Top News

HCA Healthcare announces that hackers have stolen patient data from an external storage site used to automate email message formatting and posted it for sale on an online forum.
According to DataBreaches.net, the dataset includes 27.7 million rows, personal patient details, and information related to appointment reminders. The hackers made contact with HCA around July 4, and gave the company until July 10 to meet their unspecified demands.
Based in Nashville, HCA Healthcare manages the operations of 180 hospitals and 2,300 outpatient facilities in the US and UK.
HIStalk Announcements and Requests
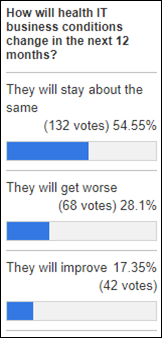
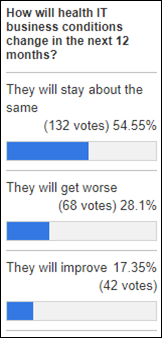
The pessimists slightly outweigh the optimists when it comes to health IT business conditions over the next year. IT/OPs_ProjectManager’s experience with recent IT staffing budgets certainly gives credence to the former: “The institution I work with has reduced budget for contracted IT staff and is purposefully throttling the IT project pipeline due to resource ($$ and people) constraints coming out of the pandemic. Knowing this plan makes me think the ‘non-core’ IT projects will be under much more scrutiny.”
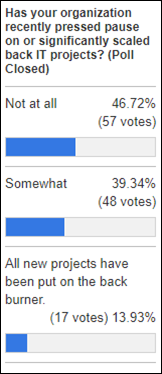
New poll to your right or here: Has your organization recently pressed pause on or significantly scaled back IT projects? Feel free to share observations as to why project priorities are changing, and what types of projects are still getting the green light.
Webinars
July 12 (Wednesday) 2 ET. “101: National Network Data Exchanges.” Sponsor: Particle Health. Presenter: Troy Bannister, founder and CEO, Particle Health. It’s highly likely that your most recent medical records were indexed by a national Health Information Network (HIN). Network participants can submit basic demographic information into an API and receive full, longitudinal medical records sourced from HINs. Records come in a parsed, standardized format, on demand, with a success rate above 90%. There’s so much more to learn and discover, which is why Troy Bannister is going to provide a 101 on all things HIN. You will learn what HINs are, see how the major HINS compare, and learn how networks will evolve due to TEFCA.
July 26 (Wednesday) 1 ET. “Lessons We’ve Learned Since Launching our Cancer Prevention Program.” Sponsor: Volpara Health. Presenter: Albert Bonnema, MD, MPH chief medical information officer, Kettering Health System, and Chris Yuppa, product owner for oncology services and cancer prevention, Kettering Health System. Kettering’s IT department has played a critical role in providing an EHR-driven framework to bring cancer risk assessment and individual prevention plans to more than 90,000 patients. Primary care, OB/GYN, oncology, and imaging providers are now able to assess the hereditary, genetic, and lifestyle factors that affect the risk of developing lung, breast, ovarian, colon, and prostate cancer in any patient encounter. Learn how Kettering brings together people, processes, and technology to be more proactive in the fight against cancer and where its cancer prevention program is headed next.
July 27 (Thursday) noon ET. “Why You Shouldn’t Wait to Use Generative AI.” Sponsor: Orbita. Presenter: Bill Rogers, co-founder, president, and chairman, Orbita. The advent of generative AI tools truly represents a paradigm shift. And while some healthcare leaders embrace the transformation, others are hesitant. Invest 20 minutes to learn why you shouldn’t wait. When combined with natural language processing, workflow automation and conversational dialogs, generative AI can help leaders address a raft of challenges: from over-extended staff, to the rising demand for self-service tools, to delivering secure information to key stakeholders. You will learn where AI delivers the greatest value for providers and life sciences, how it can solve critical challenges faced by healthcare leaders, and how Orbita has integrated generative AI into its conversational platform so healthcare leaders can leverage its full capabilities safely and securely.
July 27 (Thursday) 2 ET. “Denial Prevention 101: How to stop denials from the start.” Sponsor: Waystar. Presenter: Crystal Ewing, director of product management, Waystar. There’s a reason denial prevention is prominent everywhere in healthcare RCM. Denials reduce cash flow, drive down revenue, and negatively impact the patient and staff experience. More than half of front-end denials don’t have to happen, but, once they do, that money is gone. It’s a pretty compelling reason to take some time now to do some preventative care on your revenue cycle. This webinar will help you optimize your front end to stop denials at the start. We’ll explore the importance of not only having the right data, but having it right where staff need it, when they need it.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Automated provider credentialing and compliance software vendor Verifiable raises $27 million in a Series B funding round, bringing its total raised to $47 million since launching three years ago.
Sales
- Vandalia Health (WV) will implement Oracle Health across its system. Mon Health and Charleston Area Medical Center, both of which seem to have been Cerner customers, merged to create Vandalia last year.
- Adventist Health selects WinWire’s cloud-based data analytics and management software.
People

Aaron Neinstein, MD (UCSF) joins Notable as chief medical officer.
Announcements and Implementations

Consulting firm Healthcare IT Leaders forms an Elite Advisor group to offer peer-to-peer advisory services to healthcare executives.
Montage Health leverages Xealth’s digital health integration and digital prescription referral platform as a part of its digital health support programs for behavioral health, consumer wellness, orthopedics, and patient education.
Los Angeles Network of Enhanced Services adopts Google Cloud’s Healthcare API and BigQuery enterprise data warehouse.

Garrett Regional Medical Center (MD), part of the WVU Medicine health system, goes live on Epic.
Privacy and Security
Barts Health NHS Trust, the UK’s largest, reports a ransomware attack in which BlackCat hackers stole 70 terabytes of data. The group claims it is the largest healthcare data breach in UK history.
Other

Regenstrief Institute and Indiana University researchers develop natural language processing algorithms that can extract text data related to social determinants of health from within EHRs. The researchers say that their algorithms are easier to implement and use than more sophisticated risk models.
Sponsor Updates
- Meditech releases a new podcast, “Making transformative care attainable with genomic medicine and informatics.”
- Ethisphere recognizes Availity with its Compliance Leader Verification.
- Bamboo Health will exhibit at the AHA Leadership Summit July 16-18 in Seattle.
- CTG publishes a new case study, “CTG Helps Regional Healthcare System with Microsoft 365 Migration.”
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.

Comments Off on News 7/12/23




















The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en