News 6/2/21
Top News
Physician networking site Doximity, which introduced a telemedicine service last year, hopes to raise $100 million in an IPO that would allocate up to 15% of its shares to qualifying physician members.
Doximity’s filing notes that it is used by 1.8 million medical professionals working in the nation’s top 20 hospitals and health systems.
The company’s revenue, which is largely subscription-based, jumped nearly 80% last year to $207 million.
HIStalk Announcements and Requests
Happy 18th birthday to HIStalk, which I started spontaneously on a Memorial Day weekend back in 2003 when I didn’t have anything interesting to do. I apparently still don’t.
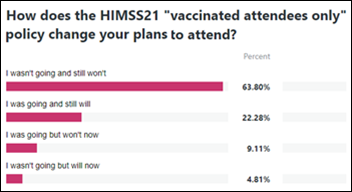
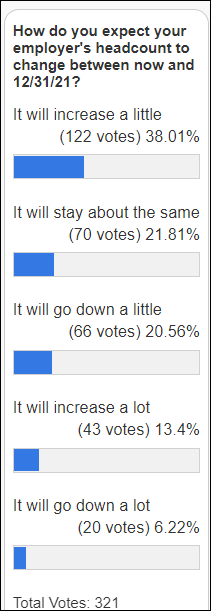
Slicing and dicing last week’s poll results shows that 29% of those who were planning to attend HIMSS21 won’t go because of the conference’s mandatory COVID-19 vaccination requirements, while 7% of whose who weren’t planning to attend now will. Announcement of the new policy failed to change the intentions of 86% of respondents, most of whom weren’t going to attend anyway.
New poll to your right or here: Which do you surreptitiously check three or more times daily during live or video work meetings? I edited the poll after posting it to include HIStalk just for fun although I doubt many folks (other than me) are pulling it up three times per work day.
Webinars
June 3 (Thursday) 2 ET: “Diagnosing the Cures Act – Practical Prescriptions for Your Success.” Sponsor: Secure Exchange Solutions. Presenters: William E. Golden, MD, MACP, medical director, Arkansas Medicaid; Anne Santifer, executive director, Arkansas Department of Health – Office of Health Information Technology; Kyle Meadors, principal, Chart Lux Consulting. A panel of leading experts will provide practical guidance on how to prepare for the Cures Act. Will it upend your business model? What is information blocking? How can standardized technologies be applied to meet Cures Act requirements? What must I do now as well as in the next five years?
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
CompuGroup Medical acquires Germany-based PACS and healthcare content management vendor Visus Health IT.
Virtual care company Babylon Health may go public via a merger with special purpose acquisition company that has lined up $270 million in funding in valuing the company at $3.5 billion. London-based Babylon’s first attempt at going public via an SPAC fell apart earlier this year.

Epic will require employees to return to work at its Wisconsin headquarters in part-time capacities beginning July 19. The company had attempted a similar return-to-work scheme last August, but dropped the plan after facing pushback from employees.
Clarity Informatics, whose back office software is used by 80% of GPs in England, is acquired by medical practice software vendor Agilio Software.
People

Industry long-timer David Madaffri (Philips) joins Mach7 Technologies as SVP of global sales.

Cone Health (NC) promotes CMIO Valerie Leschber, MD to SVP / chief medical officer.

Loyal hires Angela Jones, MS (Meazure Learning) as VP of customer success.

UofL Health promotes Debbie Mullins, MBA to VP/CIO.
Announcements and Implementations
Epic announces that its UGM 2021 – Stories of Legend and Lore – will be held as an on-campus event in Verona, WI August 23-25, 2021 for fully vaccinated attendees. Registration and hotel reservations open June 17.

Hampton Regional Medical Center (SC) opens a tele-ICU that connects ICU patients virtually with clinicians from telemedicine company Hicuity Health and Medical University of South Carolina, which provided grant money for the unit.

Syracuse Area Health (NE) will convert to Cerner this fall.
Surveyor Health develops SurveyorAI, technology that combines patient data with drug knowledge from First Databank to offer clinicians medication management tools for remote care, including risk stratification, clinical decision support, and educational resources.
Other
Doctors in England warn the public about NHS Digital’s plan to extract the medical data of 55 million people – everyone who has been registered in a GP clinic – in de-identified form to a database that will be made available for third-party research and planning. The Doctors’ Association UK says NHS DIgital has not done enough to explain to patients how their data will be used and how they can opt out. A medical confidentiality group cautions, “They’re trying to sneak it out. They are giving you six weeks nominally, and if you do not act based on web pages on the NHS Digital site and some YouTube videos and a few tweets, your entire GP history could have been scraped, never to be deleted.”

