The Ascension incident shows the gap of the AHA statement indicting third parties. Hospital/healthcare organizations need to step up their…
EPtalk by Dr. Jayne 5/2/24
The hot topic in the virtual physician lounge this week was that another company has decided that delivering healthcare is more difficult than it thought.
Across the board, members of a primary care discussion group felt vindicated that Walmart plans to close all 51 of its Walmart Health centers as well as its Walmart Health Virtual Care telehealth offering, citing rising costs and “the challenging reimbursement environment.” These are the same struggles that physicians are facing, usually without any kind of corporate subsidy.
The health centers locations by state are Florida (23), Georgia (17), Texas (7), Arkansas (3), and Illinois (1). Non-provider associates are eligible to transfer to other Walmart or Sam’s Club locations, otherwise they’ll be paid for 90 days and then receive severance benefits. Providers will be paid “through their respective employers” for 90 days and then will receive transition payments. Walmart Health is an Epic client, making me curious as to what breaking that contract looks like.
I’m a fanatic about scheduling my next dental appointment before I leave my current appointment, so I was surprised recently when I started receiving reminder text messages that my appointment was due and I needed to schedule. I called the office and they confirmed that my appointment had disappeared from the system, but offered me the “recently opened spot” that was actually my original appointment. It turns out that they migrated their electronic dental record to a different system and apparently some appointments became casualties. I’ve done enough practice management system conversions in my career to know that sometimes things happen, but it sounds like they may not have had as rigorous of a QA plan as they needed since they said other appointments had disappeared as well.
On the Saturday morning prior to my appointment, I received a text message to fill out some forms. I was busy doing other things and didn’t do it, only remembering as I was in the car on the way to the appointment. I had some extra time in the parking lot and tried to fill them, out but discovered that the web app wasn’t really configured for a mobile device and the fonts were too small to read. I couldn’t figure out how to make the fonts any bigger, so gave up and went into the office. They tried to send me the text again to have me complete the forms on my phone. I explained the problem with the font size and they had no suggestions other than to hand me an old fashioned clipboard. They mentioned that “none of the information from the old system came into the new one,” which made my informaticist heart shudder.
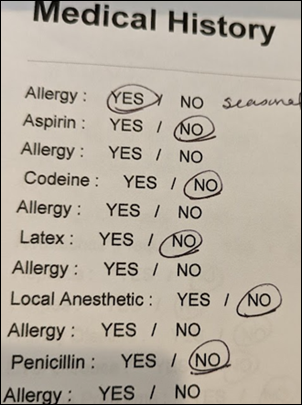
The paper forms were a sorry lot, with the first page having been printed without all the desired data elements on it, so someone had gone through and written “Emergency Contact Name and Number” blanks by hand. I zoomed through to the medical history form, and only after answering the first question did I realize that the format made no sense at all. I made my best interpretation at what they were wanting and handed back my clipboard as quickly as possible.
It’s embarrassing that professionals think these kinds of forms are OK. I secretly wanted to offer some clinical consulting services. I mentioned my confusion about the form to the dentist, who reassured me that my records had indeed been migrated into the new system, showing my chart on the in-room display. He said that he would follow up with the front desk to find out why they’re making people fill out a full history, so at least that’s something. I’m not sure who the vendor was on the electronic dental record, but if you work for one and are reading this, please check your mobile app to make sure it’s accessible to those of us who are experiencing the visual changes that come with age.
An ”Inside Story” feature in JAMA Internal Medicine tells the story of what resident physicians feel like when the EHR goes down unexpectedly. The resident describes an “unexpected fatal error to the system that the IT department was working to resolve.” There is no mention of a downtime solution, with the author stating that “samples for the morning laboratory tests could not be collected because the phlebotomy team did not know which patient needed which tests.”
The resident arrived at the “simple answer” of asking patients about their conditions and talking to the nurses who had most recently cared for them. They changed to a “minimum laboratory testing approach” after realizing that it was likely that patients had been undergoing tests that weren’t necessary, but rather were ordered simply as a result of order set use.
The author notes that “the EMR downtime made me realize that while the system seems to make our clinical routine convenient, it may not result in increased efficiency or better patient care.” Patients continue to receive daily labs that are part of an admission order set and those caring for them aren’t asking each day whether those orders are necessary or appropriate. They mention that “I look unprepared to my team when I do not know my patients’ latest basic metabolic panel and complete blood count values during rounds, but no one would ask me how much time I spent talking to my patients.” The author also enjoyed actually talking to members of the care team rather than communicating through the EHR, closing by saying that “our patient care on that day was the most patient-centered and most collaborative than ever in my 2 ½ years of residency.” Only one comment has been left on the piece so far, but I’ve got my popcorn and am sticking around.
It’s time to update those health maintenance settings in the EHR, now that the US Preventive Services Task Force (USPSTF) has issued an updated Recommendation Statement on breast cancer screening. Women aged 40 to 74 are recommended to have screening mammography every two years. The previous recommendation that was last updated in 2016 called for women to begin screening mammograms at age 50 and that women aged 40 to 49 should engage in individualized decision-making to determine a screening plan.
In a situation where we don’t have enough physicians who have the time to truly do health-related counseling during their visits, individualized decision-making can be problematic. Patients are reluctant to schedule a dedicated appointment to discuss screening, so it becomes one more thing that has to be crammed into a well woman or other preventive visit. I wonder how quickly people will be updating the recommendations in their EHRs and how organizations plan to educate physicians and care teams.
What is your organization’s plan to roll out the new USPSTF recommendation? Leave a comment or email me.

Email Dr. Jayne.


My dentist office switched to electronic forms a few years ago. The last time I filled out a paper form was when I joined their practice. Now I’m handed a table each time I visit (twice a year) and complete the same questions. The user interface is awful. Like you, I want to know if the staff are looking at this from a patient’s perspective. On the one hand, I know that choosing a specific software vendor for forms completion does not impact the dentist’s qualifications, ability to perform work, etc. But the choice of a forms vendor does make me question their judgement, which then makes me wonder if there are other dentists that would provide a better front-desk experience. I haven’t switched, and probably won’t because I love my hygienist, but these experiences really do matter. It’s hard to explain that well without sounding nitpick and over the top.
1) RE: EMR down & good staff collaboration. I believe it. Having worked at a now defunct EMR for 15+ years, we were so held hostage to government requirements—versus good clinical workflow. Period!
2) RE: Dental software… at least they’re trying. I get so annoyed by paper forms where I’m handed 6 forms and have to hand write my name, DOB and today’s date on them six times! Like the practice couldn’t take 5 seconds to staple together and just ask for that once? I’ll take the tablet/mobile option with small font! Ha!