Top News

The Defense Department appoints former Harris Corp. VP Barclay Butler to serve as director of the Defense Department/VA Department Interagency Program Office to manage the development of an integrated EHR for both departments.
Reader Comments
 From HairClub: “Re: Shafiq Rab. The CIO at Orange Regional Medical Center is taking the VP/CIO position at Hackensack University Medical Center.” Unverified.
From HairClub: “Re: Shafiq Rab. The CIO at Orange Regional Medical Center is taking the VP/CIO position at Hackensack University Medical Center.” Unverified.
 From Free Lunch: “Jason DeSantis. Joining Zanett’s healthcare division as executive director of business development.” Unverified. He’s division CIO at University Hospitals in Cleveland.
From Free Lunch: “Jason DeSantis. Joining Zanett’s healthcare division as executive director of business development.” Unverified. He’s division CIO at University Hospitals in Cleveland.
 From Last Man Standing: “Re: GE Healthcare. Layoff today of 5% targeting services and support.” Unverified. Many of the GEHC rumors I get are somewhat true but exaggerated, so if the company provides an update (which companies usually don’t for HR-related issues) I’ll run it here.
From Last Man Standing: “Re: GE Healthcare. Layoff today of 5% targeting services and support.” Unverified. Many of the GEHC rumors I get are somewhat true but exaggerated, so if the company provides an update (which companies usually don’t for HR-related issues) I’ll run it here.
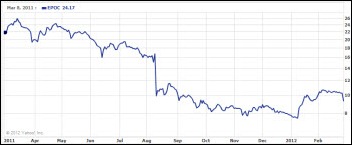
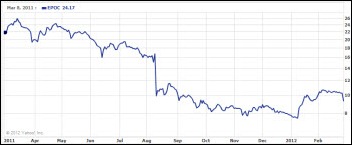
 From Printgeek: “Re: Epocrates. Laid off their entire EMR staff on Tuesday and are shutting down their EMR project. The BOD lost patience, as crazy sales expectations were set by previous CEO and CFO. They expected to sell 1,500 docs in 2011 with an uncertified system that was release in July. This exec team did a good job hiring talent, but failed to listen to their feedback on what it takes to actually sell EMR and the subsequent expectations.” I think there’s a lesson to be learned here: if selling EMRs was easy, everybody would be doing it, and HITECH has accelerated the polarization of the successful and unsuccessful vendors. If Epocrates, which has an impeccable brand recognition in healthcare and was seemingly doing all the right things, struggled to meet sales numbers for its EMRs, clearly the age of the mom-and-pop EMR is over. Actually, there’s an even more applicable lesson here: publicly traded companies may say all the right things about being dedicated to healthcare, but quarterly numbers can send them fleeing for cover almost instantly. Whatever docs just bought their EMR are now finding out what it means to be on the wrong side of their vendor’s “core business.” The one-year share price chart doesn’t inspire much confidence that a steady hand on the tiller is what’s needed – shares are down almost 60% in the past year.
From Printgeek: “Re: Epocrates. Laid off their entire EMR staff on Tuesday and are shutting down their EMR project. The BOD lost patience, as crazy sales expectations were set by previous CEO and CFO. They expected to sell 1,500 docs in 2011 with an uncertified system that was release in July. This exec team did a good job hiring talent, but failed to listen to their feedback on what it takes to actually sell EMR and the subsequent expectations.” I think there’s a lesson to be learned here: if selling EMRs was easy, everybody would be doing it, and HITECH has accelerated the polarization of the successful and unsuccessful vendors. If Epocrates, which has an impeccable brand recognition in healthcare and was seemingly doing all the right things, struggled to meet sales numbers for its EMRs, clearly the age of the mom-and-pop EMR is over. Actually, there’s an even more applicable lesson here: publicly traded companies may say all the right things about being dedicated to healthcare, but quarterly numbers can send them fleeing for cover almost instantly. Whatever docs just bought their EMR are now finding out what it means to be on the wrong side of their vendor’s “core business.” The one-year share price chart doesn’t inspire much confidence that a steady hand on the tiller is what’s needed – shares are down almost 60% in the past year.
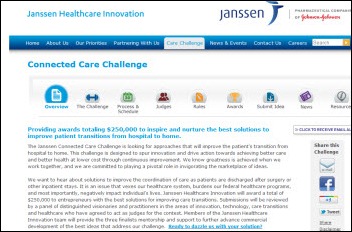
 From HIT Student: “Re: Connected Care Challenge. I thought some of your readers might be interested.” Janssen is offering $250K in awards for easily adopted, low cost technology solutions that can improve information sharing among hospitals, patients, caregivers, and community physicians, with the goal of improving post-hospital care and lowering the cost of unnecessary readmissions. Submissions are being accepted through March 25.
From HIT Student: “Re: Connected Care Challenge. I thought some of your readers might be interested.” Janssen is offering $250K in awards for easily adopted, low cost technology solutions that can improve information sharing among hospitals, patients, caregivers, and community physicians, with the goal of improving post-hospital care and lowering the cost of unnecessary readmissions. Submissions are being accepted through March 25.
 From Non-Sequitur: “Re: SNOMED. Here are examples of the proposal to require SNOMED in Stage 2/2014 Edition. In the 45 CFR Part 170 Standards Companion, see Pages 45 (cancer registry), 52 (problem list MU objective), 58 (summary care record MU objective), and 90 (lab results to public health agencies MU objective.)” Thanks. I know several readers are interested in the potential requirement to use SNOMED.
From Non-Sequitur: “Re: SNOMED. Here are examples of the proposal to require SNOMED in Stage 2/2014 Edition. In the 45 CFR Part 170 Standards Companion, see Pages 45 (cancer registry), 52 (problem list MU objective), 58 (summary care record MU objective), and 90 (lab results to public health agencies MU objective.)” Thanks. I know several readers are interested in the potential requirement to use SNOMED.