Insurer Lemonade, which portrays itself as a AI-savvy technology company, apologizes for suggesting in a since-deleted tweet that its AI analyzes non-verbal cues (physical or personal features) to automatically reject claims. The company – which sells homeowner’s, renter’s pet, and life insurance – clarifies that it uses facial recognition technology to detect claims that are submitted under more than one identity, but then sends those claims to human reviewers for a final decision. The company’s IPO filing says that its AI Jim chatbot system “handles the entire claim through resolution in approximately a third of cases … without human intervention,” but Lemonade admits that while it calls the system “AI Jim,” it uses plain old programming rules rather than the sexier-sounding AI do much of the work.

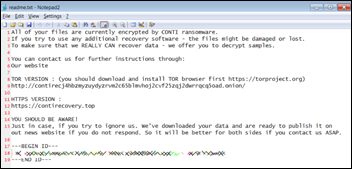
Sturdy Memorial Hospital (MA) reveals that it paid hackers an undisclosed amount of ransom after some of its systems were held hostage in February.
University of Washington researchers review several AI models that have claimed to be able to diagnose COVID-19 from chest X-rays and find that they rely on irrelevant data, such as patient position or age. They caution that such models therefore may not be generalizable outside the original setting, also noting that that most providers don’t use X-rays to diagnose COVID-19 anyway. At least one of the models has been deployed in multiple hospitals.
The New Yorker posts a sad, enraging article called “The Death of Hahnemann Hospital,” which describes how selling a historic hospital that served vulnerable patients to a private equity firm turned out to be a predictably bad idea.
Sponsor Updates
- Kyruus appoints Tina Brown-Stevenson (UnitedHealth Group) and Rob Coppedge (Echo Health Ventures) to its Board of Directors.
- Health Catalyst will present during the William Blair Growth Stock Conference June 2.
- SOC Telemed will present during the William Blair Growth Stock Conference and Jefferies Virtual Healthcare Conference June 2.
- Agfa HealthCare publishes a new white paper, “What is Enterprise Imaging, Really?”
- AGS Health meets KLAS/Censinet Cybersecurity Transparent Initiative requirements.
- Alcatel-Lucent Enterprise receives a 2021 Silver Medal rating by sustainability assessor EcoVadis.
- Ascom signs a six-year contract with a German hospital group for mobile IP-DECT communications and alarm solutions.
- CareSignal joins the Population Health Alliance.
- Cerner releases a new podcast, “Geisinger’s innovative approach to wellness and addressing healthcare inequities.”
- EnterpriseTalk features Change Healthcare VP of Platform and Marketplace Gautam Shah.
- CHIME will host its Summer Forum June 16-17 across three cities featuring eight past and present ONC leaders.
- PM360 features ConnectiveRx Product Manager of Enterprise Analytics Kylie Hall as part of its Elite 2021 Leader of the Future program.
- CloudWave is included on Modern Healthcare’s list of “Best Places to Work in Healthcare.”
- Divurgent VP of Technology Emily Carlson has been named one of Consulting Magazine’s “2021 Women Leaders of Technology” in the category of Innovation.
- Elsevier Clinical Solutions supports the State of California in expanding its COVID-19 online learning program for registered nurses.
- PatientPing announces that Innovaccer will become a reseller of its Pings real-time notification solution, embedding it within the Innovaccer Health Cloud.
Blog Posts
- Long-term care facilities now required to report COVID-19 vaccinations under new CMS rule (Ability Network)
- Blueleaf Banter: Improving Outcomes by Aligning Workflows with Technology (Bluetree)
- Measuring SNF Quality with the CarePort Quality Score (CarePort)
- Overcoming the Challenges of Balancing Patient Care and Administrative Functions (Vyne Medical)
- How to Maximize Patient Enrollment in Your Chronic Care Management Program (ChartSpan)
- Supporting the Breastfeeding Dyad During the Pandemic (Obix Perinatal Data Systems, developed by Clinical Computer Systems)
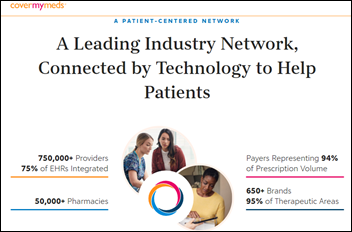
- Our journey to do bigger things – together (CoverMyMeds)
- A Prescription for Safety, Legibility, and Ease of Use (EClinicalWorks)
- Beyond the pandemic: digital patient intake is here to stay (Experian Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…