News 12/11/20
Top News
Amazon announces HealthLake, an API-driven, HIPAA-eligible, petabyte-scale AWS Cloud service for storing, transforming, querying, and analyzing health data.
It supports ingestion of FHIR-formatted data and provides natural language processing of unstructured data for querying and searching.
Early adopters include Cerner, Orion Health, and Konica Minolta.
Amazon estimates that a large hospital that stores 1 TB of patient data, runs 13,500 FHIR queries per hour, and applies NLP to 5 million characters of text would incur charges of $500 per month.
Reader Comments
From John Barleycorn: “Re: ActionOI. Vizient bought the workforce productivity benchmarking tool from IBM Watson Health a few months ago and has now cut off access to consulting firms. Just about every process improvement consulting firm – Huron, Deloitte, Accenture, Kaufman, etc. – used either ActionOI or Premier’s benchmarking package. I’m guessing that Vizient doesn’t want third-party firms profiting from their benchmarking and would rather sell the tool directly to hospitals.” Unverified. IBM Watson Health acquired Truven Health Analytics for $2.6 billion in April 2016, then in May 2020 announced a “partnership” in which it turfed ActionOI, CareDiscovery, and Market Expert to Vizient to offer clients a transition path to Vizient Operational Data Base.
HIStalk Announcements and Requests
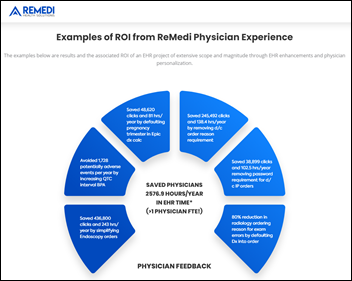
Welcome to new HIStalk Platinum Sponsor ReMedi Health Solutions. The Houston-based, clinically-driven healthcare IT advisory firm is committed to improving the future of healthcare. It provides EHR solutions that support enhanced patient care, efficient clinical workflows, and improved financial and operational performance for healthcare providers. The company believes in leading with empathy. Its deep knowledge of healthcare systems, workflows, and technology has helped it improve physician buy-in, patient care, and engagement significantly. ReMedi assists its clients with all aspects of EHR, from system selection and data migration to go-live, and provides valuable insights into trends and changes emerging from new regulations and industry best practices. The company was founded in 2017 by Texas native and physician informaticist Sonny Hyare, MD. Thanks to ReMedi Health Solutions for supporting HIStalk.
Unrelated to anything except maybe in a COVID Christmas stretch, but perhaps you need a current and future Zoom break. Mrs. HIStalk came running in with catalog that had come in the mail for her, gleefully describing how I would love it (the address label started with “For the master bathroom of:”) Thus began my two-hour, sophomorically giggling immersion into the warped world of Shinesty, which is what could result if writers for “The Onion” bought a manufacturer of bizarre Christmas pajamas, semi-profane underwear, and wild party suits. I’ve yet to decide whether I require “Weekend in Boca” Hammer pants or a Jesus-adorned “Santa is Fake News” sweater, but meanwhile, the catalog has earned a permanent spot within impulsive reach.
Listening: new from Toronto-based U.S. Girls, throwback, experimental pop with some disco thrown in by what is really just a single performer with some backers. Bands have usually ended up being ephemeral, fluid gatherings, so I guess I’m OK with one-off collaborations even as I wonder how the resulting musical diaspora can string together financially successful careers.
Webinars
December 15 (Tuesday) 1 ET. “Highlights from the 2021 CPT Code Set Update.” Sponsor: Intelligent Medical Objects. Presenters: June Bronnert, MSHI, RHIA, senior director of global clinical services, IMO; Shelly Jude, RHIA, RHIT, mapping manager, IMO. Top coding professionals will highlight the most important changes to the Current Procedural Terminology code set that take effect on January 1, including crucial additions, deletions, and revisions; how to communicate Official Coding Guidelines changes to the healthcare team; and a description of the impact that the code set update could have on practice.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Baxter International has reportedly offered to acquire medication management technology vendor Omnicell for more than $5 billion. OMCL share price jumped on the news, up 44% in the past year versus the Nasdaq’s 46% increase.
Consumer telehealth vendor Ro acquires Richmond-based Workpath, which offers an API-powered platform for dispatching workers to provide in-home blood draws and nurse visits.

