News 6/18/14
Top News

Nuance is reported to be discussing a sale of the company to Samsung, with shares rising nearly 10 percent Monday and a bit more on Tuesday on the rumor. One might speculate that the recent addition of two of Carl Icahn’s people on Nuance’s board may have heightened the money-losing company’s interest in finding a buyer. Samsung already uses Nuance’s voice technology in its devices (as does its arch nemesis Apple, for which Nuance provides Siri), but would probably have little interest in Nuance’s considerable healthcare businesses that includes Dragon speech recognition, transcription, clinical documentation and coding, and image sharing. Highly paid Nuance CEO Paul Ricci ($78 million compensation in three years and shares worth $60 million) swelled Nuance with a bunch of acquisitions in two main sectors (healthcare and mobile) and has declined to focus its corporate strategy despite lackluster results, while Icahn likes selling off individual parts to create shareholder value. It will be interesting to see whether cash-rich Apple will be threatened enough by the rumored Samsung interest to make overtures of its own for the $6 billion market cap Nuance or perhaps part of it if Nuance is willing to break it up.
From Joe: “Re: rumored Nuance acquisition talks. Ironically Domino’s announced its Nuance-powered ‘order your pizza by voice’ app today. There’s probably a ‘Pete’s a delivery boy’ misrecognition joke in there somewhere.” Domino’s, which like Walgreens and other retailers is making technology an integral part of its product, says that typing characters is becoming obsolete and its app (which features order-taker “Dom”) will differentiate it from competitors. It’s refreshing to see how non-healthcare companies use technology to improve their business and customer experience given obvious, non-government mandated incentives (i.e., profit) to do so.

