News 3/20/20
Top News
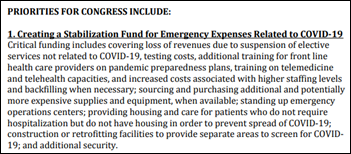
The American Hospital Association, American Medical Association, and American Nurses Association jump on the federal government bailout train by asking for $100 billion to offset COVID-19 diagnosis and treatment.
Hospitals say they will lose revenue from delaying elective procedures and will spend more on training, supplies, and employee childcare.
The letter to Congress didn’t mention that insurers, including the federal government in the form of Medicare and Medicaid, will pay hospitals and doctors for providing care to COVID-19 patients.
HIStalk Announcements and Requests

I’ve added a “comments” link to the bottom of every HIStalk post, a much-requested feature that allows reading or adding comments without scrolling back up.
Unrelated, outside of social distancing: need something interesting to eat with your canned soup? I made what I will modestly call “good” baguettes that were easy (no kneading), quick, and required just flour, water, salt, and yeast. They passed Mrs. H’s test of being crusty on the outside and soft (but not spongy) in the inside. You might as well have something homey while at home and make it smell good besides.
Webinars
March 25 (Wednesday) 1 ET: “Streamlining Your Surgical Workflows for Better Financial Outcomes.” Sponsor: Intelligent Medical Objects. Presenters: David Bocanegra, RN, nurse informaticist, IMO; Alex Dawson, product manager, IMO. Health systems that struggle with coordinating operating rooms and scheduling surgeries can increase their profitability with tools that allow for optimal reimbursement. This webinar will identify practices to optimize OR workflows and provider reimbursement, discuss how changes to perioperative management of procedures can support increased profitability, and explore factors that can impede perioperative workflow practices.
March 26 (Thursday) 12:30 ET. “How to Use Automation to Reduce ‘My EHR is Slow’ Complaints.” Sponsor: Goliath Technologies. A common challenge is that a clinician is ready to work, but their technology is not. EHRs can be slow, logins not working, or printers and scanners are offline. Troubleshooting these end user tickets quickly is nearly impossible, especially in complex environments that might include Citrix or VMware Horizon. This webinar will present real-world examples of how leading health systems are using purpose-built technology with embedded automation and intelligence to proactively anticipate, troubleshoot, and prevent end user performance issue across their IT infrastructure and EHRs.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Sales
- Nebraska Health Information Initiative selects NextGate’s enterprise master patient index.
- The Cardiovascular Center of Puerto Rico and the Caribbean will implement Medsphere’s CareVue EHR.
- Topeka, KS-based HIE Konza will use Diameter Health’s data normalization and enhancement software to deliver de-duplicated CCDs to its members.
People



MDLive names Chairman Charles Jones CEO, Christopher Shirley (Catasys) CFO, and Andy Copilevitz (Walgreens) COO.

University of Washington Medicine pathology professor Stephen Schwartz, MD, PhD died Wednesday of COVID-19.
Announcements and Implementations
Children’s Hospital of The King’s Daughters (VA) implements analytics and data management software from Dimensional Insight.
Cobre Valley Regional Medical Center (AZ) rolls out Meditech Expanse, with consulting help from Engage.
![]()
Health Catalyst will make available COVID-19 patient and staff tracking, public health surveillance, and staff augmentation support capabilities.
Jump Technologies makes its inventory management software available to hospitals for free for a limited time.
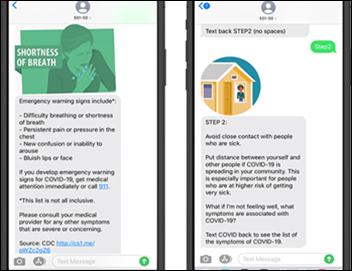
Dina offers COVID-19 rapid response tools, including self-assessment of quarantined patients, remote monitoring of discharged and isolated patients and healthcare workers, patient self-assessment, and checking the health of staff members daily with text-based remote screening questions.
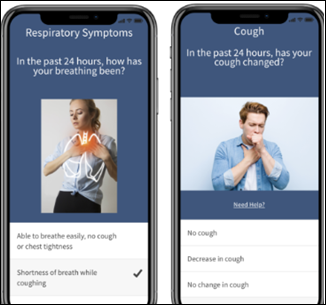
Blue Shield of California offers its network hospitals a customizable COVID-19 Screener and Emergency Response Assistant for consumers. Mobile device or hospital website users answer questions whose answers direct them to the most appropriate medical setting. Blue Shield is covering the cost of implementation, which takes 48 hours, and three months of updates. The tool was developed by Gyant, which offers digital front door and patient engagement technology.
Allscripts announces its COVID-19 response, which includes a fast-tracked telehealth implementation plan for FollowMy Health, rollout of an EHR-agnostic automated triage tool, and employee travel restrictions.
Registry reporting vendor Iron Bridge offers free access to system to allow hospitals and labs to report COVID-19 cases to the CDC faster.
Verge Health offers free access to its Compliance Rounding solution that helps hospitals complete the COVID-19 CMS Infection Prevention Worksheet and CDC Hospital Preparedness Assessment
CompuGroup Medical offers free provider use of CGM ELVI Telemedicine, which allows them to collect patient information, share information, and provide care from anywhere.
Government and Politics
HHS will allow physicians to practice across state lines in an effort to prevent staffing shortages during the COVID-19 pandemic.
HHS asks for $21 million in additional 2020 funding for ONC to “support the emergency expansion of a patient lookup system to aid patients and COVID-19 medical response” via an online database.
COVID-19

