Top News
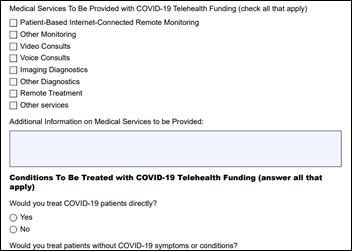
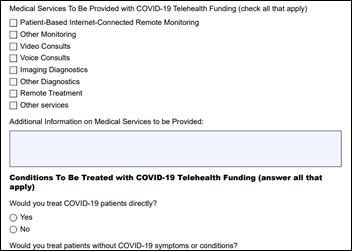
The FCC opens the application window for its $200 million COVID-19 telehealth cost reimbursement program.
Applications are completed on an eight-page fillable PDF form that is then emailed to the FCC.
Non-profit healthcare provider sites that treat patients, schools, health departments, rural clinics, and skilled nursing facilities are eligible to have their expenses reimbursed for telecommunications and connected devices.
Awards are expected to be under $1 million per applicant, with the money being assigned on a rolling basis until the $200 million has been committed.
Reader Comments
From Just Laid Off by Allscripts: “Re: the US healthcare system. We like to believe that the public needs are best served when the organizations that provide the needs are run like businesses. Now we’re seeing the downside. While all healthcare organizations across the globe will struggle with the need to care for so many sick people, it seems beyond dysfunctional that hospitals might close or have to layoff healthcare workers because of not doing elective surgeries.” We also have the problem that most Americans couldn’t afford to pay modest healthcare bills even before the pandemic took income and health insurance away from millions of them. I’ve seen estimates that health insurance premiums will rise 40% or more next year, which takes us further down the death spiral of unaffordable premiums, unaffordable deductibles and co-pays, and health systems that expect to be paid richly for providing sometimes questionably necessary services. On the other hand, it wouldn’t surprise me if Americans get healthier over the short term as we reduce our contact with profit-maximizing providers and thus the dangers of overprescribing, overtreatment, elective surgery, and medical errors (the uptick in poor outcomes post-pandemic will be conveniently blamed on deferred maintenance). What we want or need as patients is incidental to whatever makes the cash registers ring. I would like to think that we as patients – which is everybody, not just all at the same time — will demand better, but most of us don’t have a lot of lobbyists and politicians in our pockets.
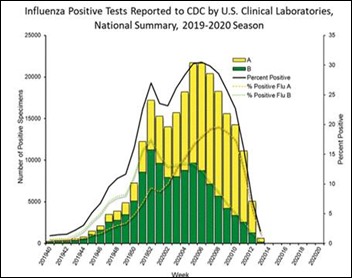
From Curves Flattened: “Re: COVID-19. Being sequestered accomplished the goal of flattening the curve. Well done!” My joy is restrained by the fact that “flattening the curve” is not the same as “reducing the area under the curve.” Drastic societal efforts so far were intended only to extend the timeframe over which people get infected and require hospital care. Your odds of being taken out by COVID-19 in the long term haven’t changed, other than maybe you get the chance to die unconscious on a ventilator instead of while gasping for air without one. We have no proven treatments and no vaccine. Meanwhile, our globally underperforming healthcare system isn’t the immediate problem – it’s that our world-leading logistics failed us in being unable to source and distribute COVID-19 tests, ventilators, and personal protective equipment.
From Tommy Hawk: “Re: webinars. I suggest that vendors, at least for the near term, allow webinar registration using non-corporate email addresses. This would allow those of us who are newly unemployed to continue our education and maybe our employment.” I agree, although for broader reasons. We make recordings of the webinars that we produce freely viewable on YouTube (I think we were the first to do this). We discourage webinar sponsors from requiring more than the absolute minimum of signup information since studies have shown a huge drop-off in registrants if you bug people to list their employer, job title, telephone number, buying timeline, etc. in ensuring a nagging contact afterward. I haven’t seen many webinars whose content would help a competitor, and I haven’t seen many companies whose competitive intelligence strategy consists of watching webinars. It reminds me of the old HIMSS conference days, when a few paranoid and mostly crappy companies posted sentries around their booth perimeter to shoo away non-providers who might be seeking out the nuclear secrets that were hidden inside.
From Seagull Soaring: “Re: HIStalk. My communication is a simple thanks and gratitude for all of your hard work on HIStalk. I read your site nearly every day and it makes me better at my job. You provide a great service. Thank you.” I’m gratified at the several recent messages like this one that came out of nowhere. Thank you for those who sent them.
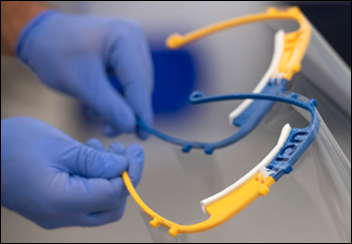
From Michael Raymer: “Re: ventilators. Your original post led to finding our first large private donor. We will return the first ventilators to clinical use this week, three weeks after the initial idea. Thanks for your help! We need help continuing to identify ventilators. We have acquired almost 50 in one week.” Health IT long-timer Mike is the co-founder of the non-profit Co-Vents, which is refurbishing retired ventilators for clinical use to meet the short-term need.
HIStalk Announcements and Requests
I’ve received some thoughtful answers from consultants about how their work is changing, as requested by a consultant reader who is struggling. Add yours to be included in my writeup later this week.
Webinars
April 15 (Wednesday) 1 ET: “Scaling front-line COVID-19 response: virtual education, screening, triage, and patient navigation.” Sponsor: Orbita. Presenters: Lawrence “Rusty” Hofman, MD, medical director of digital health, Stanford Health Care; Kristi Ebong, MPH, MBA, SVP of corporate strategy, Orbita. The presenters will describe how chatbots can be quickly deployed to streamline individual navigation to the appropriate resources, administer automated virtual health checks for monitoring and managing specific populations, increase access to screening and triage for high-risk populations across multiple channels (web, voice, SMS, and analog phone), and reach individuals in multiple languages.
April 28 (Tuesday) 1 ET: “COVID-19: Managing an evolving patient population with health information systems.”Sponsor: Intelligent Medical Objects. Presenters: Julie Glasgow, MD, clinical terminologist, IMO; Reeti Chauhan, senior product manager, IMO. IMO recently released new novel coronavirus descriptors to help clinicians accurately record diagnoses and also created free IMO Precision COVID-19 Sets to help identify and analyze patients with potential or documented infection. The presenters will discuss these new tools and describe how to use them optimally.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Life sciences data and managed services vendor IntegriChain acquires the life sciences division of Cumberland, which provides managed services, advisory services, and systems integration for life sciences contracts, pricing, and revenue management.