 From I Was There: “Re: HIStalk sponsor lunch at HIMSS. Great location, great food, a nice mix of heavy hitters and rising stars, and great networking with lots of cards being passed and commitments for follow-up discussions. Art Glasgow’s talk was very well received, talking about how HIStalk plays a part in his daily activities as Duke University Hospital CIO, how vendors and providers should help spread the word about it, and the shifts he made going from the vendor world at Ingenix to Duke. The focus was on the three of you as people were trying to figure out who you are and checking out Inga’s shoes. I thought the event was great.” It was really cool that 100+ folks from our sponsoring companies took time away from a very busy first day of the HIMSS conference to let us say thanks to them for supporting what we do. Naturally Inga, Dr. Jayne, and I felt simultaneously ridiculous and vulnerable appearing in disguise, but we did our best. Most of our sponsors understand that we’re going to objective and fair to sponsors and non-sponsors alike and, to their credit, they support us even when what we say isn’t going to be popular back in their offices. If you were there, thank you very much.
From I Was There: “Re: HIStalk sponsor lunch at HIMSS. Great location, great food, a nice mix of heavy hitters and rising stars, and great networking with lots of cards being passed and commitments for follow-up discussions. Art Glasgow’s talk was very well received, talking about how HIStalk plays a part in his daily activities as Duke University Hospital CIO, how vendors and providers should help spread the word about it, and the shifts he made going from the vendor world at Ingenix to Duke. The focus was on the three of you as people were trying to figure out who you are and checking out Inga’s shoes. I thought the event was great.” It was really cool that 100+ folks from our sponsoring companies took time away from a very busy first day of the HIMSS conference to let us say thanks to them for supporting what we do. Naturally Inga, Dr. Jayne, and I felt simultaneously ridiculous and vulnerable appearing in disguise, but we did our best. Most of our sponsors understand that we’re going to objective and fair to sponsors and non-sponsors alike and, to their credit, they support us even when what we say isn’t going to be popular back in their offices. If you were there, thank you very much.
 From Judy Judy Judy: “Re: Epic consulting firm. Last week Judy F. of Epic met with executives of [consulting firm name omitted] about their violation of Epic’s non-solicitation clause. An Epic client turned them in to Epic after the firm poached a handful of the client’s employees. Epic banned the firm for a year (which was ‘negotiated’ to a shorter term) from selling to or doing business with any new Epic customers. Seems like a slap on the wrist based on recent discussions with Epic Consulting relations personnel and their stringent expectations for consulting partners. Why not take away their preferred certification program as well?” Unverified, so I’ll leave out the company name for now.
From Judy Judy Judy: “Re: Epic consulting firm. Last week Judy F. of Epic met with executives of [consulting firm name omitted] about their violation of Epic’s non-solicitation clause. An Epic client turned them in to Epic after the firm poached a handful of the client’s employees. Epic banned the firm for a year (which was ‘negotiated’ to a shorter term) from selling to or doing business with any new Epic customers. Seems like a slap on the wrist based on recent discussions with Epic Consulting relations personnel and their stringent expectations for consulting partners. Why not take away their preferred certification program as well?” Unverified, so I’ll leave out the company name for now.
 From MD Informaticist: “Re: digital pen technology – mightier than the mouse? Are they really making an impact on usability and clinical documentation? I would be interested in your opinion of the Verizon and other digital pens and clarify for us: can this technology re-energize a dormant innovative industry?” What I’ve seen of them seems pretty cool, but I’m interested in hearing from readers about who is actually using them and what results they are getting.
From MD Informaticist: “Re: digital pen technology – mightier than the mouse? Are they really making an impact on usability and clinical documentation? I would be interested in your opinion of the Verizon and other digital pens and clarify for us: can this technology re-energize a dormant innovative industry?” What I’ve seen of them seems pretty cool, but I’m interested in hearing from readers about who is actually using them and what results they are getting.
 From Mark Schmidt: “Re: HIMSS. It’s become such a large event that the Booth Crawl brought back feelings of those early days when it was possible to spend time with just about every vendor. I learned a lot and heard the latest from Sunquest, which has not been sitting still as the industry has progressed!” Mark, CIO of SISU Medical Systems of Duluth, MN, won a Sunquest-provided iPad last week. He and I have swapped occasional e-mails going back to early 2008.
From Mark Schmidt: “Re: HIMSS. It’s become such a large event that the Booth Crawl brought back feelings of those early days when it was possible to spend time with just about every vendor. I learned a lot and heard the latest from Sunquest, which has not been sitting still as the industry has progressed!” Mark, CIO of SISU Medical Systems of Duluth, MN, won a Sunquest-provided iPad last week. He and I have swapped occasional e-mails going back to early 2008.
 From Just a Fan: “Re: 5010. Anyone else having issues with a claims clearinghouse not being ready? Our cash on hand is taking a beating because our claims have been sitting at the clearinghouse and are only just now starting to trickle out to payers, which are requesting information required on 4010 but deleted in 5010. And the enforcement delay was good why?” We keep hearing anonymous rumblings with no specific examples. Give us details and we’ll see what we can find out.
From Just a Fan: “Re: 5010. Anyone else having issues with a claims clearinghouse not being ready? Our cash on hand is taking a beating because our claims have been sitting at the clearinghouse and are only just now starting to trickle out to payers, which are requesting information required on 4010 but deleted in 5010. And the enforcement delay was good why?” We keep hearing anonymous rumblings with no specific examples. Give us details and we’ll see what we can find out.
HIStalk Announcements and Requests
 This week on HIStalk Practice: Dr. Gregg pulls a double shift in an an attempt to diffuse last week’s “mournful silence” on HIStalk Practice while I was busy drinking IngaTinis and walking my high heels off at HIMSS. Dr. Gregg missed HIMSS this year, but still offers some fun HIMSS musings. A proposed rule would require physicians to return improper Medicare payments within 60 days of notification and allow auditors to investigate 10 years of records. Most physicians believe EHR use is valuable for improving quality and managing patient care, but less convinced that EHR improves diagnosis accuracy or treatment planning. Black Book Rankings announces its ambulatory EHR vendor rankings. Athenahealth CEO Jonathan Bush likens his company to a “snippy kind of overconfident Chihuahua jumping up and trying to nip at the tails of the Dobermans.” By the way, we are conducting a reader survey on HIStalk Practice that is in addition to the HIStalk version; we’d love readers to take a moment to have a to provide input. Thanks for reading!
This week on HIStalk Practice: Dr. Gregg pulls a double shift in an an attempt to diffuse last week’s “mournful silence” on HIStalk Practice while I was busy drinking IngaTinis and walking my high heels off at HIMSS. Dr. Gregg missed HIMSS this year, but still offers some fun HIMSS musings. A proposed rule would require physicians to return improper Medicare payments within 60 days of notification and allow auditors to investigate 10 years of records. Most physicians believe EHR use is valuable for improving quality and managing patient care, but less convinced that EHR improves diagnosis accuracy or treatment planning. Black Book Rankings announces its ambulatory EHR vendor rankings. Athenahealth CEO Jonathan Bush likens his company to a “snippy kind of overconfident Chihuahua jumping up and trying to nip at the tails of the Dobermans.” By the way, we are conducting a reader survey on HIStalk Practice that is in addition to the HIStalk version; we’d love readers to take a moment to have a to provide input. Thanks for reading!