Former FDA Commissioner Scott Gottlieb, MD provides thoughts on COVID-19:
- Therapeutic response involves three efforts: developing a vaccine (which he thinks will take two years), trying existing antivirals, and developing an antibody that can be given as a monthly injection to protect frontline healthcare workers and high-risk people.
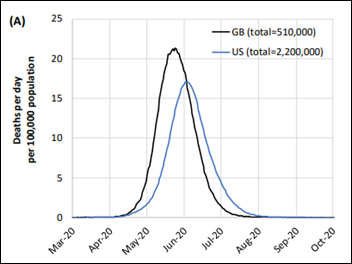
- He expects the epidemic to peak in late April and early May, with hopes that it will have run its course by July and will leave enough people who have recovered from it to create herd immunity. His biggest fear is that it will come roaring back in September and cause another epidemic that will last all winter.
- Point-of-care diagnostics similar to the flu swab are needed to allow doctors to quickly quarantine people who are infected instead of waiting 24-48 hours (he says that test can be developed within three months). Then roll out widespread surveillance testing to see how the virus is circulating. He says the nation’s posture is not sustainable unless such surveillance can be put in place while waiting for a vaccine to be developed.
Former National Coordinator and Aledade founder and CEO Farzad Mostashari, MD – who has strong syndromic surveillance experience — identifies issues with COVID-19 data collection and analysis, likening the current state of testing to giving a haphazard set of people a new drug, collecting information sloppily, and then trying to use that information to determine whether it works:
- The public health value of counting positive tests is minimal without understand each individual’s condition, their source of exposure, and how they compare to those whose tests are negative.
- The preliminary data that is being reported to the CDC is frequently missing hospitalization status, ICU admission status, death, and age. CDC does not know the denominator of how many people have been tested.
- Labs should be required to submit aggregate information on every test they perform, not just those with positive results.
- Sentinel testing needs to be performed.
- A serosurvey is needed, where a random sample of households in a large city is tested and surveyed to understand the fatality and infection rates.
- ED visits for cough, fever, and flu-like symptoms need to be studied to determine how many are COVID-19 related.

