News 11/17/23
Top News
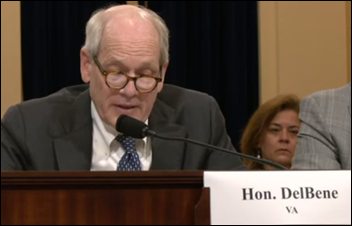
VA CIO Kurt DelBene tells a House committee that despite improvements, he has “significant concerns” about Oracle Health related to new incidents, failing to meet standards, end user responsiveness, and workflow.
On the positive side, the VA has had no complete system outages in six months.
Also from the hearing:
- Rep. Matt Rosendale (R-MT) cited a KLAS survey of VA employees in which only 26% said the EHR is available when they need it, leading him to question whether the VA’s help desk makes it too hard for employees to report problems.
- Deputy CIO Laura Prietula, MS, EdD blamed VA-approved customization of the base Oracle Health platform for its implementation struggle compared to the private sector. She added that the VA is now trying to reverse that customization and go back to out-of-the-box functionality.
- Rosendale cited a report saying that it will take Oracle Health 15 more years to match VistA’s functionality. Prietula responded that she doesn’t think it will take that long.
- Rosendale says that Oracle “hold themselves out as the experts in this field” but the VA’s VistA has 99.9% uptime and “it’s baffling that anyone could pay billions of dollars and set a lower standard.”
- Rosendale noted that the committee invited Oracle EVP Mike Sicilia to attend the hearing, but he didn’t attend or send an alternate.
Reader Comments

