News 3/22/24
Top News
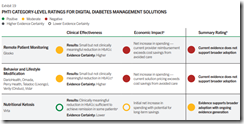
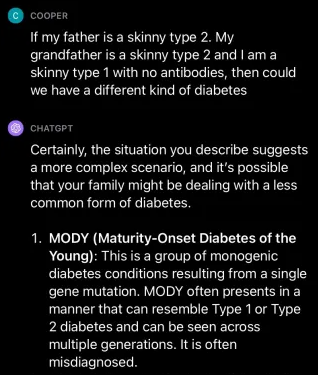
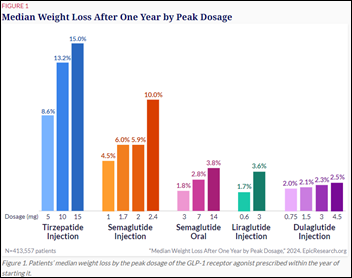
Digital diabetes management solutions increase healthcare spending without delivering meaningful clinical benefits, according to a review of evidence by the Peterson Health Technology Institute.
The study found that the tools facilitate small, clinically unimportant and sometimes temporary reductions in HbA1c that have little impact on overall health.
The report concludes that the solutions “increase net healthcare spending for purchasers because the small, estimated savings are less than the cost of the solution.”
The authors also note that the solutions require patients to record their self-management activities, which may not happen regularly.
Their advice for providers: “Because these digital health solutions complement (rather than substitute for) usual care, they represent an additional cost. Furthermore, these solutions can be labor intensive for provider practices to set-up and document for reimbursement, and effort from the provider and patient is required for implementation. As a result, providers should be cautious when considering the patient benefits weighed against the spending impact of these programs”
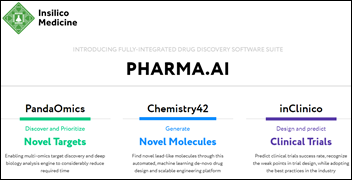
Click to enlarge the above graphic for a list of products in the categories reviewed.
Teladoc Health probably didn’t need this reminder that paying $18.5 billion for Livongo the fall of 2020 was unwise, especially now that the entire TDOC business is valued at just $2.5 billion.
Reader Comments
From CPAhole: “Re: disruption. What do you see as the next disruption in the delivery of health IT?” This technology CEO wasn’t optimistic about technology-goosed disruption in the rest of his email to me and neither am I. I don’t think you can disrupt technology without disrupting the delivery of health services, and I see little to suggest that the powers that be, including the elected ones, have an appetite to kill the golden goose. People leave HIMSS every year buzzed on their annual Kool-Aid top-off that technology will improve our embarrassing standing among developed nations in health, cost, and lack of insurance coverage. I could have expressed optimism about AI like most uninspired pundits, but I don’t see how whiz-bang diagnoses and point-of-care research findings help people who can’t afford treatments or even get appointments. Those of us who spend our days in the carpeted parts of healthcare are jarred by reality when we, or our family members, become patients who have to deal with the infuriating system that we created and that lines our pockets. Still, technology can make some inefficient and ineffective parts a bit better – just don’t expect technology to fuel consumer-level disruption or to power big moves of our societal health needle. I am now successfully vented like a time-expired Instant Pot, thank you, so it’s your turn to tell me what you think. What technology could disrupt or at least markedly improve health services delivery?
From No Cap (IYKYK): “Re: the quotes sent to Existential Dreadlocks about attending conferences. They are aren’t wrong. Conferences are a boondoggle, spurred by the FOMO inertia of company brass, salespeople, and marketers who want to be at the cool kids’ party. Thinking that the next $MM deal is there for the taking.” I’m picturing a “Self-Importance Summit,” where those industry gadabouts who are known for public displays of self-affection sit in their own booths, where they interview each other for podcasts, present each other with fake awards, and “network”at a never-ending happy hour by energetically exchanging business cards like jousting medieval knights.
HIStalk Announcements and Requests

