Chris Molaro, MBA is co-founder and CEO of NeuroFlow of Philadelphia, PA.

Tell me about yourself and the company.
I come from healthcare as a patient, first and foremost. I am an Army veteran, a West Point graduate, and went to the Wharton School for an MBA. I met a psychiatry professor there and that’s where NeuroFlow got its start. NeuroFlow is a digital health platform that helps assess and triage a population of behavioral health conditions in non-behavioral health settings, like primary care, and helps patients get to the right level of care, keeping them engaged and measuring outcomes over time.
You were deployed to Iraq as a platoon leader in combat. What is your experience with the military’s system for behavioral care?
A lot of people are probably intimidated about the military, or the government healthcare system, because of lack of knowledge or experience with it. In reality, it’s just a giant integrated delivery network, a giant at-risk payer-provider system. It’s obviously the biggest in terms of resources and so forth. When I was serving from 2006 to 2015, there was a tremendous amount of resources and investment, in particular on the mental health side. We were a number of years into the conflicts in Afghanistan and Iraq. PTSD was well known and it was discussed and talked about. There wasn’t a shortage of investments and resources or the supply of those resources.
The challenge is similar to what you see in the non-government space, which is identifying those issues, getting people with those issues engaged, providing them access, and offering them ongoing support at the right time and at the right place. It’s a challenge, especially because of the stigma that is associated with the mental health space. People are, for whatever reason, ashamed, embarrassed, and maybe concerned about their job security or their ability to succeed professionally, so there was a reluctance to get that care. That was a challenge in the military, but from my NeuroFlow perspective in working with a lot of commercial partners, we see that same thing transcend into the civilian population.
How can technology help bridge the chasm between physical and mental well-being, which involves different providers and insurance requirements?
In the world today, 40 to 50 million people a year have a behavioral health issue. Looking at claims data, we know that two-thirds of them will never get it treated. That’s a huge problem. Imagine if we said that two-thirds of people with cancer never get it treated. That would be a tragedy. That same thing is happening in mental health today.
The highest prescribers of antidepressants in the country are PCPs. They don’t have that nuanced understanding about where to send someone. Maybe psychiatrists have a long wait time, which is true across the country, so PCPs fill that gap. The problem is that no one ever follows up. There’s no continuity of care.
The good news is that there’s a ton of integrated care models, specifically the psychiatric collaborative care model, whose outcomes and significance has been proven through 80 or more randomized controlled trials. The challenge is that it’s incredibly difficult to scale and it’s incredibly expensive. You hire psychiatrists, you train them, and you integrate them with PCPs or other providers like OB-GYNs and pain management doctors. It adds to the work and the workflow.
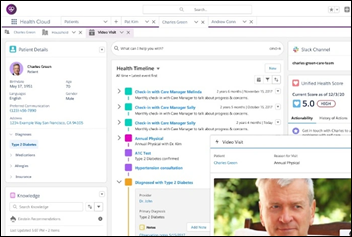
That’s where we think technology can help. Technology can help automate a lot of the workflow that is required for collaborative care, allowing the providers to operate at the top of their licensure. You can reach more people without needing more resources, scaling something that historically only the best-funded academic medical centers could do. Now you can make it more accessible throughout the healthcare system.
How does the psychiatric collaborative care model work in real life?
A lot of people will say they do integrative care or co-located care. They physically embed a social worker, psychologist, or psychiatrist with the primary care provider. That’s a great first step, but according to the academic model that was first studied and researched at University of Washington, that is not the collaborative care model.
The collaborative care model is a triangular, team-based approach, where a behavioral healthcare manager works hand-in-hand with a primary care provider, or other medical provider, to help identify patients who have mild or moderate behavioral health issues. Then if appropriate, they keep them in the primary care clinic instead of referring them out. They refer them if they are higher risk or if they need a higher level of care, but then there’s a psychiatric consultant there to help guide the PCP in how and what to prescribe.
This removes the burden placed on the dedicated behavioral health providers who are already in short supply. It gets the highest-risk patients to the dedicated behavioral health providers while keeping the lower-risk people treated within the medical provider, the PCP or otherwise. It’s a better allocation of resources and better continuity of care.
Does the traditional model create a blind spot for PCPs who refer patients who don’t follow up, leaving the PCP unaware that behavioral care never happened and leaving no electronic trace in claims data?