From Chip Ludd: “Re: CarePod. Serious Silicon Valley Kool-Aid is being slurped by anyone who thinks this will work.” The likelihood of success for this clinician-less health app kiosk in malls has two dimensions – whether it’s a viable business (which I doubt) or if it’s a medical breakthrough (which I’m sure isn’t the case). My reactions:
- HealthSpot went bankrupt in early 2016 after failing to gain traction for a similar offering even after installing its gadgets at the facilities of its partners Cleveland Clinic and Rite Aid. Higi offers a national network of free Smart Health Stations, but it was acquired for nearly nothing in early 2022 by Babylon Health, whose share price is also approaching near-nothingness. And everybody remembers the endlessly hyped but modestly featured Scanadu Scout tricorder-like device, whose 2017 shutdown after an 18-month study led some to call it Scamadu.
- Memberships cost $99 per month, and don’t include in-person clinic access. Insurance is not accepted.
- Customers still have to drive to a physical location, although finding a parking space at a dying mall shouldn’t be a problem.
- I would be hesitant about having my orifices penetrated by a machine that has a single, non-licensed attendant who will probably be so bored between breakdowns and reboots that they’ll hang out at Cinnabon.
- I assume that the company will need to navigate a regulatory maze in performing scans and blood draws using self-developed equipment that operates without clinician oversight.
- The company is investor-hungry, so it adds the obligatory AI connection – the box will perform AI searches of medical literature and generate a care plan that clinicians review. I’m not sure most of primary and preventive care requires real-time literature review.
- The gadget is a pivot for the company, whose core business is running a few clinic locations that they like to compare Apple Stores.
- The functions the technology can assess are limited compared to what a skilled human can perform in a real examination. Only so many sensors and algorithms are available and approved.
- The target audience seems to be young, worried well people who prefer faceless machines and tons of prevention-focused data or congratulatory test results to interacting with a clinician. That actually is a pretty good business model. Reviews for the company’s in-person clinics are almost all from customers in their 20s and early 30s.
- Forward attracted a fresh $100 million from investors, but this is an entirely different, capital intensive, and less-certain business mode than its actual operating business of running clinics.
- From a societal health perspective, convincing people that running app tests in a mall is equal or better to seeing an actual clinician is not a positive accomplishment, nor is a system that cares so little about consumerism and preventive health that people flee to the healthcare equivalent of a photo booth in front of a defunct Sears.
Also interesting is that the company’s clinics have mediocre reviews from their $149-per-month members, with comments like these making you wonder if investors are watching the company’s member retention rate (independent PCPs, especially direct primary care docs, everything you need for your marketing plan is right here):
- There’s no way to talk to a real human being on the phone, it’s all done through chat, and often the people I were chatting with didn’t understand the issue I was trying to explain to them. Wait times to see a doctor are horrendous, usually longer than 2 weeks. The app that they offer is mediocre and is much worse than record keeping systems used by other medical providers.
- Slow followup on things like bloodwork and other tests. Billing issues. Inconsistencies on providers & quality of care/advice. 10 out of 10 do not recommend.
- Tone def. Limited communication channels – no one available on phone. Virtual experience – not in person. They define your health priorities and disregard the health priorities that are important to you. They do not solicit your medical records – they rely on the patient to share that information. Not data backed guidance. The app is not intuitive – very poor user experience
- At my 1 year checkup recently, all that happened was collection of lab blood by staff and a report on my app without any guidance from my doctor. Fortunately, things are going well for me, but I would like to keep that going. I am looking for more of a partner in healthcare instead of a monitor.
- Initially had potential yet with physician turnover, outsourced labor and a lack of continuity in records and communication you are no better off than dealing with the typical primary care physician. Save yourself the money and perhaps try a different concierge-like medicine platform.
- I had a membership for several years and always had frustrations, mostly about the doctors and their poor advice. Eventually though I got tired of not getting prompt replies and having physicians change repeatedly, the new ones never seeming to bother with reading your history. They contradict each other. It really doesn’t feel safe. For example, they can’t administer the Covid vaccine. They can’t handle simple things like annual skin cancer exams. They take pictures of your moles and send them to someone. They have to send you to a specialist outside of their system for EVERYTHING.
From Dockside: “Re: BJC. I work there and the CEO aid in a town hall this week that the merger with Saint Luke’s in Kansas City is set to close on January 1, 2024. For now, the systems will operate as BJC HealthCare in eastern Missouri and Saint Luke’s Health System in western Missouri.” Unverified, but previously rumored as planned “by the end of the year” The merger would create a 28-hospital, $10 billion health system. I think they’re both running Epic.
HIStalk Announcements and Requests
I’m noting with grammarian interest the sudden pervasiveness of the word “lovely,” which I actually kind of like despite (or maybe because of) its time capsule images of grannies sipping tea pinkies-up on lace doilies. I hereby propose the resurrection of the similarly aged “splendid.”
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
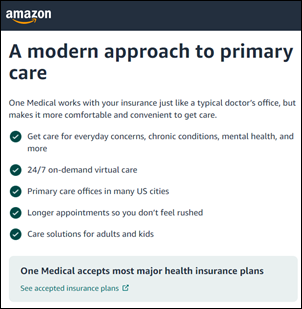
Primary care chain Forward Health raises $100 million in growth capital to roll out CarePod, which it calls “the world’s first AI doctor’s office” for members who pay $99 per month for access to the app-equipped kiosks that will be installed in retail locations.
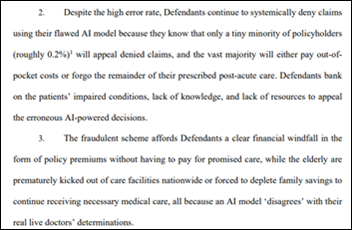
The estates of two deceased individuals sue UnitedHealth Group (UHG), alleging its AI algorithms, which came from its acquisition of NaviHealth in 2020, deny necessary care to Medicare Advantage seniors. The complaint highlights a 90% error rate in the AI system when its decisions are challenged, with the plaintiffs alleging that UHG’s Medicare Advantage patients receive substandard care compared to traditional Medicare patients.
The healthcare business that 3M will spin off in the first half of 2024 will be named Solventum.
Sales
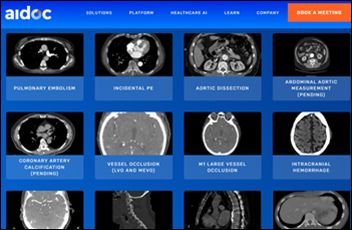
- University of Miami Health System chooses Aidoc to identify and triage abnormalities in patient images.
- Lee Health (FL) will offer virtual urgent care from KeyCare, which patients can launch from MyChart.
People

Elation Health hires Tom Natt (ConnectRN) as chief growth officer.

