Pamela Arora is VP/CIO of Children’s Medical Center of Dallas, TX.

Tell me about yourself and the medical center.
At Children’s, we’ve reached our 100-year anniversary, which certainly shows that Children’s Medical Center here is here to stay. Relative to the organization, we’re a not-for-profit. We’re the fifth-largest pediatric healthcare provider in the country. We have campuses in Dallas, Plano, and Southlake, which is around this Dallas-Fort Worth area. We also have 15 My Children’s pediatric practices. By the end of the year, we’re expecting that to be 17.
From a Children’s standpoint, not only do we have the hospital and the ED and we’re a Level One trauma center, but we’re also affiliated with UT Southwestern Medical Center. We have been working the hospital, the ambulatory setting, with over 50 subspecialties, and we have these primary care offices around the area here.
Relative to my background, I’ve been here at Children’s as CIO for approaching seven years. When I joined Children’s, it was just embarking on its Epic deployment. Prior to that, I was CIO at UMass Memorial in central Massachusetts in Worcester and have over the years worked in information technology — including some of Ross Perot’s companies, Perot Systems and EDS — working in a number of industries, including healthcare.
How is it different working in a children’s hospital instead of a general one?
From an electronic medical records standpoint, we really do have to look at weight-based much more extensively and from the standpoint of how the alerts work. It does have unique aspects that really affect the quality and safety of the children that we serve.
From a non-EMR standpoint, what I do say, which isn’t so professional, is that grumpy adults lead to grumpy adults, but kids, the pediatrics — they bring out the best in everybody. Really, I find that the folks here just love to adopt technology. It really is about making life better for kids. It helps people focus on, let’s say, the larger end game, just because with these children, they’re just amazing as far as how they’re working through their various conditions.
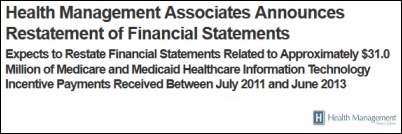
Someone from outside might say, gosh, you don’t have any Medicare to deal with.
We have a huge Medicaid base. We do have Medicare as well, but Medicaid is administered at the state level. That’s about 60 percent of our population. Relative to Medicare, we have that as well.
How did you choose Epic it and how do you view that project?
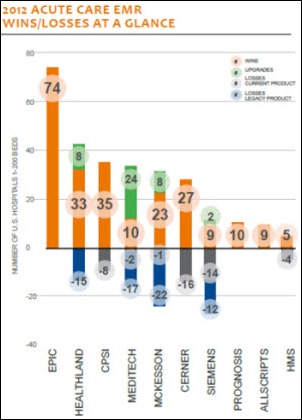
With Children’s, they’ve been a Cerner shop as far as hospital-based. We still have a footprint of Cerner within our back yard. But we’re for the most part Epic in a single instance. That has ended up being a good solution for us and we have a very strong ROI for our deployment.
Why switch from one EMR vendor to another? As context, our ambulatory clinics and our primary care office — at the time there was one – were on paper. When the organization was going to deploy an enterprise solution, a single instance across the entire organization, we stepped back, looked at it strategically, also took a look at our campus partners with UT Southwestern because we’re a teaching hospital and we certainly collaborate very well with Parkland, who’s also on this campus.
A strategic choice was made to go to Epic because our partners on the campus were also going to Epic. When you think of physicians that work in multiple environments, residents that may be working in Children’s as well as over at Parkland or one of the two hospitals with UT Southwestern, being able to be on the same EMR helps the care delivery.
In addition, our patients flow among the campuses. A baby might be born in Parkland and then end up being here at Children’s because they have broader needs. Sometimes from an ancillary standpoint we deliver services across the campus. Being on the same electronic medical record really helps.
We took it beyond that. We had cross-campus standards groups that clinicians engaged in to help us standardize how we deployed these three separate instances of Epic across our campus partner organization.
I’ve never heard of anybody collaborating with what could be considered your competitors. It’s interesting that for the benefit of physicians and patients, you’ve combined it into one big project.