Today I learned that you can send documents to Amazon’s Kindle reader app. An author sent me a PDF proof of their book, which I wanted to read on my IPad. I Googled and found Amazon’s Send to Kindle webpage, where you can send PDF and DOC files to your Kindle library and then read them pretty much like a normal Kindle book. You can also send files directly to the Kindle app on IOS and Android, export them to Kindle from Word, or email them directly to your Kindle account’s email address (who knew that it had one?) Amazon also provides a Chrome extension that can send full webpages to a user’s Kindle library. TL;DR – you can read most kinds of documents on your Kindle app or device.
Webinars
March 27 (Wednesday) 3 ET. “Houston Methodist: Deploying clinical AI at scale for improved outcomes.” Sponsor: Health Data Analytics Institute. Presenters: Khurram Nasir, MD, MPH, chief of cardiovascular disease prevention and wellness, Houston Methodist DeBakey Heart & Vascular Center; Brenda Campbell, RN, senior consultant, HM Health System Innovations; Nassib Chamoun, MS, founder and CEO, HDAI. The presenters will share how an interdisciplinary team collaborated to successfully use predictive models and a novel AI-driven approach to address post-discharge mortality. They will also describe how they expanded use of the platform to reduce clinician time spent digging through the EHR with a one-page risk profile, including codes extracted from notes using generative AI, and targeting their highest risk patients for extra attention. They will speak to how they overcame barriers to bringing AI at scale to support clinicians across the care continuum.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
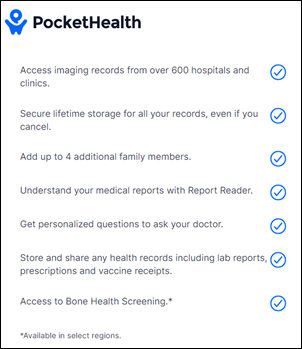
Pocket Health raises $33 million in Series B funding. The company offers a patient-centric, subscription-based image exchange platform that explains medical terms, detects follow-up recommendations, and suggests questions that the patient should ask their doctor.
CareCloud reports Q4 results: revenue down 13%, adjusted EPS $0.30 versus $0.25, beating earnings expectations but falling short on revenue. CCLD shares have lost 63% of their value in the past 12 months versus the S&P 500’s 27% rise, valuing the company at $20 million. The company said in the earnings call that it will implement a cost savings program and will introduce an ambient listening solution for visit documentation. It took a $42 million goodwill impairment charge in Q4 as a result of suspending the payment of dividends, resulting in FY2023 loss of $49 million.

Process automation vendor Syllable acquires Actium Health, whose system reviews EHR data to identify patients who may need specific medical services.
People



Optimum Healthcare IT founders Gene Scheurer and Jason Mabry return as CEO and president, respectively, and the company promotes Brian Symonds, MBA to chief digital officer and head of digital transformation.
Announcements and Implementations
Artera adds a referral service to its Harmony platform that automates outreach, appointment management and self-scheduling, and pre-visit communications.
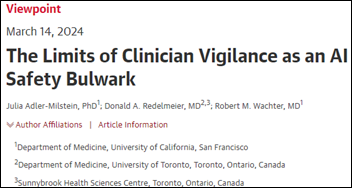
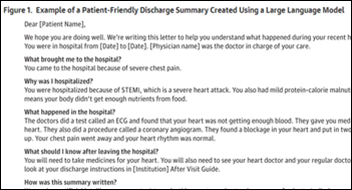
A study of Stanford Health Care’s use of AI to draft responses to patient message finds that clinician adoption was higher than expected and assessments of burden and burnout were improved, but EHR audit logs showed no time savings even though study participants perceived that the process was faster.
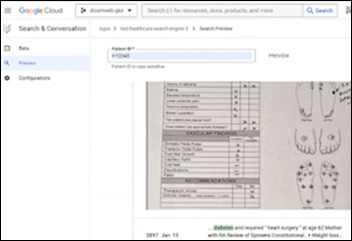
An Optum insider says that executives at its financially underperforming eastern division planned to order nurses to find old medical conditions in patient charts, whether they remained active or not, to support increased billing. The plan was for the nurse to add detail that would bring those issues back into the active problem list, and when the chart was next updated with a new visit, offshore coders would bill Medicare for the nurse-created codes without the physician’s knowledge.
Privacy and Security
A British privacy watchdog is investigating reports that at least one employee of the London Clinic tried to read the medical records of the Princess of Wales during her January stay for abdominal surgery.
New HHS guidance reiterates that covered entities can’t use web tracking technologies that might result in PHI disclosure, but clarifies that webpages that don’t require users to log in and that don’t have access to PHI don’t fall under HIPAA’s purview even if the user can be tied to an IP address.
Other

Someone used AI to generate this graphic that I saw on Linkedin. Which is most bizarre — the missing and deformed fingers, the oddly designed stethoscopes, the faceless watches, or the guy at the top who is either missing his right hand or using it to violate his female colleague?
Boston surgeons transplant a pig’s kidney into a patient. They didn’t mention how the pig is doing.
Sponsor Updates
- Wolters Kluwer Health publishes a new case study, “Cooper University Hospital of New Jersey achieves USP compliance success with Simplifi+.”
- FinThrive releases a new Healthcare Rethink Podcast, “Let’s Give Healthcare Consumers a Clean Slate!”
- Healthcare IT Leaders releases a new Leader to Leader Podcast, “Technology Planning for Future Growth.”
- InterSystems announces that, as part of the 2024 Best in KLAS Awards, its HealthShare Unified Care Record has been named the regional winner in the Shared Care Records/HIE category in Europe.
- Neuroflow releases a new podcast, “Neuroflow NLP Technology Surfaces Suicide Risk That Assessments Alone May Miss.”
Blog Posts
- Medical Billing Best Practices for Optimal Revenue in Urgent Care (Experity)
- Fixing Inefficient and Costly Prior Authorization: A Path to Modernization (FinThrive)
- How Cyber Attacks Impact Patient Trust (Fortified Health Security)
- Themes on the path to revolutionize clinical trials at SCOPE Summit 2024 (Inovalon)
- How EHRs Elevate Rural and Community Nurses (Medhost)
- Connection Fuels Interoperability at HIMSS24 (Meditech)
- Unlock New Telehealth and Remote Therapeutic Monitoring Opportunities in 2024 (Net Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…