Marketing firm W20 acquires Symplur, a healthcare-specific social media tracking platform. W20 recently used the system to create a coronavirus media tracking tool for the California Life Sciences Association.
Sales
- Highmark Health, Allegheny Health Network, and Gateway Health will implement Aunt Bertha, which connects people to social services that can help with food, housing, and transportation.
People

Care team collaboration platform vendor Andor Health hires industry long-timer Raj Toleti, MS (Allscripts) as CEO and board chair.
Announcements and Implementations

Henry Schein Medical offers providers free 90-day use of VisualDx, which enhances telemedicine visits with shared images and documents.
QliqSoft adds patient and engagement content from Wolters Kluwer to its clinical collaboration and patient communication solutions.
ClaraPrice offers a service to help hospitals manage the ongoing reporting and payback of advance Medicare payments via the CARES Act.
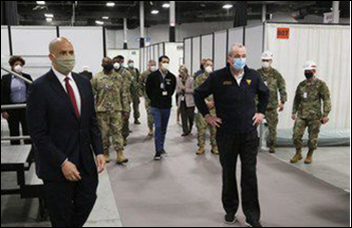
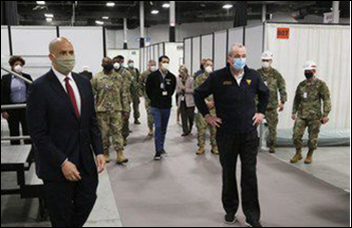
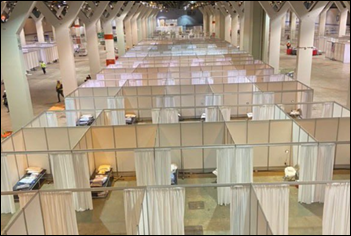
Epic announces in a second recent (and rare) press release that it has donated software and services to the temporary hospital that has been created in Meadowlands Exposition Center by University Hospital (NJ). Epic says its implementation took three days, with the first patient being admitted on the fourth day. The newly named Secaucus Federal Medical Station has beds for 250 non-COVID patients.
COVID-19
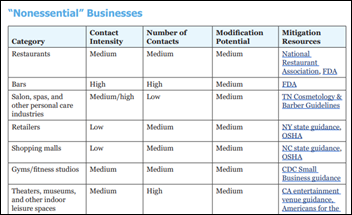
Former FDA Commissioner Scott Gottlieb, MD says in a Wall Street Journal op-ed piece that US employees may return to work as early as May, but employers should be prepared to offer onsite screening to detect infected but symptom-free workers. He says the rapid test platform of Cepheid is fast and requires less invasive swabbing, with other companies introducing similar machines. Gottlieb says that employers who can’t perform onsite testing should offer take-home tests or refer their employees to a local pharmacy or government program. He also recommends that employees who test positive continue being paid so they don’t have to choose between doing the right thing versus feeding their families.