 I appreciate the support of Levi, Ray & Shoup (specifically LRS Output Management) for supporting HIStalk as a Platinum Sponsor. The company’s expertise is in document solutions for hospitals, so let’s use a typical Epic shop as an example. Maybe your big Epic print jobs fail; you need centralized capability to monitor and reprint jobs without re-running them on Epic; you are maxing out out your Windows print queues or the Windows print spooler; or you’d like to save print costs by allowing users to preview reports before printing and automatically route large reports to more economical printers. With the LRS solution, you gain centralized control, you can implement load balancing, you avoid installing multiple print drivers on each workstation, and you get rid of the unreliable science fair of printing solutions (UNIX to JetDirects, multiple printer types, a mix of Epic text and ERTF documents, etc.) and you can even require users to verify their identity before printing patient documents to an unattended printer. It doesn’t matter how cool Epic is if the tangible, patient-critical label or report it creates as an end product is hanging out there in the ozone because of a cobbled-together print solution that is far less enterprise grade than the system that drives it. One hospital with four FTEs handling printing issues cut back to just one after implementing LRS Output Management, which can handle anywhere from hundreds to thousands of printers. And while Epic is a good example, the solution works with any application (Lawson, SAP, etc.) Check out their case studies from Carilion, Hopkins, UVA, etc. Thanks to Levi, Ray & Shoup for supporting HIStalk.
I appreciate the support of Levi, Ray & Shoup (specifically LRS Output Management) for supporting HIStalk as a Platinum Sponsor. The company’s expertise is in document solutions for hospitals, so let’s use a typical Epic shop as an example. Maybe your big Epic print jobs fail; you need centralized capability to monitor and reprint jobs without re-running them on Epic; you are maxing out out your Windows print queues or the Windows print spooler; or you’d like to save print costs by allowing users to preview reports before printing and automatically route large reports to more economical printers. With the LRS solution, you gain centralized control, you can implement load balancing, you avoid installing multiple print drivers on each workstation, and you get rid of the unreliable science fair of printing solutions (UNIX to JetDirects, multiple printer types, a mix of Epic text and ERTF documents, etc.) and you can even require users to verify their identity before printing patient documents to an unattended printer. It doesn’t matter how cool Epic is if the tangible, patient-critical label or report it creates as an end product is hanging out there in the ozone because of a cobbled-together print solution that is far less enterprise grade than the system that drives it. One hospital with four FTEs handling printing issues cut back to just one after implementing LRS Output Management, which can handle anywhere from hundreds to thousands of printers. And while Epic is a good example, the solution works with any application (Lawson, SAP, etc.) Check out their case studies from Carilion, Hopkins, UVA, etc. Thanks to Levi, Ray & Shoup for supporting HIStalk.