In a lost referral, I’m a PCP, I refer you to a therapist, and after you leave my office, I have no idea if you followed up, if you’re getting the care that you need, and how that’s impacting your other chronic conditions. Think about someone who has hypertension or diabetes. Most of those people have a co-occurring behavioral health issue. They are four times more expensive on an annual basis – they are higher healthcare system utilizers or have higher prescription spend than someone with just the chronic medical condition.
The collaborative care model tries to close that loop. Without technology, that’s a very manual process. I have to call everyone who is enrolled in the model and do monthly follow-up and assessments. It gets burdensome and time-consuming. Technology allows you to do that in a more automated fashion so that those resources connect over voice or in person only with the people who need that higher level of touch.
Employers bear some of the cost of behavioral health issues in the form of abseentism and lost productivity. Does the market address those people, who are probably insured and may receive behavioral health benefits, from others whose needs are similar but who don’t receive employer or insurer support?
That’s precisely it. If there’s a silver lining of the last two years in the pandemic, it’s that as a society, there’s a light that is shining on this mental health conversation. More than ever, people are acknowledging that there are challenges here. We have all felt them at home, and we’ve seen that in the workplace now. The ability to have this more integrated care model not only helps the cost of care, it improves the outcomes. The interesting thing is that we measure not only improved mental health outcomes, like a decrease in depression or anxiety, but you also see improved A1C levels, pain levels, and outcomes on the physical health side.
On the employer side, NeuroFlow does work, some of which is public, with groups like Aflac and Prudential to support their short-term and long-term disability business. That’s relevant because even if people aren’t in disability for mental health reasons, the mental health aspect of being lonely, away from your work, depressed, or recovering has a huge impact on their productivity and getting them back to work. We help their disability claimants and beneficiaries get better faster with the integrated care model.
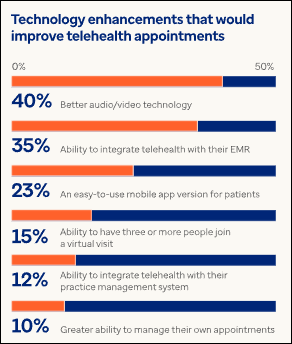
Behavioral health is the one inarguable success story of telehealth, where both patient preference and outcomes have been documented as well served. How does telehealth fit into the model you described?
It’s great. It’s the best thing that could have happened in the behavioral health space. It is removing those barriers of adoption, engagement, and access. However, it doesn’t fix the problem that a tele-therapist is still a finite resource. If I’m providing teletherapy, whether it’s over the phone, video, or in-person, I still can only see one patient at a time. I’m still a limited resource.
There’s still the question of getting the right people to the right level of care. Not everybody needs a tele-therapist. Some people would benefit from digital self-service tools alone, working on mindfulness and exercises. It’s still a matter of triaging effectively.
Telehealth services also don’t help with the identification of these issues in primary care or in other types of settings. While telehealth is an enormous step in the right direction, in terms of improving access and so forth, there’s still a huge component that it doesn’t address, which is the way that we think about behavioral health from a behavioral health integration lens as opposed to just the services.
What developments do you expect to be most important to the company and your niche in the next few years?
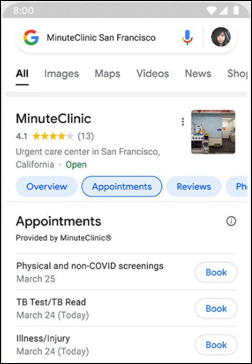
For the company, we think of ourselves as an augmentee to the providers. We are a clinical decision support engine, and to use a military term, we are a force multiplier to the system. We’re not competing with the therapy companies. Quite the contrary, we are helping get the right people to them. We’re investing a lot into open API structures, making interoperability easier with appointments and making that user experience more seamless from primary care to therapists and back to primary care. I think that will be a huge trend as we move forward in the industry.
In terms of the industry overall, the jury isn’t even out any more. The data is unequivocal that the impact of physical and mental health combined is astounding. I think you’ll see more value-based care contracts that are aligning the payers and the providers to provide holistic care to the patient, ultimately getting the patient better on both sides of the spectrum and making sure that we are reducing unnecessary utilization and improving costs, which I’m excited about.








































I can read them fine by clicking and dragging them larger. Tested on desktop, iPad, and iPhone. Not perfectly sharp,…