HIStalk Interviews Ed Marx, Chief Digital Officer, The HCI Group
Ed Marx, MS is chief digital officer of The HCI Group of Jacksonville, FL.

Tell me about yourself and your job.
I started my health career at age 16 as a janitor in a healthcare facility. Since that day, I knew my purpose in life was in healthcare. I didn’t know how it would manifest itself. Certainly not as a chief digital officer for a major global organization.
What does a chief digital officer do?
My objective is twofold. One is to make sure that we as an organization digitally transform ourselves. I always say that you have to eat your own dog food. If we are going to consult or sell or whatever to customers around the world, we had better be able to use ourselves as the number one use case.
Second is to take those same learnings and teach people how to leverage technology in order to see digital transformation in whatever their specific objectives are. It runs the gamut.
What is digital? I can give you the formal definition as I see it, but really it’s a natural evolution of technology, but centered around experience. Helping organizations achieve that and to continue their evolution to enable the organization’s objectives.
What organizations are doing digital transformation well in healthcare?
I give credit to everyone who is doing anything, because at least they are moving the needle. I’m going to answer your question specifically with a couple of the obvious ones, but in addition to that, a lot of small hospital systems are doing good things.
We always highlight the bigger ones that have more resources. Certainly you talk about the Mayo Clinic and Cleveland Clinic. They have done a lot for a long time to continue that evolution, and now revolution, of technology enablement. Those are a couple of organizations that are doing a really nice job.
The impetus of the situation that we are in today is only going to help everyone accelerate that journey. That journey has been slow, especially compared to other industries. But we have an opportunity to catch up and see the fruition of all of that technology can do to enable superior clinical care.
Are health systems looking at new entrants like Walmart, Amazon, and Walgreens that have created new consumer experiences and just throwing up their hands and say they can’t match them, or are they choosing specific aspects they can implement?
We have new entrants because those companies are looking to continue to grow their margin. They look at the percentage of GDP that healthcare makes up and think it’s an area that they should focus on.
But a second reason, which maybe never should have happened, is that few of us were leveraging digital transformation and changing the whole experience. You’ve seen that in other industries. People get upset when you compare healthcare to other industries and I know healthcare is different, but from a technology point of view, you saw disintermediation of multiple industries by new entrants who said, we’re going to be more about the experience. We’re going to use automation and “digital,” quote unquote. We can do it at a lower cost point. Those sorts of things.
Whether it’s big tech or it’s retail, they are seeing the same thing. Not only is there a huge opportunity in terms of what the spend is, but in healthcare, we haven’t done it necessarily the best way because we weren’t forced to. Now we have globalism, consumerism, and retail giants who are all focused about the experience of big tech. That’s why we’ve seen this happen.
We need to learn quickly. What is the secret sauce that a retail giant might bring in terms of the experience? That’s really it. I keep using the word “experience,” but it’s really a focus on the experience. Then enabling all the technologies that they are using on a day-to-day basis to make their life easier. That’s what we need to learn.
In some cases, we need to partner and we should partner. Sometimes it’s better to partner and do good things in the world than to sit back and watch your business be disintermediated.
Sometimes it’s better to be second in learning from the mistakes made by whoever got there first. Will we see organizations leapfrogging that first generation of consumerism?
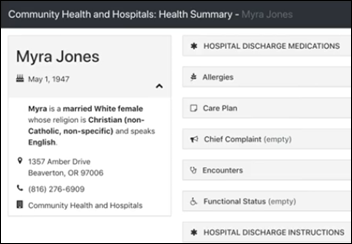
That is happening with some forward-thinking hospitals and health systems. They are taking the time to analyze what’s going on in retail, how they created those new, enhanced experiences, and taking some of those learnings. We’re seeing that now. I’ve heard of many health systems that are working on their basic patient portal, and you know those aren’t about the experience. It’s a good start, but again, years behind what other industries have been doing.
Some forward-thinking hospitals and healthcare systems are keeping that as the foundational base because of all the integration it has. They they are building layers on top of it that get all about the experience. So I do think you can … I don’t know if it’s actually leapfrogging, but at least keeping pace.
