Farzad Mostashari, MD, MSc is CEO of Aledade of Bethesda, MD.

How do you pronounce the company’s name? Is it Allay-DODD?
Allay-DADE.
Explain the company’s business model and what Venrock’s interest is in backing it with a significant investment.
The business model is pretty simple, actually. We’re going to give physicians – independent primary care practices – pretty much everything they need in order to form and join an ACO. The key business model for an ACO in this case is that the main revenue source for us comes if and when we generate total healthcare spending reduction and improvement in total healthcare quality and coordination.
This is all predicated on our belief that with the right tools, with the right technology, with the right boots on the ground, with the right team, with the right primary care providers, we can go right at the heart of what’s ailing healthcare today and get to better care, better health, and lower cost. If we can do that, the company prospers and the primary care docs prosper.
Who actually writes you checks and how do you calculate that savings that I assume you’re getting a percentage of?
There is an organization, an accountable care organization, which we will stand up. That entity then enters into contracts with health plans. The contracts with the health plans basically say, “You have a projected total cost for this panel of 5,000 or 10,000 patients. If we come in below that benchmark, the health plan gets half and the ACO gets half.” The largest plan in the world, Medicare, now has this available for primary care providers throughout the country. Many other health plans are following suit.
If I’m a physician and I decide I want to get in on this ACO thing, who are my fellow members or should I even know or care?
Healthcare is very local. We believe that you need boots on the ground, like the Regional Extension Centers in a way, harking back to that. Or even before that, to my experience with Mat Kendall, my co-founder, when we were in New York City. We went to 233 independent practices and we enrolled them in the Primary Care Information Project. This is similar, where in a given geography, we get a field team out, we find the right practices, and we bring them together, oftentimes with practices in a group they haven’t worked with before.
But really the work is done one-on-one with the practice. There’s a common set of tools — referral management tools, patient management tools, and risk management tools — but the real work happens in an individual, given practice, with the team going into the field.
What we’re looking for isn’t really networks of docs that have already come together. We’re looking for the independent, individual practices who might have thought, gee, I really want to get into this, but I’m just one practice — I only have a few hundred patients. They can’t by themselves enter into these risk arrangements. They need to be part of a bigger group. We’d be aggregating them with other docs who could form the core of this new high-value network.
That’s part of the value proposition we offer. It’s not that we’ll sell to anyone or work with anyone. A big part of this is the filtering out to make sure the people — the people you’re in the boat with — are really the people you want to be in the boat with.
What’s the risk to the practice?
Risk is something we have to manage. One risk is that it turns out there’s someone in the boat who’s not pulling their weight. Part of what we have and part of what Medicare requires is some incentives within the ACO that say, “We’re not just going to divide up the shared savings totally equally.” How much your participate in the ACO makes a difference in how much of a share you get. How do you on the key performance indicators determines how much of a share you get. In extreme cases, if someone’s really not doing anything, you can be expelled from the ACO. You can be voted off the island. That’s one risk.
I spent nine months at Brookings becoming a little bit of a student of ACOs that have succeeded and those that haven’t. One of the risks is if you don’t understand the regulations and their implications. This is one where being someone who’s been a regulator before and who understands how the regulators think is pretty helpful — to be able to reduce that risk for them. To say that I understand and our team has an in-depth understanding of what the regulations say and also what the implications of them are so you avoid some of the gotchas that have gotten people before.
I assume the doctor’s entire panel doesn’t just go ACO — there’s some blend of insurance patients and then adding new patients and converting some patients.
Exactly. This is perfect because it helps you transition.
It’s really hard to be going from one day doing fee-for-service regular practice and the other day to be taking full cap risk as part of Medicare Advantage. That’s not really feasible. There’s no health plan in the world that’s going to just turn over full risk contracts to you if you haven’t had the experience with this.
This is an ideal transition path for practices who know that’s the direction they’re in, that the future is value-based purchasing and being able to take accountability for total risk. This is training wheels, one-sided risk from CMS for three years. I’d love to go to a casino that gives me one-sided risk. [laughs].
In this model, if you get savings over the threshold, you share it with CMS. If costs go up, you don’t have to pay CMS the difference. It’s a really perfect opportunity for them to begin to gain the skills, gain the competencies, gain the tools, and then ramp up the risk. Ramp up with the number of different health plans that are participating. Expand to other commercial plans — as I said, more and more are going to be willing to give you these sorts of deals if you’ve proven your ability to manage risk. Then ramp up in terms of the kinds of risk you accept.
Initially, maybe you start off with one-sided risk. Then in three years, if you’ve done a good job with that, then you can feel more confident to move to two-sided risk or even delegated capitation agreements, where you get paid upfront for managing the total cost.
You mentioned the boots on the ground approach. Is this tied in any way to the Regional Extension Centers?
Well, you know, I have been a huge fan of the work of the Extension Centers. I’ve been saying for some time that the future for those Extension Centers is going to be in providing not health IT help, but actually getting into practice transformation. There’s not the funding available from the federal government for them to expand in a major way and to have a sustainability for those Extension Centers.