 Liaison Healthcare Informatics is supporting HIStalk as a Platinum Sponsor. The Atlanta-based integration and data management company has over 9,000 customers all over the world, including more than 600 in healthcare. The company’s cloud-based data integration solutions provide a platform for the secure exchange of data among providers, payers, patients, and HIEs. Some of the pain points it addresses are HIPAA, HITECH, DEA Form 222, Safe Harbor qualification of encrypting PHI data at rest, electronic file transfers, and avoidance of data breaches. Its Liaison Protect solution makes sure you are securing your databases, integrating encryption, tokenization, key management, and logging. Its Liaison Exchange managed file transfer software suite allows cost-effective management of ever-increasing volumes of file transfer exchanges both inside and outside the organization. If you need to accelerate your HIE or ACO efforts, securely share patient information with other organizations, or gain control over risky and poorly monitored file transfers, give their offerings a look. Thanks to Liaison Healthcare Informatics for supporting HIStalk.
Liaison Healthcare Informatics is supporting HIStalk as a Platinum Sponsor. The Atlanta-based integration and data management company has over 9,000 customers all over the world, including more than 600 in healthcare. The company’s cloud-based data integration solutions provide a platform for the secure exchange of data among providers, payers, patients, and HIEs. Some of the pain points it addresses are HIPAA, HITECH, DEA Form 222, Safe Harbor qualification of encrypting PHI data at rest, electronic file transfers, and avoidance of data breaches. Its Liaison Protect solution makes sure you are securing your databases, integrating encryption, tokenization, key management, and logging. Its Liaison Exchange managed file transfer software suite allows cost-effective management of ever-increasing volumes of file transfer exchanges both inside and outside the organization. If you need to accelerate your HIE or ACO efforts, securely share patient information with other organizations, or gain control over risky and poorly monitored file transfers, give their offerings a look. Thanks to Liaison Healthcare Informatics for supporting HIStalk.
 Inga mentioned the reader survey — you have one last chance to provide input that we’ll use to plan the next year of HIStalk. Thanks. It really does help us given that we work largely in a vacuum and have to pick and choose our projects since we have limited time to get things done.
Inga mentioned the reader survey — you have one last chance to provide input that we’ll use to plan the next year of HIStalk. Thanks. It really does help us given that we work largely in a vacuum and have to pick and choose our projects since we have limited time to get things done.
 For our numbers-obsessed reader(s), we had a record-breaking 125,867 visits in February, along with 196,565 page views. The e-mail blasts go out to 7,935 subscribers, while Dann’s HIStalk Fan Club has 2,268 members (OK, I admit that we’re not entirely comfortable with the idea of having fans, but it’s slightly satisfying to reflect on that fact during our frequent bouts of feelings of inadequacy and lack of accomplishment.) You can move our emotionally needy needles by (a) subscribing to the updates; (b) connecting with us on Facebook, LinkedIn, and Twitter; (c) supporting the sponsors who support us by poring over their ads, clicking those of interest, checking out their Resource Center pages, use the Consulting RFI Blaster to quickly solicit consulting help; (d) sending us news, rumors, guest articles, or anything else that would interest your fellow readers; and (e) feeling the positive thoughts Inga, Dr. Jayne, and I are beaming your way for supporting what we do in whatever form that support takes, which means a lot to the ladies and me.
For our numbers-obsessed reader(s), we had a record-breaking 125,867 visits in February, along with 196,565 page views. The e-mail blasts go out to 7,935 subscribers, while Dann’s HIStalk Fan Club has 2,268 members (OK, I admit that we’re not entirely comfortable with the idea of having fans, but it’s slightly satisfying to reflect on that fact during our frequent bouts of feelings of inadequacy and lack of accomplishment.) You can move our emotionally needy needles by (a) subscribing to the updates; (b) connecting with us on Facebook, LinkedIn, and Twitter; (c) supporting the sponsors who support us by poring over their ads, clicking those of interest, checking out their Resource Center pages, use the Consulting RFI Blaster to quickly solicit consulting help; (d) sending us news, rumors, guest articles, or anything else that would interest your fellow readers; and (e) feeling the positive thoughts Inga, Dr. Jayne, and I are beaming your way for supporting what we do in whatever form that support takes, which means a lot to the ladies and me.
 A reader asked about WellStar’s ambulatory EMR project. I have the information, but agreed to sit on it for a few days. Stay tuned.
A reader asked about WellStar’s ambulatory EMR project. I have the information, but agreed to sit on it for a few days. Stay tuned.