Greg Tracy. MS joins Wondr Health (ResMed) as CTO.

VCU Health hires Jeffrey Kim, MD (Loma Linda University Health) as CMIO.
Announcements and Implementations

Rimidi will provide its remote patient monitoring technology to Atlanta-based non-profit Brighter Day Health Foundation, which will offer RPM and chronic condition management services to underserved communities from local churches. Rimidi CEO Lucienne Ide, MD, PhD founded the company in 2011, and before her medical training, served as a signals analyst for the National Security Agency.
California health and social data-sharing organization Connecting for Better Health restructures as a non-profit and announces its initial board of directors.
Sectra will integrate its enterprise imaging diagnostic application for radiology with GE HealthCare’s AW Family Advanced Visualization applications.
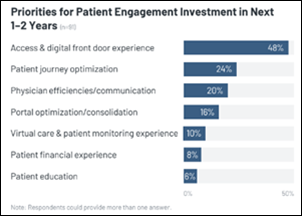
A new KLAS report on patient engagement finds that patient portals, patient surveys, and telehealth are widely adopted and health systems are moving on to implement provider search and patient self-scheduling. Two-thirds of respondents say their plans involve their EHR vendor, either alone or with third-party solutions, with 58% of Epic-using respondents and nearly as many Meditech customers saying that the vendor aligns with their plans, while one-third of Oracle Health’s customers say the same. Technologies most mentioned for consolidation are virtual care and patient communications.
Privacy and Security
Mail order pharmacy fulfillment vendor Truepill files a breach notice that the information of 2.4 million people was exposed in an August cyberattack.
Other
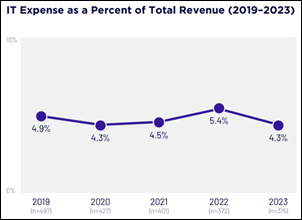
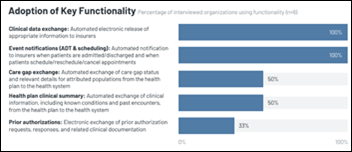
Snips from the Digital Health Most Wired 2023 survey:
- Health system IT budgets have stabilized, with most returning to pre-pandemic levels and likely to increase as they acquire technology to address labor shortages, wage inflation, and reduced margins.
- They are looking for solutions that offer a clear, measurable ROI.
- The average Digital Health Most Wired score has increased steadily from 63% in 2019 to 77% in 2023.
- An ever-increasing amount of stored data has increased use of advanced analytics, although often involving multiple vendor solutions across locations and departments, with limited integration.
- End users need to improve their understanding of how to use data, but scaling education programs is hard as systems rapidly evolve.
- Health systems are trying to integrate data from patient-wearable devices into their EHR.
- The role of the CIO is becoming complex as cybersecurity, innovation, and analytics require leadership that may or may not fall under the CIO’s oversight.
- Few large health systems place cybersecurity under the CIO, as 90% of them have a CISO or other VP-level position.
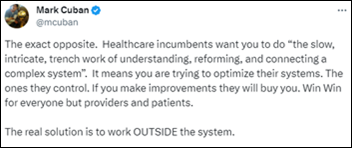
Mark Cuban disagrees with a tweet that says Big Tech won’t disrupt healthcare, offering a detailed response that I’ll summarize:
- Tech companies that claim to “optimize” the system are improving only its rent-seeking aspects.
- Healthcare consolidation has used lack of transparency to “extract rents everywhere and anywhere they can” so that nobody can see who pays how much.
- PBMs and insurers add complexity and are not needed given the ability for employers to contract directly with providers, adding that “is it really insurance if they do everything possible not to pay claims?”
- Providers know that contracts, pricing, and network games that big insurers play are ruining the quality and cost of care, but they are too scared to speak up.
- Employer CEOs don’t understand that they are enabling the status quo by working with incumbents, but they are finally realizing the need to change for financial and employee wellness reasons.