But you know, this could be a set of services that they could contract with us or anyone else to provide. This could be part of the sustainability model for Extension Centers moving forward if those Extension Centers have demonstrated their value to the providers and have the ability to move beyond just health IT to true practice transformation.
Assuming you work with the RECs in some capacity, who do you employ within the company?
There’s a set of central resources that you need that you don’t want to duplicate for every ACO — for every ACO to have their own legal team and have their own regulatory review and have their own IT team.
One of the things I’ve realized is once you are doing this ACO work, I can’t tell you the number of IT companies who assure me that they have the solution for me. [laughs] I’m the former National Coordinator for Health IT. I’ve seen a few products in my day. I have a sense and my chief technology officer Edwin Miller has been involved with some 30 different products. We have the ability to weed through and find out what makes sense to buy, what makes sense to build, and how do you assemble this all into one integrated technology platform. For a small ACO to do that, that’s just prohibitive.
I’ve talked to many ACOs who a year into it say, “We haven’t done anything because we’d have to start all over with our IT vendor.” That’s part of the central support that they get — the integrated technology platform, the data, the analytics, the regulatory, the legal, protocols, all that stuff. Then that’s partnered with the boots on the ground, which are local to them. A medical director who’s dedicated to them. A nurse coordinator. The project managers and transformation staff who go into the practice. The best of both worlds.
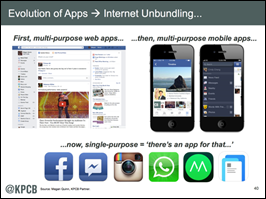
You mentioned EHR optimization and the integrated data and technology platform. Do you anticipate working with the EHRs each practice runs or will you have a relationship with vendors that will become the standard for the ACO?
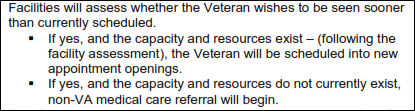
Step one is I’m going to pre-select the practices based on their ability to demonstrate Meaningful Use. For me, Meaningful Use is, “You’ve got to be this tall to ride.” Because without that, you don’t have the data to be able to make all this work.
Two, you and I know well that the EHR systems are not optimized, particularly for population health. We’re not going to rip and replace people’s EHRs, but we’re going to optimize the hell out of them. Make sure that the efficiency is there, that the workflows make sense, that the work of documentation doesn’t all fall on the poor doc. That you actually make use of the data you’re collecting. That their decision supports are meaningful and tied to the quality measures they’re trying to accomplish. That the registry functions actually work as intended.
Our team will have something of an advantage having not just implemented the certification and Meaningful Use qualities, but having actually built, with Edwin, three cloud-based EHRs that met the Meaningful Use requirements. So step one, make sure that they have the basic foundation.
Step two, optimize the heck out of them. Step three, bring to bear the tools that EHRs aren’t really built for. I wrote about this after HIMSS last year. There are too many people selling shrink-wrapped population health — reporting, really, not management — tools that are trying to automate stuff when we’re in the discovery stage. I think the first infrastructure we really need is a discovery set of tools, where you have a very flexible data architecture underneath with some very flexible data analytics tools on top. Then you figure out what it is after you do discovery. Then you create protocols. Then you move to automation.
We’ll look at what’s available right now in terms of both the fundamental underlying data architecture, the middleware tools that are needed, the analytic tools that ride on top, and then some frameworks for being able to create custom visualization into that framework. As I’m describing it, I’m sure you are seeing the flavor of what we’re building is not monolithic software platforms or enterprise pieces of software. It’s really more of a platform that becomes a chassis with separation between the logical layers.
There are a lot of certified products, so in a given group of practitioners that might want to be part of an ACO, you might have 10 or 15 EHR systems. How can you optimize those systems not knowing them first-hand like the users of those systems do?
I think we’re going to need to probably develop and hire and add to the team people who are experienced and experts in each of probably the top half a dozen, maybe eight EHRs, that will probably account for the bulk of our practices we want to work with. That’s one.
Two is to work with the vendors. This is one of the advantages that I’ll have. I’ll continue to take a vendor-neutral approach on the EHR side, which is more comfortable to me, and I’m sure there will be some that see the opportunity to work with us and will be able to learn from us even as we are working with them to optimize their solutions for the practices.
The EHR vendors need to learn how to optimize their own systems for population health management. There will be no one better to work with than us in terms of figuring out what that means.
You’ll be supporting some number of the more popular EHRs and then building the data layer that’s aggregated across all members of the ACO and you’ll provide analytics and population health management tools to sit on top of that?
Correct.
From the physician’s standpoint, you’re handling the administrative overhead. They’re just using the EHR they’ve always used and it’s somewhat invisible to them other than optimization changes or changes to meet quality standards. You’ll report back to them from the centralized version of their data collected with everyone else’s.
That’s right. Same EHR, just better. [laughs]
Hospitals and even practices are hearing “ACO” and are writing checks having no idea what they need or want. Will people get burned trying to jump too early on what they think the future will be?
I think this is a key risk for for ACOs — jumping on with the wrong technology and the wrong technology platform. Assuming that there’s going to be some magical ACO technology that’s going to solve your problem. This is still very much about discovery before we get to automation.