From KayCee: “Re: Epic. I asked Epic about whether their name should be capitalized.” KayCee inquired of Epic, “Only Mr. HIStalk seems to be defending the position that an all-caps reference reflects ignorance” and asked the company’s position. Epic’s response from spokesperson Shawn, who said the email was forwarded to him because, “We don’t have a marketing department,” states “EPIC” was used in an old version of the logo, but that was changed in the late 1990s and “Epic” is correct. I enjoyed Shawn’s erudite conclusion, which is more tolerant than mine: “Without judging whether it represents ignorance or an historical homage to our early years, we’re pretty forgiving and accepting of the misuse.” I will stubbornly point out that Shawn said that writing EPIC constitutes “misuse.”
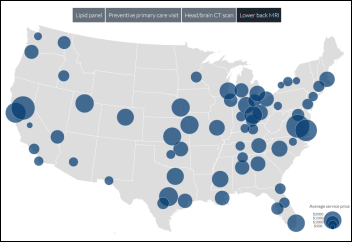
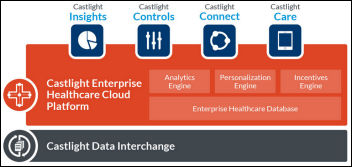
From Art Vandelay: “Re: Walmart opening clinics. The mind begins to work when combining this with information from Castlight Health: there is no state exchange or ‘caid expansion, Austin, TX has very expensive office visits but isn’t representative of the state, Walmart enters with a low-cost alternative. Most large health systems aren’t worried about retailers like Walmart, CVS, and Walgreens entering the market. It is less about primary care and more about interrupting their ecosystems for chronic care management – how will the data come back, will they use similar protocols, will patient education materials and the plan of care align.” Walmart will open its second and third company-owned clinics in Texas, expecting to expand that to a dozen this year in a pilot project. They will offer primary care services for $40 and will treat insured Walmart employees for just $4, but they won’t take private insurance, only Medicare and Medicaid down the road. The clinics will be staffed by nurse practitioners and managed by workplace clinical operator QuadMed.
HIStalk Announcements and Requests
Lorre has a lot of webinars going on and could use more CIO-type reviewers to fill out a quick evaluation form after watching a recording of the rehearsal that lasts about 30 minutes. I will send a $50 Amazon gift certificate as my thanks (or just my thanks to the folks who can’t accept them because of employer policy). Let me know if you can help out every now and then. I provide each Webinar presenter with three reviews of their practice session — two from CIOs and one from me – to make their live day webinar the best it can be in terms of educational value and in keeping my short attention span engaged. If you’d like to present a webinar, I’m all ears for that, too – I’m up for anything that is educational and interesting to readers.
Upcoming Webinars
June 24 (Tuesday) noon ET. Innovations in Radiology Workflow Through Cloud-Based Speech Recognition. Sponsored by nVoq. Presenters: David Cohen, MD, medical director, Teleradiology Specialists; Chad Hiner, RN, MS, director of healthcare industry solutions, nVoq. Radiologists – teleradiologists in particular – must navigate multiple complex RIS and PACS applications while maintaining high throughput. Dr. Cohen will describe how his practice is using voice-enabled workflow to improve provider efficiency, productivity, and satisfaction and how the technology will impact evolving telehealth specialties such as telecardiology.
June 24 (Tuesday) 2:00 p.m. ET. Share the Road: Driving EHR Contracts to Good Compromises. Sponsored by HIStalk. Presenter: Steve Blumenthal, business and corporate law attorney, Bone McAllester Norton PLLC of Nashville, TN. We think of EHR contracts like buying a car. The metaphor has is shortcomings, but at least make sure your contract isn’t equivalent to buying four wheels, an engine, and a frame that don’t work together. Steve will describe key EHR contract provisions in plain English from the viewpoint of both the vendor and customer.
June 25 (Wednesday) 2:00 p.m. ET. Cloud Is Not (Always) The Answer. Sponsored by Logicworks. Presenter: Jason Deck, VP of strategic development, Logicworks. No healthcare organization needs a cloud – they need compliant, highly available solutions that help them deploy and grow key applications. This webinar will explain why public clouds, private clouds, and bare metal infrastructure are all good options, just for different circumstances. We’ll review the best practices we’ve learned from building infrastructure for clinical applications, HIEs, HIXs, and analytics platforms. We will also review the benefit of DevOps in improving reliability and security.
June 26 (Thursday) 1:00 p.m. ET. The Role of Identity Management in Protecting Patient Health Information. Sponsored by Caradigm. Presenter: Mac McMillan, FHIMSS, CISM, co-founder and CEO of CynergisTek. Identity and access management challenges will increase as environments become more complex, users create and manage larger amounts of sensitive information, and providers become more mobile. Learn how an identity and access management program can support regulatory compliance, aid in conducting audits and investigations, and help meet user workflow requirements.
July 2 (Wednesday) noon ET. The CIO’s Role in Consumer Health. Sponsored by HIStalk. Presenter: David Chou, CIO, University Of Mississippi Medical Center. We are moving towards an era where the consumer is searching for value. Healthcare is finally catching up with other industries and this is forcing health care providers and health plans to rethink their "business model" as consumers test new decision-making skills and demand higher quality and better value. Technology can provide value in this space as we move towards a digital healthcare.
Speaking of webinars, Steve Blumenthal’s abstract for his EHR contracts one was witty, so we suggested he do a video introduction. I can’t help but snicker every time I play it, especially when I see his fake smarmy, “Oh, I just noticed the camera was running five feet from my face” introduction. He’s a good actor and funny (even by non-lawyer standards), so it should be a good webinar.
Acquisitions, Funding, Business, and Stock

Cost management systems vendor Equian, which changed its name from Health Systems International a few weeks ago, completes its acquisition of AfterMath Claim Science, which offers data mining cost analysis solutions to payors.
Consulting firm VeritechIT acquires Health Technology Solutions, a one-employee consulting firm run by Terry Grogan, acting CTO for Temple University Hospital (PA). It appears from VeritechIT’s bio page that Michael Feld — listed as founder, president, and CEO – is also acting CTO of Lancaster General Health System (PA).
Medical device maker Medtronic acquires competitor Covidien for $42.9 billion in cash and stock, giving Medtronic a convenient excuse to move its headquarters out of US tax jurisdiction to Ireland even though the company’s name will continue as Medtronic and its “operational headquarters” will remain in Minneapolis. Several companies have taken the acquisition route to evade the 35 percent US corporate tax rate that’s one of the highest in the world, the only method remaining to accomplish that since US laws now prohibit a company from simply moving its headquarters offshore to pay a lower tax rate (12.5 percent in Ireland). The deal also gives Medtronic a place to spend the $14 billion of foreign profits it has parked offshore to avoid paying US taxes.