James Wright, MD, medical director at the private equity-owned Virginia nursing home that has seen 45 COVID-19 deaths among its residents so far, says that American society has chosen to warehouse its senior citizens in underfunded facilities that can’t afford adequate staffing and that are forced by economics to offer non-private rooms that don’t have access to the outdoors. His facility lost much of its staff as the outbreak began since most of them work multiple jobs and were ordered by their other employers to stop working there to avoid spreading the infection among facilities. More than 50% of the facility’s residents who tested positive have died. Wright concludes that “this will not be the last untreated virus to decimate our elders” and that “a publicly funded nursing home is a virus’s dream.”
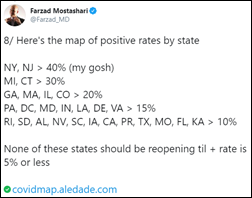
A Harvard professor of epidemiology says that we don’t have enough data to determine who in the population might have developed coronavirus immunity. He speculates that most COVID-19 patients develop some degree of immune response, but its strength and duration is probably variable, and creating herd immunity requires a large percentage of people whose immunity is long lasting. The US’s low testing rate makes analysis impossible, but results from better-responding countries suggest that herd immunity isn’t significant. The bottom line is that scientists can’t predict immunity until widespread testing for both infection and antibodies is performed. In the absence of immunity, the only hope is a vaccine.
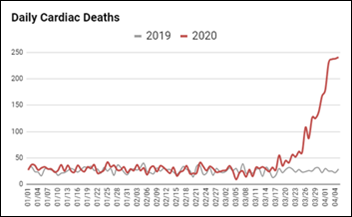
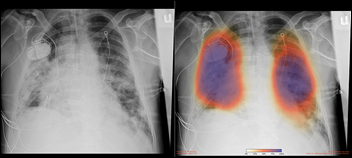
Preliminary evidence suggests that COVID-19 causes clotting events that can lead to thromboembolism, deep vein thrombosis, ischemic stroke, and possibly even cardiomyopathy. That may also explain why those patients go downhill so quickly from what seems like normal COVID-19 pneumonia. The presence of abnormal coagulation has been found to be predictive of pneumonia outcomes in COVID-19 patients, which could lead to recommendations that those patients be anticoagulated.
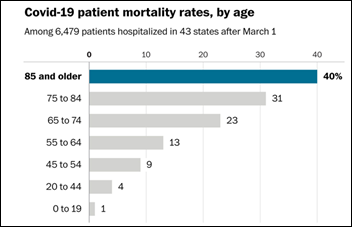
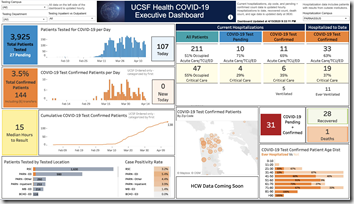
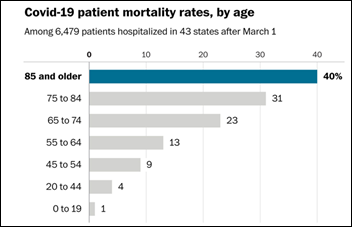
Analysis of the inpatient data of 1,000 hospitals by Allscripts subsidiary CarePort Health finds that COVID-19 mortality rates are about 10% overall, but 40% for those over age 85. A new finding from the analysis is that chronic kidney disease seem to increase death risk dramatically. More than half of patients who were hospitalized are under 65, while risk-adjusted death rates for men are 1.3 times that of women, both conclusions matching those of the CDC.