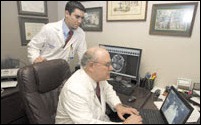
 The overachievers at API Healthcare, not content to simply mail Gabe Davis (right) of Texas Health Partners his iPad prize from the recent Booth Crawl after he had to leave the HIMSS conference early, sent VP Kyle Allain (left) to his office to hand-deliver “the famous HIStalk iPad” personally. This was Gabe’s first trip to HIMSS and he had nice things to say about HIStalk and API’s support of it. His 16-year-old son will get the iPad and is apparently pretty stoked about it, and rightfully so because iPads are darned cool even if you aren’t an Apple fanboy.
The overachievers at API Healthcare, not content to simply mail Gabe Davis (right) of Texas Health Partners his iPad prize from the recent Booth Crawl after he had to leave the HIMSS conference early, sent VP Kyle Allain (left) to his office to hand-deliver “the famous HIStalk iPad” personally. This was Gabe’s first trip to HIMSS and he had nice things to say about HIStalk and API’s support of it. His 16-year-old son will get the iPad and is apparently pretty stoked about it, and rightfully so because iPads are darned cool even if you aren’t an Apple fanboy.
On the Jobs Page: Financial Systems Consultants, Meditech CPOE Go-Live Support, Epic Certified Builders. On Healthcare IT Jobs: Senior Health Information Technology Specialist, Implementation Consultant, Project Manager CMIO Informatics, McKesson Paragon Consultants.
 I’m taking a little break to escort Mrs. HIStalk to somewhere warm and sunny where laptops are as rare as bathing suit tops (OK, I’m kidding on that one) so the eminently capable Inga and Dr. Jayne will be holding down the fort as I try to fight the urge to stay off e-mail (I’m rarely successful.) I don’t know about you, but I’m really tired after all the HIMSS-related activities over the past few weeks and I want to see what it feels like to sleep more than five hours in a single night.
I’m taking a little break to escort Mrs. HIStalk to somewhere warm and sunny where laptops are as rare as bathing suit tops (OK, I’m kidding on that one) so the eminently capable Inga and Dr. Jayne will be holding down the fort as I try to fight the urge to stay off e-mail (I’m rarely successful.) I don’t know about you, but I’m really tired after all the HIMSS-related activities over the past few weeks and I want to see what it feels like to sleep more than five hours in a single night.
Acquisitions, Funding, Business, and Stock
Teledermatology provider Iagnosis raises $1 million from 11 investors.