From the Streamline Health Solutions earnings call:
- President and CEO Bob Watson apologized for the late financial report, caused by a change in CFOs, a change in audit firms, and completion of an internal controls audit required by the company’s market capitalization.
- The company is offering the commercialized version of analytics software it acquired last year from Montefiore Medical Center.
- In a refreshingly honest announcement, Watson said the company erred in taking on work to help its clients go live faster in hopes of being able to recognize more revenue from the backlog, which Watson said didn’t really help and cost the company twice as much as expected. He concluded, “An outside consultant stepping into XYZ health system doesn’t have the innate natural knowledge of how that health system’s IT infrastructure is organized and therefore cannot be that helpful. So that was our plan that didn’t work.”
- Sales of computer-assisted coding solutions were delayed after the “disastrous” results experienced by early adopters of “some of our well-known competitors.”
- The acquisition of Unibased Systems Architecture resulted in one new Q1 sale and renewals worth a total of $10 million.
- The company’s products have been renamed within the Looking Glass family nameplate and underlying analytics platform.
Healthcare benefits electronic payment systems vendor Evolution1 will be acquired by corporate payment solutions vendor WEX for $532.5 million in cash. The Fargo, ND-based Evolution1 has 300 employees.
Sales

Children’s Hospital Los Angeles (CA) and Wisconsin Statewide Health Information Network (WI) choose Orion Health’s Rhapsody Integration Engine.
The FHP Health Center (Guam) selects eClinicalWorks.

Thibodaux Regional Medical Center (LA) will implement Health Catalyst’s Late Binding Data Warehouse and Analytics platform.
People

Practice Fusion names Robert Park (Chegg) as CFO.

Dan Baker (NextGen) joins Remedy Informatics as SVP of sales.


HealthStream hires Tom Schultz (Infor) as SVP of sales and promotes Michael Sousa to SVP of business development.
Payment financing company CarePayment names Craig Hodges (Emdeon) as CEO. Outgoing CEO Craig Foude will stay on as board chair and managing partner for Aequitas Capital, founder and owner of the company.
Announcements and Implementations