Bill Gates address coronavirus in a Reddit “Ask Me Anything,” where he observes about COVID-19:
- US testing is disorganized. The federal government needs to provide a questionnaire website for consumers that prioritizes the testing, such as making sure that healthcare workers and the elderly are tested first.
- Labs that perform COVID-19 testing need to be connected to a national tracking system.
- Gates and his researchers feel that the Imperial College models are too negative given that China’s shutdown reduced case numbers that showed little rebound. The Imperial College models were based on influenza.
- He expects treatments for COVID-19 to be available before a vaccine, which would keep people out of ICUs and off ventilators. The Gates Foundation is funding research on bringing all industry capabilities into play.
- The Foundation is working on a plan to send test kits to people at their homes to try to offset the US’s disorganized testing.
- He expects individuals to be assigned digital certificates to show that they have recovered, or when a vaccination is available, that they have received it.
Mitre urges the federal government to take immediate action to halt the short doubling time of new COVID-19 cases in the US:
- Close all schools.
- Give businesses incentives for allowing working from home.
- Shut down all places of social gathering, including restaurants, bars, theaters, concerts, and sporting events.
- Provide home food supplies to everyone who needs them.
- Seal the US borders to all forms of traffic and transport.
Cerner temporarily closes its Realization campus after an employee tests presumptively positive for COVID-19. The company had already announced a work-from-home policy for most employees.
National medical group Mednax comes under fire for telling clinicians that if they require a two-week quarantine following coronavirus exposure, they must use their sick leave or PTO.
First Affiliated Hospital of Zhejiang University and Alibaba Health publish a 60-page, detailed COVID-19 prevention and treatment handbook that accumulates information gained from China’s outbreak.
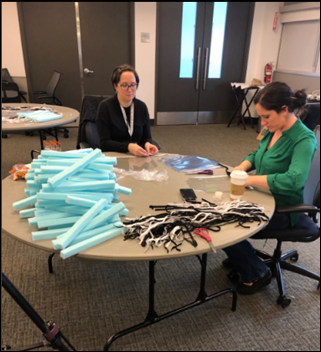
Healthcare workers at Providence St. Joseph Health in Washington fashion face shields out of supplies from craft stores and Home Depot, including marine-grade vinyl, industrial tape, foam, and elastic. The health system is evaluating the quality of material used for surgical tray liners in case they need to repurpose them for masks.
YMCAs in Memphis, TN convert into childcare facilities for healthcare workers and first responders.
US funeral homes are asking families to scale back or postpone funeral services, limit attendees, and conduct services virtually to comply with federal guidelines that limit gatherings of more than 10 people. The funeral homes are also increasing worker protection since nobody knows now long the coronavirus can live on the tissue of the deceased.
Pulizter-winning cartoonist Mike Luckovich of The Atlanta Journal-Constitution posted this work.
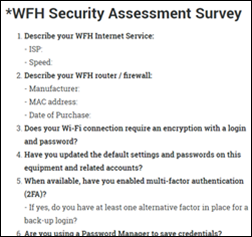
Privacy and Security
Government officials in Massachusetts warn the public, particularly seniors, of COVID-19 testing scams: “Testing can only be ordered by a treating physician. We have heard about teams in white coats going door-to-door offering virus testing. This is NOT a valid offer. What they are really interested in is robbing the elderly or stealing their identity. And we have heard reports of callers pretending to be a nurse offering test results once they get a credit card number. These kinds of calls are also not for real.”

Several ransomware hacker groups say they will refrain from attacking healthcare organizations during the pandemic.
Other
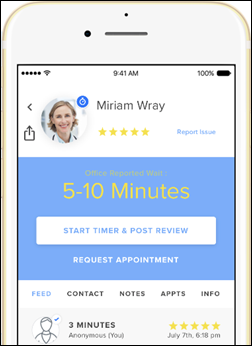
Telehealth services are being overwhelmed with a surge in patients that is stressing their technology and their supply of physicians. Cleveland Clinic reports a fifteen-fold increase in telehealth visits and is doing phone consults and recorded video visits to try to keep up. University of Pennsylvania has increased telehealth staffing from six to 60, but is running days behind, while Jefferson Health is receiving 20 times the number of virtual visits and is scrambling to enlist more doctors.
ProPublica looks at the role medical conferences have played in spreading COVID-19.
The New York Times calls the Zoom videoconferencing service “where we work, go to school, and party these days.” People are convening virtual birthday parties and cannabis hangouts, teens are referring to themselves as “Zoomers,” college students are using it for blind dates, it’s being used for virtual college graduations, and experts worry that it will turn into a Facebook-like cesspool of live online mass shootings and child porn that will force the company to moderate content. Zoom’s soaring share price values the company at $29 billion.
Sponsor Updates
- Kyruus incorporates Gyant’s chat-based virtual assistant into its patient-provider routing and scheduling software.
- Intelligent Medical Objects will release free COVID-19 terminology content and value sets to customers on March 26.
- Omni-HealthData adds enhanced social determinants of health data to its health information management software.
Blog Posts
- Brown Clinic: Community Values with Leading-Edge Technology (EClinicalWorks)
- A Message from Ensocare’s President on Our Coronavirus Response (Ensocare)
- Trouble Finding Citrix Expertise? The Answer is Technology (Goliath Technologies)
- Remote work essentials: How IT can prepare for a distributed workforce (Google Cloud)
- Digital health solutions for business continuity during a pandemic (Greenway Health)
- COVID-19 Pushes Telemedicine Into the Spotlight – Are You Prepared? (PMD)
- Pandemic Response as part of your DR/BC Solution (The HCI Group)
- This Historic Ruling by the ONC Means More Empowered Patients (Healthwise)
- While we work from home, healthcare providers stand on the pandemic frontline (Hyland)
- Yale New Haven matches workstation locations to clinician log-ins to help manage Coronavirus (Imprivata)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.

























Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…