What have we learned about ACOs since the arguably mixed success of the Pioneer group? Can ACOs work everywhere and not just in areas where Medicare is paying too much?
Great question. I think my team at Brookings was the first to actually identify the individual 29 who had gotten shared savings and then start to look at the predictors and correlates of that.
What we found was that, one, it had been assumed that the Pioneer-type ACOs, the big integrated delivery networks, were going to blow the small physician-led ACOs out of the water. That was not true. Thirty percent of the physician-led ACOs demonstrated savings in Year One versus 20 percent of the hospital-sponsored ones. That’s a really interesting observation.
The second observation that I’ve had in a more qualitative than quantitative way has been that among a lot of ACOs that didn’t succeed, there were three factors and one underlying issue. The one factor was that they didn’t understand the regulations. The second factor was that they didn’t use data. They didn’t use data, they sat on the data, this treasure in the form of the claims data of every client paid by CMS, they just sat on it. They didn’t do enough with it. The third thing was that they didn’t change practice enough. They had monthly meetings and that was kind of it. If you do that, it’s too hard. You’re not going to generate savings.
I think those three factors are going to be more important than where you are. It’s can you use data? Have you invested enough, both in terms of your time and in money, in changing what you do? Third, do you understand the regulations? That’s what I’m bringing to the practices.
What you still need — and no one can hand it to you — is will. The will to change. That’s what we have to select for.
Hospitals I’ve worked in were swimming in data but didn’t act on it because there wasn’t enough imperative. Do we have enough data to move to a value-based payment model? Do you think the economic pressure will be enough to get people to pay attention?
I do. I do. Particularly for the smaller primary care practices.
With the hospitals, it’s more complicated. A, they have tons of competing demands. Forget about academic medical centers who have the teaching mission and the research mission and all of that mixed in. Even in just the tertiary care setting you have all these entrenched structures that reflect the fee-for-service optimization world.
For the hospital, life begins with the emergency room admission. Now you’re asking them to think about how to prevent an admission. That is totally foreign to a hospital and totally schizophrenic in terms of their revenue, where on the one hand they’re trying to reduce admissions, but on the other hand that’s their revenue and their bread and butter — heads in beds.
With a physician — and particularly a primary care-led ACO — it’s much easier. One, you don’t have tons of committees [laughs] to navigate through. It’s a small practice. The doc gets together with the office manager and their nurse and they say we’ll do this, and they do it, and it happens. I’ve seen time and time again in trying to make changes that it’s easier in the smaller practices than in the larger institutions.
Two, the incentives are much more meaningful to the primary care doc who is making $150,000 a year. That’s their take-home pay — $150,000 a year on average. For them, saying you could make an extra $50,000 or $100,000 – that’s really meaningful. That’s game-changing for them, whereas for a hospital to get back half of the revenue that they lost, that’s not really a game-changer.
How do you see small practices being configured differently with primary care docs getting squeezed by mid-levels and then operating under an ACO model?
We’re not going to try to totally upend the practice. We’re going to start with pretty simple stuff. Is there going to be someone to answer the phone at 9:00 at night when the patient calls or is there an answering service that says to go to the emergency room? That’s not totally upending the practice structure, exactly.
I think in the ultimate manifestation of really optimizing for value, what I suspect we’re going to see is primary care providers using referrals as consults. Neil Calman at the ACO Summit talked about how when as a group of family medicine docs they took over a practice that had tons of specialists in it – 10 orthopods and a hematologist or whatever – and they looked at what the patients were coming in for, they realized this is family medicine stuff. They were managing people with stable anemias. They were managing people with stable seizure disorders.
Use specialists as consultants, not to manage patients with stable conditions. That’s an example of disruption, where the primary car doc starts to do more of the work and not just refer patients reflexively to this specialist for this and that specialist for that and a third specialist for that and a fourth specialist for that.
Their job, frankly, is going to become a lot more interesting. That lets them shed some of the boring stuff that pays the bills today – the strep throat, the poison ivy. Let the mid-levels do that. Heck, let the urgent care center do that. Let CVS do that. Focus on what the highest value work is that each part of the healthcare system can provide.
Where do you hope the company is in two or three years?
For me, I want to have the most successful ACO in the country. [laughs] That to me is success, where we’re the best. We’re the best. We figure out how to use data and technology to bring the focus on the outcomes.
Gosh, I just can’t wait to tear into the meat of what we’ve needed to do, which is about the outcomes. It’s about being able to focus on how do we get measurably better health, measurably better patient experience, and lower cost. And use data and technology in really fundamental ways to accomplish that, but to have our eyes on the prize instead of structures and processes and so forth.
Do you have any final thoughts?
It’s an exciting time. This is in some ways a strange turn for me to do a startup and join the ranks on the private sector side. But in other ways, it just feels incredibly familiar to me. [laughs]
Let’s start with a blank piece of paper. Let’s think about what the world needs and build a team, build an awesome team, that can use data to improve population health. In a way, I feel like I’ve been in training for this all my life.




















































"A valid concern..." Oh please. Everyone picks the software they like and the origin of that software is an afterthought.…