We have, and I’ll give you more examples. We’ve even have a single program manager across all three campuses, select the same vendor product, kind of rework decisions along the way. We did that with our transplant solution.
From that vantage point, we’re looking at some solutions today around radiology, because in many cases, we’re running these tests for patients across the various campuses. It’s something that we do, and we’re expanding. I will also offer that we meet on a monthly basis, and when I describe the kind of collaboration across our campuses, many organizations that are in the same corporate entity cannot get that level of cooperation.
Now that you’re on Epic and having seen Cerner recently, what would you say are the best and the worst aspects of being live on Epic?
We have no regrets about being on Epic at all. I’m going to give you just a quick sense of how we rolled out, because comparing Cerner to Epic in some ways is apples and oranges because we are using Epic differently.
I think Cerner has a good product suite as well, honestly. We think that they have a great lab system. Epic’s has improved dramatically, too. But as far as working through it, when we first embarked on the Epic journey, we had Epic in the hospital, but the doctors weren’t documenting on the system. There was no CPOE. Our ED was still on paper, Ambulatory was on paper, those 55 different subspecialties. That one primary care office we had — that was on paper, too.
We went live with the first phase of Epic in October 2008. We took in scheduling, registration, and hospital billing. Phase 2, about a year later in November 2009, is when we got into the clinical documentation, bar code med administration, CPOE. Phase 3 was when we upgraded and we started to get into the subspecialties. But when you take a look at the doctors, it really became in Phase 2 that they got much more engaged.
If you take a look at how we digitized, we have eliminated paper. We’re a HIMSS Level 7 organization. From the standpoint of that journey, the contract was in early 2007 and even now we’re doing different components of rolling out Epic. We’re very happy with the Epic solution. No regrets.
As far as Cerner, we have been over the years a development partner with them, and bar code meds, we’ve been one of the first organizations. We’ve had, I think, four different solutions in here. Since I’ve been here, it was a Cerner solution and then we helped Epic as far as refining their solution. The nursing and the folks that had been using Cerner before – they came into using Epic with a point of view.
There were some things that allow navigation that we needed to refine after we went live with Epic. At first the nurses in particular found it hard to follow the way the flow of documentation works within Epic. But truth be known, Epic is very flexible. They work with their customers. They’ve been very responsive.
Cerner, we’ve continued to be impressed with some of the innovations they’re doing around their lab solution. But because we’re trying to move to seamless, we keep working with our lab organization here, our lab department, to see at what point we can take them over to Beaker. Ultimately our aim is to deploy Epic enterprise-wide vanilla, and it has been deployed enterprise wide. But when you take a look at radiology, we still have iSite and we have Cerner for lab. There’s different boutique solutions we have out there.
What recent projects, excluding Epic, are you the proudest of?
Here in Texas, we’re just going onto prospective payment.That occurred in September of this year. As far as deploying that solution, as our organization is going through and seeing how that impacts our organization, there’s a lot of awareness that needs to be built with the clinical folks on how their documentation translates into how prospective payment informs reimbursement. From that vantage point, we’ve had a very helpful deployment. We’ve plugged in some 3M tools. The partnership between the HIM, the IT organization, and the clinicians as far as going through that transition … I’m incredibly proud of the accomplishments even at this early stage of the go-live of prospective payment in our state.
In addition, we looked at it as a broader clinical documentation improvement program. I would say that a lot of the work that needs to be done for ICD-10, we’re at a state of readiness because we were working a lot of those components simultaneously, even though the date for ICD-10 was pushed out. I’m very proud of the accomplishments there.
We recently went live with a telemedicine solution for our NICU. Given that our organization handles the most of fragile of patients, and we have the highly specialized clinicians in our environment; we’re trying to figure out how to help the community broadly and allow children, especially when they’re in that fragile state, help them be able to stay in their community and only be flown in phone in or helicoptered in when they absolutely need to be. We have a partnership with Trinity Mother Frances. We’re deploying our talent with our NICU via telemedicine into that community hospital. In doing so, we’re finding opportunity to turn around the care of a patient within their environment.
