a Strong Networking and Technology Foundation (CereCore)
- How Providers Can Support the Telehealth Needs of Patients in 2021 (CoverMyMeds)
- Adaptability: The Key to Healthcare Technology Planning (Dimensional Insight)
- Spanish Updates for Healow (EClinicalWorks)
- Leveraging comprehensive consumer data to improve healthcare collections (Experian Health)
- Mike Alkire: Three Objectives Guiding Me As I Step into the Role of Premier President and CEO (Premier)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.








































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…