Accretive Health releases its Q4 numbers: profit of $13.2 million ($0.13/share) compared to last year’s $5.5 million ($0.06/share.) Net services revenue grew 53% to $260.1 million.
HP Enterprise Services notifies the State of Wisconsin that it will be eliminating 157 Medicaid program jobs in Madison and Milwaukee.
Sales
DR Systems announces six new contracts for its Unity platform totaling more than $2.07 million.

Cancer Treatment Centers of America signs an agreement to deploy Unibased Systems Architecture’s ForSite 2020 application suite across all its facilities.
People

Beacon Partners appoints Christina Bertsch (EMD Serono) VP of human resources.

The National Quality Forum board of directors announces that President and CEO Janet Corrigan will resign as of June 2012.

HHS Office for Civil Rights names attorney Juliet K. Choi (American Red Cross) as chief of staff and senior advisor.
Announcements and Implementations

Four Lakeland Healthcare (MI) hospitals go live on their $50 million Epic system.
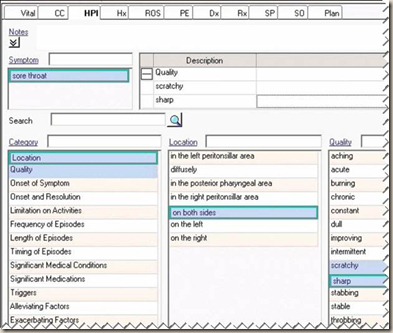
T-System licenses its clinical terminology to Prognosis HIS, allowing Prognosis to incorporate into its ChartAccess EHR more than 200,000 clinical phrases.
MED3OOO chooses Macadamian to help develop a new product that it says will expand the usability and adoption of its ambulatory systems.
Shareable Ink incorporates Pentaho Business Analytics to create a data analytics platform for healthcare.
Michigan Health Connect wins second place in an IT innovator awards contest for its electronic referrals solution app, powered by Medicity’s iNexx, that was rolled out to nearly 1,000 physicians over 28 counties.
Government and Politics
The Advisory Board Company does a nice high-level summary of the proposed Meaningful Use Stage 2, nice for CIOs prepping peer execs for what the IT agenda will look like.
In England, two NHS trusts seek a supplier to take over their IT help desk and infrastructure in what would be the first outsourcing contract of its kind. The deal is valued at $50 million.