Capacity management, access management, and analytics software vendor LeanTaaS raises $130 million in a Series D funding round, increasing its total to $250 million. CEO Mohan Giridharadas, MS, MBA founded the company in 2010 after 18 years at McKinsey & Company.
CitiusTech acquires healthcare management firm FluidEdge Consulting.
Sales
- Hi-Bridge HIE chooses NextGen Health Data hub as its HIE platform.
People

Novant Health promotes Angela Yochem, MS to EVP / chief transformation and digital officer, expanding her CDO/CTO role to include transformation and growth initiatives.
Announcements and Implementations
HIMSS launches its Office of Scientific Research, which will offer digital health vendors help with creating evidence of the effectiveness of their products and to share best practices.
Google announces Health Studies, a clinical trials recruitment app for Android devices. The first study involves COVID-19 related respiratory illnesses and is being conducted by Harvard Medical School and Boston Children’s Hospital.
Credit card services company Alliance Data donates $2 million to Nationwide Children’s Hospital (OH) for development of a database to support its community children’s program, allowing the hospital to track infant mortality, kindergarten readiness, high school graduation, teen pregnancy, obesity, suicide, preventive health, and child mortality.
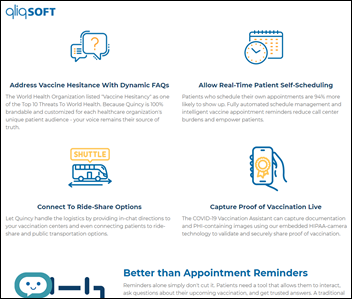
CPSI will offer its customers a COVID-19 Vaccination Assistant chatbot that was developed by QliqSoft, hoping to automate education and follow-up to overcome vaccine hesitancy.
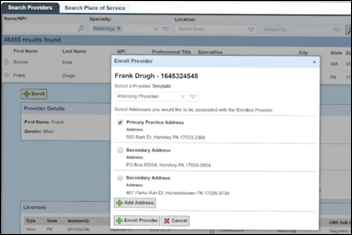
Phynd announces Epic App Orchard availability of Provider Data Connect, which allows Epic users to enroll providers and keep their data synchronized with Phynd Provider Data Management.

Banner Health is using Cerner integration with Xealth to allow providers to order digital content and services from a single location in Millennium.
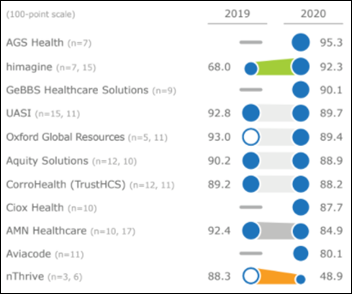
A KLAS report on outsourced coding finds high client satisfaction with Himagine and AGS Health, while internal changes and expansion have caused a 40-point drop in customer satisfaction for NThrive.

Runnymede Healthcare Centre goes live with Meditech Expanse following an eight-month implementation involving its relationship with Humber River Hospital, North America’s first fully digital hospital.

Scanwell Health, which sells direct-to-consumer home lab tests, lists its urinary tract infection kit for sale on Amazon. Consumers pay $15 for three tests (with free Prime shipping), read the test strip on the company’s app, then get same-day prescriptions via a $25 telehealth visit that is provided by Lemonaid Health. The urine test detects leukocytes and nitrites. The company is working with Lemonaid on a home blood test for COVID-19 antibodies.

Atropos Health launches itself with a “digital physician consult service” that mines EHR information for real-world evidence from similar patients to provide recommendations. The product uses Green Button technology that was developed at Stanford Medicine to form its Clinical Informatics Consult service.
Government and Politics
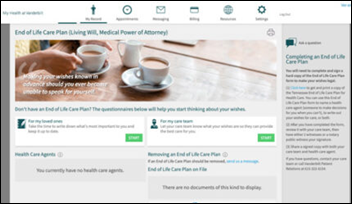
HHS OCR publishes draft changes to HIPAA, including:
- Patients would be allowed to take notes, photos, and videos of their records when inspecting them in person.
- The time for a covered entity to respond to a patient’s request for their records would be shortened from 30 days to 15, with the possibility of one 15-day extension.
- Patients could request a covered entity to send an electronic copy of their information to third parties.
- Covered entities would not be allowed to charge patients for viewing their information in person or online, but could charge patients their cost to make and mail paper copies. Copies made for third parties could be charged only to cover the labor involved.
- Covered entities would not be allowed to require patients to comply with unreasonable identity verification measures, such as requiring their records requests to be notarized, making them prove their identity in person when it could be done electronically, or requiring patients to use the covered entity’s online portal.
- Healthcare operations would be expanded to include care coordination and case management by health plans, at both the individual and population level.
- Covered entities would not need to decide which information is minimum necessary when the request comes from a provider or health plan for care coordination and case management.
- Covered entities would be allowed to disclose PHI to social services and community agencies for care coordination and case management.
- Permissible disclosure would be expanded in cases of substance abuse, serious mental illness, and emergencies.
- Providers would not be required to get a patient’s signed acknowledgment that they received a Notice of Privacy Practices.
COVID-19