Aesynt, the former Pittsburgh-based McKesson Automation plus its acquired Health Robotics, says it signed 18 IV automation contracts in Q4. Those are for the former Health Robotics i.v.STATION hospital IV room products.
The Central Texas division of Baylor Scott & White Health goes live on API Healthcare’s ShiftSelect.
Memorial Hermann (TX) launches Wolters Kluwer UpToDate Anywhere for its 12 hospitals and 5,000 affiliated physicians.
Government and Politics
The VA will issue an RFP next week for a commercial patient scheduling system to work within VistA, with its CIO saying that while VistA’s clinical system is “one of the best out there,” its non-clinical modules haven’t kept up. He also says that current events make it obvious that the new system will include extensive auditing features to review changed appointments. The VA gave up on a previous attempt to build its own scheduling system a few years ago and nothing seemed to happen with the open source Health eTime app that won the VA’s scheduling system competition last fall.
Health IT Now says HITECH has paid $24 billion to subsidize information-hogging EHRs and wants HHS to make data sharing (at no extra customer cost) a certification criterion. Health IT Now is a coalition of patient groups, providers, employers, and payers – it claims that Aetna, American Cancer Society, AHIMA, IBM, Intel, Oracle, the US Chamber of Commerce, and a few health systems are members – whose agenda involves promotion of interoperability standards, Meaningful Use changes to emphasize lower cost and improved outcomes, innovation and increased use of telemedicine, and medical licensing that spans state boundaries. I first reported on the group in mid-2007, saying, “The founding members include a couple of former Congressmen ([Nancy Johnson and John Breaux] and a cross section of influential medical, professional, and other organizations. I don’t think I’ve heard anything from them since (their “About” page claims “we will continue a formidable education agenda in 2012”), so while I agree with their platform, I don’t think it’s having much of an impact inside the Beltway. The only named employee is Executive Director Joel White, a former Congressional staffer who omits the group from his LinkedIn profile and instead list himself as President and CEO of Horizon Government Affairs, which sells political services and operates four other non-profit coalitions: Council for Affordable Health Coverage, Rare Disease Legislative Advocates, Prescriptions for a Health America, and Newborn Coalition.
DoD releases the third and near-final draft of its $11 billion DHMSM EHR solicitation, removing the veterinary medicine requirement, eliminating required use of any particular development methodology, and making the contract performance-based. Vendors will have a chance to ask questions on Industry Day next Tuesday, June 24, which would be fun to write up if you’re going.
Innovation and Research
Microsoft announces Azure Machine Learning, available in July, that will allow users who store data in its Azure cloud to use drag-and-drop predictive analytics. Potential healthcare uses include scheduling, reducing readmissions, and anticipating disease outbreaks.
Other
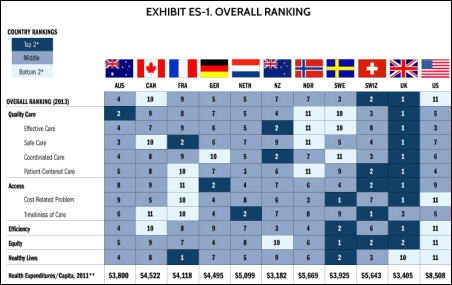
Research by The Commonwealth Fund finds that the US health system is not only the most expensive among 11 developed nations, it is also the worst, coming in dead last in access, efficiency, equity, and healthy lives, primarily due to the lack of universal healthcare coverage and support for the patient-physician relationship. The report also calls out the stubborn resistance to using healthcare IT. The bright spot, the report says, is that the Affordable Care Act is improving access and the system is moving toward more value-based payments. Methodology footnote: the study was done by surveying around 3,000 US residents with a self-rated health status of below average and recently treatment for a serious problem that involved at least one hospitalization, so the sample size wasn’t very large and the results reflected patient perception more than hard measures. The president of The Commonwealth Fund is former National Coordinator David Blumenthal, MD, so naturally the report pays disproportional attention to EMRs. Still, nothing in the results is all that surprising since it measures overall health of a cross-section of citizens, not just the specific healthcare outcomes of the more privileged among us.
The Wall Street Journal profiles Dignity Health’s use of Google Glass for clinical documentation, which it claims allows physicians to double the amount of time they can spend with patients. Dignity is using software from startup Augmedix to send Glass-collected information and commands to the EMR. It’s a small pilot started in January 2014 – the CMIO and two other docs – but they say manual EMR entry was reduced from 33 percent of their total time to 9 percent.
An apparent tornado damaged several homes and an elementary school within a mile of Epic’s Verona, WI campus Tuesday morning, but nobody was hurt.

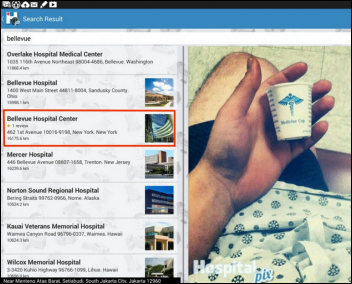
Overlake Hospital Medical Center (WA) gets a S&P bond ratings upgrade to A, primarily due to completion of its Epic implementation.
In China, Internet giant Alibaba, which has more sales than eBay and Amazon combined and is planning a US IPO, unveils a 10-year plan to disrupt China’s notoriously backward hospital system with online payments, patient scheduling, e-prescribing, hospital transfer, insurance claims management, and eventually wearables and other prevention technologies. The company had released a patient self-scheduling application for 600 hospitals last year to fix the eight-hour process of getting an appointment, but the government shut it down over privacy concerns (not mentioning that the site competed with the government’s own online service). The announcement of Future Project is here, although you should probably be able to read Chinese since Google translates it as, “Today, Alipay announced a program called ‘future hospital.’ Payment was originally conducted in hospitals, registered, classified ad will be transferred to PayPal platform. The implementation of this plan is completely far away from us, section house, ‘said the doctor chase behind the ass, give praise it pro’ story can become true?” And in other breaking news, all your base are belong to us