Beaumont Health launches what it says is the country’s largest coronavirus serology testing program, where it hopes to test volunteers from its 38,000 employees to measure the incidence of antibody formation among people who had no COVID-19 symptoms. The health system will use the data in its return-to-work process and to identify possible donors for convalescent serum treatment. SVP/CIO Hans Keil, MBA, MA says the antibody test, which is not yet approved by the FDA, has been validated on 1,000 volunteers.
New York City increases its COVID-19 death count by 3,700 after including presumable coronavirus-related deaths that could not be confirmed because no tests were available. The city now reports more than 10,000 deaths.
Privacy and Security
Hartford Hospital (CT) announces that information about 2,400 patients was exposed in a February phishing attack in which hackers gained access to the email accounts of two employees. Several other healthcare organizations have reported similar attacks in recent months.
Other
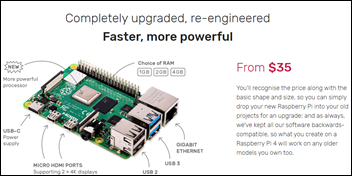
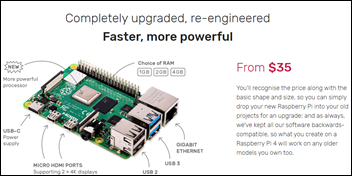
Sales of the stripped down Raspberry Pi computer, which starts at $35, set records as people teach themselves new skills at home and groups use them to create ventilator prototypes using hardware store components.
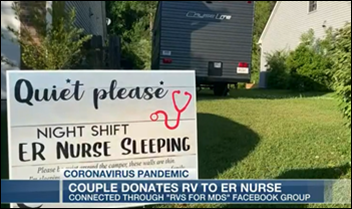
Doctors on the front lines of coronavirus are seeing their pay cut even as they are asked to risk infection, often without adequate PPE. This includes those whose compensation includes a significant component that is based on RVUs whose volume has been reduced with COVID-19 focus:
- A California ED doctor who was forced to buy her own N95 masks on Craigslist will see her pay cut by at least 25%.
- A New York ED doctor took a 10% pay cut and is expecting more.
- The income of some specialists has dropped by 80% due to lack of procedures.
- An urgent care company cut all salaries by 10% and confiscated all untaken PTO.
- New York doctors are being asked to take unpaid positions at COVID-19 hotspot hospitals owned by NYC Health + Hospitals, while the organization is recruiting temporary nurses $10,000 per week plus travel expenses.
- Envision Healthcare will cut the pay of its doctors who work in areas that have lower patient volumes.
- Alteon Health backed off some of its announced cuts after ProPublica reported its plans, but is still moving salaried doctors to hourly and then reducing their schedules.
- Atrius Health is withholding pay for doctors and nurses or cutting it by 20%.

In England, 99-year-old World War II veteran Captain Tom Moore, who hoped to raise $1,300 for the NHS’s coronavirus efforts by accepting donations for each 82-foot lap he completes around his garden using his walker, says he won’t stop even as donations have topped $3 million.

Rio de Janeiro illuminates the Christ the Redeemer statue in medical gear on Easter Sunday to honor medical workers around the world who are battling coronavirus. Meanwhile, Brazil’s president, Jair Bolsonaro, maintains that coronavirus is “a measly cold,” asserts that it’s a media hoax intended to erode his political support, and says the virus is leaving Brazil on its own accord.
Sponsor Updates
- Phynd will ingrate provider credentialing and privileges data from Symplr into Phynd 360, which allows organizations to publish provider data and deploy consumer provider search tools.
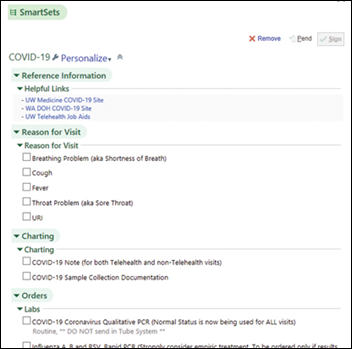
- TransformativeMed lists several health systems that are taking advantage of free use of its Cerner-integrated Core COVID-19 App for patient monitoring and data submission to health departments and the White House Coronavirus Task Force, among them UPMC, MedStar Health, UW Medicine, and Virginia Commonwealth University Health System.
- Use of the EClinicalWorks Healow telemedicine app exceeds 1.5 million daily minutes amid the COVID-19 pandemic.
- Montefiore St. Luke’s Cornwall Hospital (NY) and UPMC Western Maryland choose AHIMA’s compliant template library within Artifact Health’s mobile physician query platform.
- Nuance names Avaya a top growth partner and, for the third consecutive year, its top producing channel partner.
- Datica releases the latest edition of its 4×4 Health podcast, “ONC Final Rules on Information Blocking – Part 3.”
- Mental Health Center of Denver implements CareSignal’s COVID-19 Companion text messaging app.
- The Columbus business paper features the remote working strategies of CoverMyMeds.
- Diameter Health publishes a multi-part series on new ONC, CMS regulations.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.





















































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…