News 9/3/21
Top News
Baxter International will acquire Hillrom for $10.5 billion in cash plus assumption of debt that values the transaction at $12.4 billion.
The announcement emphasizes Hillrom’s recent refocus from manufacturing hospital beds to remote patient monitoring and connected care solutions.
Hillrom previously acquired cardiac monitoring company Bardy Diagnostics for $375 million, patient monitoring vendor EarlySense for $30 million, and clinical communications vendor Voalte for $180 million.
HIStalk Announcements and Requests
I was saddened to learn from Bill Bogutski that Vince Ciotti has died. Vince retired in 2019 after a 50-year health IT career, much of it spent working with Bill and other principals of the HIS Professionals consulting firm. The photo of Vince above is from a reunion of former employees of Shared Medical Systems in 2019. Vince spent considerable time over several years, starting in 2011, documenting health IT’s first decades for HIStalk readers in his engrossing HIS-tory series. I interviewed him two years ago and it’s still an entertaining read that will give you a feel for Vince’s filter-less, cynical humor. I asked him then what he wanted his epitaph to say:
If I could be remembered for anything, it would probably be my HIS-tory files, which I thank you for posting over such a long time, two and a half years. I hope some of the future CIOs read them and learn from them. I hope that’s what they remember me by, the guy that warned them about not repeating these mistakes of the past.
Webinars
September 16 (Thursday) 1 ET. “Patient Acquisition and Retention: The Future of Omnichannel Virtual Assistants.” Sponsor: Orbita. Presenters: Harris Hunt, SVP growth product, Cancer Treatment Centers of America; Patty Riskind, MBA, CEO, Orbita; Nathan Treloar, MSc, co-founder and COO, Orbita. Consumers want the same digital healthcare experience from healthcare that they get in online shopping, banking, and booking reservations, and the pandemic has ramped up the patient and provider need for frictionless access to healthcare resources and services. Health systems can improve patient acquisition and retention with the help of omnichannel virtual assistants that engage and delight. Discover how to open and enhance healthcare’s digital front door to offer care that goes beyond expectations.
September 16 (Thursday) 1 ET. “ICD-10-CM 2022 Updates and Regulatory Readiness.” Sponsor: Intelligent Medical Objects. Presenters: June Bronnert, MSHI, RHIA, VP global clinical services, IMO; Theresa Rihanek, MHA, RHIA, mapping manager, IMO; Julie Glasgow, MD, clinical terminologist, IMO. IMO’s top coding professionals and thought leaders will discuss the coding changes in the yearly update to allow your organization to prepare for a smooth transition and avoid negative impacts to the bottom line. The presenters will review new, revised, and deleted codes; highlight revisions to ICD-10-CM index and tabular; discuss changes within Official Coding Guidelines, and review modifier changes.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Healthcare Triangle files for an IPO that will raise up to $50 million.
Provation acquires Pentax Medical’s EndoPro endoscopy software.
Accenture acquires Canada-based healthcare technology consulting firm Gevity.
Sales
- Coalition of Asian-American IPA chooses CarePort Connect for care coordination.
People

SOC Telemed promotes Chris Gallagher, MD to CEO. He replaces John Kalix, who resigned his CEO and board positions.

Transcarent hires Snezana Mahon, PharmD (Evernorth) as COO.

Stephanie Solich (Zipari) joins VisiQuate as VP of client development.


Patient payment and engagement platform vendor Millennia names Dave Dyell as chief strategy officer and Doug Sundlof (Cloudmed) as SVP of sales.
LexisNexis Risk Solutions promotes Jeff Diamond, JD to president and GM of its healthcare business.
Announcements and Implementations
UC San Diego Health launches the Center for Health Innovation to develop, test, and commercialize technologies.
COVID-19
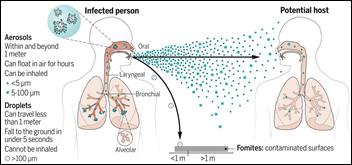
A University of California San Diego Health review of employee health records finds that COVID-19 vaccine effectiveness against symptomatic infection dropped from 90% in June to 66% in July, which the authors attribute to emergence of the delta variant, waning immunity suggesting the need for booster doses, and the ending of masking mandates. Adding to the argument for booster doses is that those healthcare workers who were vaccinated earlier were infected at a higher rate.
A New York attorney is suing hospitals that refuse to administer ivermectin to ventilated COVID-19 patients whose families insist.
Sponsor Updates
- Glytec will host “Time to Target: Uniting Around Patient Safety,” its inaugural conference on glycemic innovation and collaboration October 26-27.
- Everbridge wins two Silver 2021 Stevie Awards in the categories of customer service department of the year and customer service team of the year.
- The HCI Group releases a new DGTL Voices with Ed Marx podcast, “Soul-Stirring Kilimanjaro Clinic.”
- Healthcare IT Leaders publishes a new guide, “15 Tips for Patient Accounting System Project Success.”
- Ideawake releases a new video, “3 Health Systems Transforming Patient Care via Bottom-Up Innovation Programs.”
- Imprivata makes its digital identity solutions One Sign and Confirm ID available on Microsoft Azure.
- Infor publishes a new case study, “Bozeman Health raises quality of care and reduces waste with Infor.”
- InterSystems releases a new podcast, “How Can Healthy Data Save Healthcare?”
- Medicomp Systems releases a new Tell Me Where It Hurts Podcast featuring CPSI CMO William Hayes, MD.
- NextGate names Minakshi Tikoo, PhD (NYC Department of Health and Mental Hygiene) director of product management.
Blog Posts
- Balancing Healthcare Resilience with the Patient Experience (Everbridge)
- Five Actions to Help Prevent Opioid Overdose (First Databank)
- Digital Health Technology Deployed for Veteran Suicide Prevention (GetWellNetwork)
- Clinical Technology Disparities and Opportunities for Improvement (Halo Health)
- Six Tactics to Restore the Healthcare Revenue Cycle (Health Catalyst)
- The Value of ServiceNow IT Business Management (Optimum Healthcare IT)
- Telehealth Needs Your Help (Healthwise)
- T-Mobile breach exposed data of 40 million: How safe is your customers’ personal information? (Imprivata)
- What’s in a variant? Clinical documentation, epidemiology, and genomic sequencing (Intelligent Medical Objects)
- Healthcare Must Engage Patients and Clinicians as They Manage the Rest of Their Life (Medhost)
- How Meditech customers are supporting patients this Recovery Month (Meditech)
- 7 Tips for Leveling Up Your PT Practice Before 2022 (MWTherapy)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…