 I liked Doug Fridsma’s post on HHS’s blog about the Interoperability Showcase at HIMSS. He says Farzad Mostashari showed up there by surprise and challenged the participants to demonstrate impromptu interoperability with another participant with whom no relationship existed. He gave them one hour to make it happen technically, which involved overcoming challenges such as authentication certificates, vocabularies, and firewalls. The result: NextGen sent a C32 to Allscripts, EXCITA HIE and Medical Informatics Engineering exchanged a transfer of care document in ER discharge summary format, and Enable Healthcare sent a CCDA discharge summary to Verison to create a new patient chart. That’s pretty cool.
I liked Doug Fridsma’s post on HHS’s blog about the Interoperability Showcase at HIMSS. He says Farzad Mostashari showed up there by surprise and challenged the participants to demonstrate impromptu interoperability with another participant with whom no relationship existed. He gave them one hour to make it happen technically, which involved overcoming challenges such as authentication certificates, vocabularies, and firewalls. The result: NextGen sent a C32 to Allscripts, EXCITA HIE and Medical Informatics Engineering exchanged a transfer of care document in ER discharge summary format, and Enable Healthcare sent a CCDA discharge summary to Verison to create a new patient chart. That’s pretty cool.
Other
Ochsner Health System (LA) announces that its neurologists recently completed their 1,000th patient consult as part of Ochsner’s telehealth stroke treatment program.
KLAS reports that some providers are concerned with a number product gaps and weaknesses in the McKesson Paragon product and wonder if Paragon can scale to larger hospitals, especially those with more than 400 beds.
Jackson Health System (FL) announces the layoff of more than 1,000 people in an effort to save the organization $69 million.
Trinity Health’s Michigan hospitals sign an agreement with University of Michigan to explore ways the organizations can work together to coordinate care, with one of the areas of discussion being information technology.

A physician’s assistant who sued her former employer, Mercy General Hospital (CA), for sexual harassment is awarded $167 million.

 The folks at MED3OOO asked Inga and me to choose and announce a winner from the six finalists in their contest to create the best video testimonial. They offered to pay for our time, but we said it either had to be (a) free to them because they’re a sponsor, or (b) if they really wanted, they could donate whatever amount they wanted to a charity of our choice. Thanks to MED3OOO for their donation to Best Friends Animal Society, a highly rated charity whose mission is “to bring about a time when there are no more homeless pets.” And congratulations to the winner, Kyle Adkins, administrator of Golden Valley Medical Clinics of Clinton, MO (he’s in Interview 1 on the finalist page) which implemented the InteGreat browser-based EHR from MED3OOO. My favorite quote: “You don’t ever make this decision well the second time or a third time. You may make a better one if you’ve made the wrong decision, but there will be someone else making the decision.” Great job, Kyle, and for that you win an all-expense paid trip to MED3OOO’s 2012 National Healthcare Leadership and Users Conference in St. Thomas, US Virgin Islands in October.
The folks at MED3OOO asked Inga and me to choose and announce a winner from the six finalists in their contest to create the best video testimonial. They offered to pay for our time, but we said it either had to be (a) free to them because they’re a sponsor, or (b) if they really wanted, they could donate whatever amount they wanted to a charity of our choice. Thanks to MED3OOO for their donation to Best Friends Animal Society, a highly rated charity whose mission is “to bring about a time when there are no more homeless pets.” And congratulations to the winner, Kyle Adkins, administrator of Golden Valley Medical Clinics of Clinton, MO (he’s in Interview 1 on the finalist page) which implemented the InteGreat browser-based EHR from MED3OOO. My favorite quote: “You don’t ever make this decision well the second time or a third time. You may make a better one if you’ve made the wrong decision, but there will be someone else making the decision.” Great job, Kyle, and for that you win an all-expense paid trip to MED3OOO’s 2012 National Healthcare Leadership and Users Conference in St. Thomas, US Virgin Islands in October.
Sponsor Updates