UCLA sues Mattel for reneging on its 2017 pledge to donate $49 million to its children’s hospital, claiming that the toymaker is instead offering a few million dollars plus a bunch of toys. UCLA wants the full $49 million plus damages, but Mattel says the donation was earmarked for adding a new tower to UCLA Mattel Children’s Hospital that UCLA decided not to build.
Sponsor Updates

- CHIME gives its 2023 collaboration award to Ellkay and Signature Healthcare.
- Eric Sellari joins Health Data Movers as account manager.
- Biofourmis and HealthXL publish a report titled “Unlocking the Value of Digital Measures in Drug Development.”
- Ascom Americas names Kim Hendrix, RN regional director, Healthcare Alliance.
- The Outcomes Rocket Podcast features Availity AuthAI CTO Rob Laumeyer, “We Can’t Make Healthcare Error-Free, But We Can Make the Errors More Traceable.”
- AvaSure publishes a new guide, “AI Powered Enhancements for Your Virtual Care Workflow.”
- Nordic releases a new episode of its “In Network” podcast titled “Designing for Health: Interview with Margaret Lozovatsky, MD.”
- Bamboo Health will exhibit at the Medicare Star Ratings Summer December 6-8 in Orlando.
- Bardavon joins the National Safety Council’s TechHub Marketplace.
- Recent KLAS reports recognize Care.ai’s virtual care solutions based on the company’s expert staff, premium hardware, and advanced AI features.
- The This Week in Pharmacy Podcast features CereCore Physician Consultant Charles Bell, DO and CereCore Manager Andrea Corner, PharmD, “Pharmacists and Physicians Refining the EHR.”
- Clinical Architecture releases a new Informonster Podcast, “Documentation in the OR with AORN.”
- KLAS Research’s 2023 Data & Analytics Platforms Performance Report names Dimensional Insight a top performer.
- Divurgent releases a new Vurge Podcast, “Exploring the Power of Data and Analytics in Healthcare.”
- EClinicalWorks announces that Moreno Valley Physician Associates (CA) has successfully implemented its new AI assistant tools.
- First Databank receives the American Medical Informatics Association’s Silver Corporate Partner Award for its contributions to the association and the field of informatics.
- FinThrive relocates its corporate headquarters to Plano, Texas.
Blog Posts
- Minimizing administrative burden to maximize data insights and healthcare impact (Wolters Kluwer Health)
- The RCM Maturity Framework: A Path to Digital Transformation and Operational Excellence (AGS Health)
- Unlock healthcare productivity with data portability: A path to provider well-being and enhanced patient outcomes (Arcadia)
- Addressing Workforce Challenges and Keeping Patients Safer: How CHS is Deploying Virtual Patient Monitoring (AvaSure)
- How Technology Can Help Providers Get Paid and Common Challenges (CereCore)
- The Benefits of AI in Healthcare Are Vast, So Are the Risks (Clearwater)
- Using High-Impact Point-of-Care Messaging Without Third-Party Cookies (ConnectiveRx)
- Finding the Needle in the Tech Stack: What to Look for in a Platform Engineering Services Partner (CTG)
- 3 Takeaways from KLAS Research’s Data and Analytics 2023 Report (Dimensional Insight)
- The Evolving Role of Hiring Managers in Remote Work Environments (Direct Recruiters)
- Strategies to Prevent Coding Denials and Increase Revenue (EClinicalWorks)
- Beyond Alert Fatigue: Understanding Roadblocks to Customizing Medication Decision Support (First Databank)
- Supporting Mental and Behavioral Health (Findhelp)
- Improving the Efficiency of Healthcare RCM: A Key to Financial Health (FinThrive)
- Healthcare cybersecurity threats: October 2023 (Fortified Health Security)
- Hands Off! How You Can Protect Patient Data from Unauthorized Intruders (HealthMark Group)
- Tips for a Blended Content Strategy (Healthwise)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.























This is a great point—many discussions about patient wait times still focus on staffing or technology, while the real issue…