When you talk about how pediatrics is different from adult care, the clinicians certainly see that there’s a difference between delivering care to a child versus an adult. In many cases, if you’re in a community hospital, you get concerned on whether you can deliver the right care for that child. Many cases, they’ll transport the child to us just because they’re not certain. By having telemedicine in the mix, we’re in a position to be able to give them that support that they need in their location, which ultimately leads to not only lower-cost care, but higher quality. When you talk about transporting a child when they’re in that fragile state, it impacts their health as well.
As far as that particular accomplishment, we’re getting such positive response on leveraging our capabilities around the NICU that we’re finding a number of locations across Dallas-Fort Worth that are interested in an organization that can help them in that manner. We are somewhat unique in that we’re the first pediatric hospital in Texas to achieve Level One trauma status and we’re the only pediatric facility that’s associated with UT Southwestern Medical Center.
What technologies have you planned or implemented that will empower the families of your patients?
We have several areas where we’re helping families. We have what we call the Children’s Online Experience. It’s a portal into our electronic medical record so that they can get information on tests and be able to see about appointments. In addition, we have very specialized portals based on the disease population. For example, if I’m an endocrine patient and let’s say I’m 10 years old, I might be wanting to converse with other patients that are like me in a support group way. We provide social networking capabilities in that regard as well as education on the portals.
I will also talk about one other initiative that we’ve worked with the OCR, and that’s our personal health record. While we leverage Lucy, which is part of Epic, some of this is consumer-based on whether they’re demanding or they’re interested or even asking or aware of what a personal health record is. We’ve been committed since I’ve arrived here at Children’s to support whatever platforms the patient families are interested in leveraging in that vein. But we haven’t seen it take off very rapidly.
The OCR felt similarly. They have a grant program called Ignite. They recently shot a video about some of the work that we’ve done with their Ignite program. It was a grant-funded program that we engaged in. We were the first in the nation to use the PHR where we take records from Epic and push them out to Microsoft HealthVault. Verizon was good enough to donate handheld iPhones for our patient families that could help with sickle cell patients in Tyler, Texas. This is our initial case, and we have a number of instances across the organization, Children’s, that are interested in doing like-type solutions.
In a nutshell, we push out the record directly into Microsoft HealthVault and then the patient family gets medication alerts for these sickle cell patients, because if they don’t take their medicine in a timely way, it’s very painful. That condition is such that if you don’t take it on a regular basis, it’s very painful. Through the mechanism of using the PHR, we’re using the medication alerts on these mobile phones. But on top of that, that patient and that family has their PHR information that’s theirs to leverage at all these different locations that they may get care delivered to them. In the case of Tyler, many of these patients, to travel to Dallas-Fort Worth. That’s a long distance.
We’re finding that we’re doing a better job managing their conditions directly. It’s a slightly different model, but very similar to what we’re talking about with telemedicine. How do you get the care delivered to the location of where the patient family is, whether it happens to be in a community hospital, or happens to be on their handheld in a school?
There’s one other thing I’m going to mention relative to telemedicine. We’re also doing telemedicine with schools. It’s a much more sophisticated set of instruments for the NICU, but if you think of a little metal travel bag that someone might take on an airplane, about that size. It’s filled with medical equipment. A Children’s nurse goes into the school system and they’re able to deliver care to the patient in the school. At that point, not only is it helping the patient, it’s helping the families in some cases because it is a bit of a struggle when the child gets that earache in the middle of the day, and invariably when the parent comes home, they find it hard to find services.
In this case, we’re able to help the patients right in the school system and be able to leverage our primary care offices across the community to be able to deliver care without the child leaving the school and the physician can deliver care from one of our primary care offices. That’s another area where we’re reaching out into the community.
Comments Off on HIStalk Interviews Pamela Arora, CIO, Children’s Medical Center
















































Re: Dr Z. Great story, but whatever happened to professional courtesy???