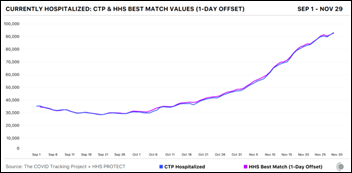
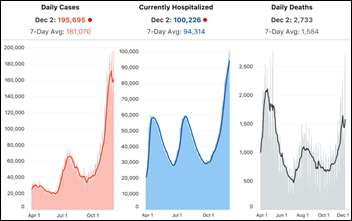
Wednesday’s state data showed another record day, with 210,000 new cases, 106,688 COVID-19 patients in hospital beds, and the highest-ever single day death count of 3,054.
China’s civil aviation authority recommends that airline flight attendants avoid COVID-19 exposure in onboard restrooms by wearing diapers.
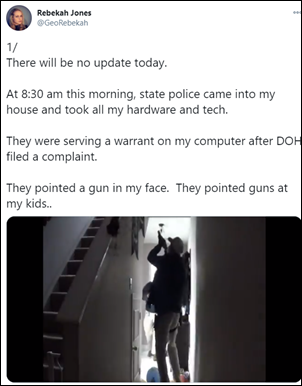
Florida state police raided the home of fired former state COVID-19 data scientist Rebekah Jones at gunpoint this week in investigating what the Department of Health says was unauthorized use of an emergency group text system, but Ars Technica finds that the system is not secured, uses a single username and password for all users, discloses those login credentials in a publicly searchable manual on DOH’s website, and will broadcast any message that is sent to a specific email address that is also listed in the manual.
Other
University of Vermont Health Network says its weeks-long, malware-caused downtime will cost it at least $63 million in lost revenue and additional expense.

The federal government’s cybersecurity agency advises users of GE Healthcare’s radiology equipment to change the widely published default password to protect their systems and networks from hackers, scoring the vulnerability at 9.8 on a scale of 10. A security firm also recommends restricting the Internet support ports to listen-only mode.

The Washington Post’s review of Amazon’s Halo Band concludes that not only is it “the most invasive tech we’ve ever tested” in using nude photos and microphone voice analysis to assess health status, it also “makes the absolute least use of it” in doing a better job sending data to Amazon than helping users get healthy. The paper warns that Amazon’s intention for the “half-baked product” is to capture user health information for training its algorithms to eventually disrupt medicine.
Plastic surgeons report an uptake in their Botox and cosmetic surgery business that could either be from pent-up demand, the perceived benefit of recovering unseen at home, or a “Zoom boom” in which housebound employees don’t like the way their webcam accents their chin, jaw, and neck on Zoom calls.
Sponsor Updates
- Healthcare Tech Outlook recognizes Lumeon as a Top 10 Surgery Solution Provider for its pathway engine that uses EHR data to personalize the care experience.
- Wolters Kluwer Health integrates Tabula Rasa Healthcare’s DoseMeRx with its Sentri7 Antimicrobial Stewardship solution.
- Meditech offers Expanse customers High Availability Snapshot to give them immediate access to patient data during unexpected downtimes.
- Saykara wins a Stratus Award for Kara, its AI-powered voice assistant that automates clinical charting.
Blog Posts
- COVID-19 Vaccine Distribution: The Next Hurdle for Hospitals (Everbridge)
- How Glytec’s EGMS Unlocks Quality Improvements in Glycemic Management (Glytec)
- COVID-19 is Exacerbating Challenges in Clinical Communication (Halo Health)
- Accelerating Healthcare Evolution: Cross-Industry Lessons (The HCI Group)
- As hiring freezes thaw, IT managers scurry to fill critical positions before year-end (HCTec)
- Shifting to Virtual Care in the COVID-19 Era: Analytics for Financial Success and an Optimized Patient Experience (Health Catalyst)
- How Does Telehealth Change the Provision of Care? (Optimum Healthcare IT)
- Measuring and Improving Patient Self-Efficacy and Informed Choice (Healthwise)
- Imprivata was in the news yesterday morning. Didn’t notice? Good. (Imprivata)
- Interoperability and COVID-19 in 2020 and Beyond (Infor)
- 5 Cybersecurity Threats to Healthcare During COVID-19 (InstaMed)
- Bed Visibility Proves Value at Two Levels: Q&A with Charley Larsen and Luke Smith (Central Logic)
- More than ever, we need powerful technology partnerships in healthcare (InterSystems)
- Creativity and caring: The secret sauce for a successful marketing team (Intelligent Medical Objects)
- For Legacy Healthcare Providers, The Retail Threat Keeps Getting Bigger (Loyale Healthcare)
- Building better virtual care experiences with the Epic App Orchard (Lumeon)
- Hackathon 2020 Drives Systemic Innovation at Medhost (Medhost)
- Managing a crisis with COVID-19 drive-thru testing at Lawrence General Hospital (Meditech)
- 6 Patient Engagement Tips to Utilize in the New Year (MWTherapy)
- Why patient identification is crucial for detecting adverse drug events (NextGate)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.












































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…