- World Wide Technology is sponsoring Geek Day 12 in Washington DC, April 11-12, complete with showcase labs, breakouts, and birds of a feather session divided by industry focus. The event is free and so is lunch.
- API Healthcare partners with Presagia Software to offer Presagia’s workforce absence management solutions to API clients.
- ProHealth Care (WI) goes live with iSirona’s connectivity technology to deliver patient data from anesthesia monitors into Epic EMR.
- A survey by BridgeHead Software finds that most hospitals want vendor neutrality with more control over their image data.
- Black Book names Quest Diagnostic’s Care360 EHR the best EHR for single physician practices and for e-prescribing. It was also ranked eighth on Capterra’s most popular EMRs.
- Alexander Orthopaedic Associates (FL) selects White Plume Technologies’ AccelaSMART resolution engine to bridge the gap between its Exscribe EHR and ADP’s AdvancedMD’s PM system.
- MEDSEEK and BrightWhistle partner to offer a search and social media marketing solution.
- Lawson Software enhances its Cloverleaf Secure Courier and Global Monitor for its Cloverleaf Integration Suite to increase speed and provide greater connectivity.
- New York-Presbyterian Hospital goes live with Awarepoint’s RTLS at its Columbia University Medical Center campus.
- Aventura will participate in the World Congress Inaugural eHealth Innovation Conference this month in Cambridge, MA.
- Santa Rosa Consulting advisor Matt Wimberley discusses confidentiality, integrity, and availability in the HIPAA security rule.
- Bruce Friedman MD, emeritus professor of pathology at University of Michigan Medical School, keynotes at the Lifepoint Informatics User Conference 2012.
- Evergreen Healthcare (WA) shares how API Healthcare’s Time and Attendance and Staffing and Scheduling technology helped the organization get its productivity and costs under control.
- MedAptus launches a revenue cycle reporting and performance analytics module for its Professional solution.
- Coastal Cardiovascular Consultants (NJ) will implement the SRS EHR at two locations for its six providers.
EPtalk by Dr. Jayne
The American Journal of Preventive Medicine recently published an article about cybercycling. It shows that riding a stationary bike which hooked up to interactive videogames could increase brain function in older adults compared with a standard exercise bike. Elderly study participants who took 3D tours and raced computer generated avatars showed better memory, attention, and problem-solving abilities. Not surprisingly, some reported knee and back pain as well as “frustration with interacting with a computer.” Now we just have to wait for a vendor to allow the cybercycling data to flow through the patient’s PHR into their EHR charts.
Shades of Eliot Ness: Even without federal approval, Illinois is getting tough on Medicaid fraud. The state will start matching Medicaid patient data with the state driver’s license database to make sure only Illinois residents are receiving benefits. Applicants would also have to show additional proof of income to maintain benefits. Even without federal blessing, this seems like a reasonable idea – recently 6% of Medicaid cards were returned as undeliverable or having an out-of-state forwarding address.
It looks like there might be another way for vendors to expand their offerings. The Department of Health and Human Services recently announced plans to look as far back as 10 years when auditing Medicare overpayments. I forsee a whole new subset of vendors offering data archiving and retrieval specifically for Medicare billing. As Medicare goes, so go the rest of the payers, so it’s only a matter of time before providers are forced to maintain massive amounts of data. And we thought seven years for the IRS was bad.
For those of you who work directly with providers, it will be interesting to see how upcoming changes to the Medical College Admission Test (MCAT) affect the physician pool. The test is being updated to gauge “knowledge of the psychological, social, and biological foundations of behavior” as well as critical thinking skills. The goal is to “better prepare students to be doctors in today’s changing health care system.” It will be interesting to see if this really makes a difference in patient care, but I do hope it will also make a difference in being able to intervene with colleagues who are ripping their hair out due to the continuous onslaught of ever-changing federal and payer regulations.
USA Today reports that Hawaiians rank at the top for residents having the best overall sense of well-being. Don’t attribute it all to the sunlight and tropical breezes though – North Dakota, Minnesota, and Alaska also made the top ten. West Virginia finished last. Gallup gathered the data by calling 1,000 people daily for all but 15 days of 2011.
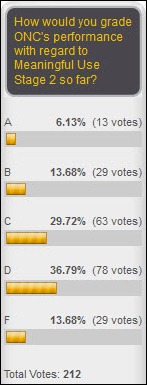
I’m still poring over all the Stage 2 documentation that’s coming across my desk (and phone, and e-mail, and the water cooler) and for better or worse, it seems like I’ve become comfortably numb as far as finding something noteworthy to discuss. Have a thought about your interpretation of those 455 pages of bliss? E-mail me.

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.































































































Thank you for your comments on Amazon. Agree 100%