Alexian Brothers Health System (IL) cancels plans to form an accountable care entity to manage Medicaid patients, saying it’s too hard to connect the 10 EHRs used by 80 percent of the doctors, not even counting those that might have been added to the network later. The ACE would have been required to connect 60 percent of its network to the Illinois HIE within 15 months, include 100 percent within 30 months, and file electronic summaries of care for 70 percent of the network within 15 months.

CHIME’s Keith Fraidenburg tweeted out this photo of Tim Stettheimer presenting at the CHIME/AMDIS CMIO Boot Camp at Ojai, CA this week. Attendees are welcome to send me a write-up about the experience.
Pittsburgh insurer Highmark stops paying higher physician chemotherapy fees devised by hospitals buying oncology practices and then billing out drugs at the much higher hospital outpatient rate. Other insurers are trying to hold down oncology costs by paying oncologists a stipend to use less-expensive (and less-profitable) chemo regimens or bundling all treatment costs into a flat payment. Brand name chemo drugs cost an average of $10,000 per month, giving physicians a financial incentive to use more expensive ones as insurance companies haven’t protested for fear of losing oncologists in their network.

Mary Milroy, MD, the new president of the South Dakota State Medical Association says EHRs add an hour of busy work to a doctor’s day, adding that, “The systems we use are cumbersome, designed by IT people and not medical people. The huge problem is they don’t communicate.” Her clinic uses NextGen, another practice she covers uses Epic, and the local hospitals use Epic and Meditech. She says none of them talk to each other.
HIMSS Analytics has issued a new report about cloud computing, but with that ever-blurring line between whether HIMSS is a member organization or a vendor, you can’t download it without providing your email address, telephone number, job title, and other contact information for the inevitable sales cold call. I’m still not clear on how HIMSS managed to change HIMSS Analytics from a for-profit subsidiary to part of the non-profit HIMSS.
Non-profit patient advocate group Stupid Cancer launches an Indiegogo campaign to raise $40,000 to develop its free Instapeer app, which will connect young cancer patients to other patients, survivors, and caregivers.

In England, Health Secretary Jeremy Hunt says new guidelines calling for hospitals to list the name of each patient’s doctor over their bed is a “huge step forward for patient safety” since it’s not always clear where the medical buck stops. A spokesperson for a patient group said writing names on a board is fine, but that won’t accomplish much if the doctor doesn’t stay in touch with the patient.
Sponsor Updates
- Regenstrief Institute joins ConvergeHEALTH by Deloitte, a real-world evidence and analytics consortium.
- SD Times names InterSystems and its Cache’ system as one of the software industry’s top 100 innovators in the Database and Database Management category..
- RelayHealth announces that RelayHealth Financial has bolstered RelayAssurance Plus 5.0, providing transparency into your claims lifecycle.
- AirWatch by VMware opens registration and lineup of analyst speakers for the AirWatch Connect Global Tour 2014 in Atlanta, London, and Sydney.
- McKesson launches Benchmark Analytics service to provide custom reports and consultation to optimize performance.
- GetWellNetwork CEO Michael O’Neil discusses the CDC Morbidity and Mortality report on the cost of cancer survivorship with a local journal.
- Kareo and Falcon EHR partner to provide cloud solutions to nephrology practices.
- Gartner names Informatica as a Leader in the 2014 Magic Quadrant for Structured Data Archiving and Application Retirement.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis .
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.

























































"A valid concern..." Oh please. Everyone picks the software they like and the origin of that software is an afterthought.…