The leapfrogging might happen in partnerships. It will be hard for a healthcare organization to compete with the capital and innovation mindsets that some of these outside entrants bring, whether it’s retail or big tech. I would see it very challenging for a healthcare organization, especially an average healthcare organization, to bring together the mindshare and the capability to leapfrog, but I think you could leapfrog if you selected a good partner.
How will the coronavirus pandemic and the economic shock that accompanies it affect healthcare’s digital transformation?
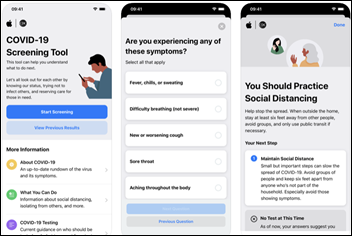
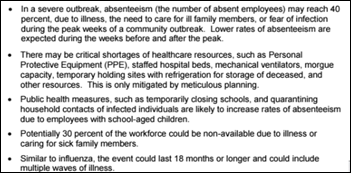
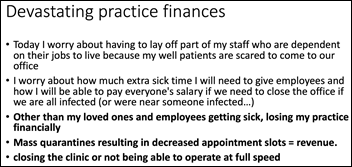
I’m thinking two or three things, and I’ve thought quite a bit about this in the last several days. One is that it’s going to be the pure acceleration of everything we’ve been trying to do, the whole virtual care continuum. I came from a leading organization and 1% of our outpatient visits were virtual, with a goal of getting to 50% in four years. I haven’t checked back, but I bet they are pretty close to 50% now.
Part of that stack, too, is healthcare at home. This was another thing that I put out there, that 25% of inpatient visits will be at home in the next four years. I get the feeling we’re going to get there much quicker.
Those are two examples. I think those are permanent. I don’t think that after this, we’re going back.
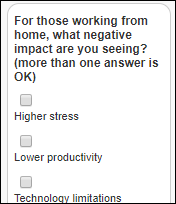
Another is a new way of work. I’ve been a big proponent of working from home as a way of work for 10 years. We’re not going to go back. There is no reason, ever, to travel to go use a computer. I’m sure some companies and hospitals will disappoint me, but those days are gone. That will do tremendous things for healthcare in terms of taking out costs.
These concepts of virtual care and a new way of work will come together to change everything. Why would you ever want to go and sit in a waiting room? Those two changes are going to be permanent.
How will the possible new emphasis on public health change the health IT discussion with regard to interoperability, analytics, and aggregating patient data?
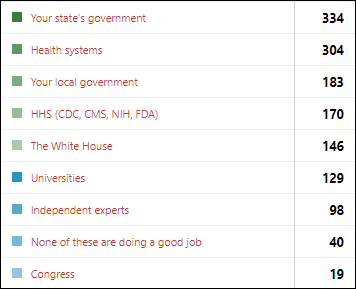
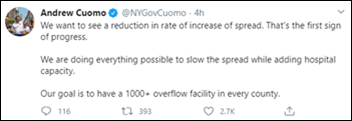
I’m less optimistic on that one. I hope this brings our country together to be more serious and more intentional on public health. It took this crisis, this terrible situation, to make it happen. You bring all these smart people together and the resources that everyone has with public-private and we can do amazing things. We should have done it a long time ago.
I’m hoping that this is a catalyst that changes our public health for good. That we become a more healthy country, that people take wellness more seriously and more personally, and that our country is able to be predictive and preventative at the same time so that nothing like this could ever occur again.
Do you have any final thoughts?
I hope that my fellow CIOs and chief digital officers continue to lead the trajectory that we are on. I’ve always been critical of myself and my peers in terms of why we lag behind other industries. Now, because we’ve been given clarity, focus, and budget, I’m hearing from a lot of my colleagues about all the awesome things they are setting into motion now. May it always continue. May we take that leadership mantle and not tarnish it, but brighten it for the good of our patients and the communities that we serve.




































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…