News 6/11/21
Top News
Healthcare AI vendor Iodine Software acquires clinical data improvement software and services company ChartWise Medical Systems, which is the #1 ranked CDI vendor in “Best in KLAS.”
Iodine acquired physician query platform vendor Artifact Health on May 25
HIStalk Announcements and Requests
Welcome to new HIStalk Platinum Sponsor Tegria. Tegria helps healthcare organizations of all sizes accelerate technological, clinical, and operational advances that enable people to live their healthiest lives. Based in Seattle with teams throughout the United States and internationally, Tegria is comprised of more than 3,000 strategists, technologists, service providers, and scientists dedicated to delivering value for customers. Founded by Providence, Tegria is committed to creating health for a better world. Thanks to Tegria for supporting HIStalk.
Here’s a Tegria intro video I found on YouTube.
HIStalk sponsors: it’s time to collect information for my HIMSS21 guide, which is a viewable / downloadable summary of sponsor booth location, conference activities, and contact information (example here). I will also list your company even if you aren’t exhibiting but will have someone available for onsite meetings. Submit your information to be included. Non-sponsors still have time to participate by signing up in the next few weeks.
Webinars
June 24 (Thursday) 2 ET: “Peer-to-Peer Panel: Creating a Better Healthcare Experience in the Post-Pandemic Era.” Sponsor: Avtex. Presenters: Mike Pietig, VP of healthcare, Avtex; Matt Durski, director of healthcare patient and member experience, Avtex; Patrick Tuttle, COO, Delta Dental of Kansas; Chad Thorpe, care ambassador, DispatchHealth. The live panel will review the findings of a May 2021 survey about which factors are most important to patients and members who are interacting with healthcare organizations. The panel will provide actionable strategies to improve patient and member engagement and retention, recover revenue, and implement solutions that reduce friction across multiple channels to prioritize care and outreach.
June 30 (Wednesday) 1 ET. “From quantity to quality: The new frontier for clinical data.” Sponsor: Intelligent Medical Objects. Presenters: Dale Sanders, chief strategy officer, IMO; John Lee, MD, CMIO, Allegheny Health Network. EHRs generate more healthcare data than ever, but that data is of low quality for secondary uses such as population health, precision medicine, and pandemic management, and its collection burdens clinicians as data entry clerks. The presenters will review ways to reduce clinician EHR burden; describe the importance of standardized, harmonious data; suggest why quality measures strategy needs to be changed; and make the case that clinical data collection as a whole should be re-evaluated.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Cerner lays off what it says is “hundreds” of employees. Unverified workers posted on Reddit:
- Speculation of the total number let go ranges from 1,000 to 4,000. UPDATE: A Cerner spokesperson says the actual number is 500 employees of its 26,000.
- Some of those involved say they worked on the company’s DoD and VA projects, and at least one employee who claims to have been affected says their developer jobs are being sent offshore.
- One says that shared services engineering had a 22% workforce reduction, while another said that 15% of Healthe are gone.
- Others said that several VPs were let go.
- Several say that Cerner fired new hires in its development and technical academies.
- Some speculate that the layoffs are intended to boost profit to make a rumored acquisition of the company more attractive.
Population health management software vendor TCS Healthcare Technologies acquires DataSmart Solutions, which sells predictive risk analytics software.
Transcarent raises $58 million in a Series B funding round, increasing its total to $98 million. Its CEO is former Livongo founder, chairman, and CEO Glen Tullman.
Patient privacy technology vendor Datavant will merge with Ciox Health, creating a patient data exchange business operating under the Datavant name that the companies say will generate $700 million in revenue and a valuation of $7 billion. Ciox CEO Pete McCabe will lead the business as CEO.
Healthcare business intelligence vendor Definitive Healthcare files IPO documents with the SEC.
Amazon has signed up several companies as customers of its Amazon Care telehealth service. The company is expanding the virtual portion of the service to all 50 states this summer, eventually followed by national availability of its mobile medic visits and two-hour prescription delivery.

Several insurers, Cleveland Clinic, IBM, and Sentara Healthcare invest in newly launched Avaneer Health, with JPMorgan health executive Stuart Hanson, MBA joining as CEO. The announcement describes the company with little detail:
Driven by its vision for a more productive and people-centered industry, Avaneer Health is building an inclusive network, breakthrough infrastructure and solutions to unlock healthcare’s potential. The groundbreaking company enters the market with an expert team of change agents; investment from top industry players; and a technology backbone designed to support a vast array of platforms for greater applicability and use in reducing administrative costs, accelerating care and improving the experience for people and their families.
Sales
- The United Kingdom Ministry of Defense will use InterSystems HealthShare to normalize, aggregate, and de-duplicate data into a longitudinal unified care record for the Defense Medical Services.
People

Rodrigo Martinez, MD (ENT and Sleep Specialists) joins PerfectServe in the newly created position of chief medical officer.

FOLX Health hires Dana Clayton (Optum) as VP of operations.
Announcements and Implementations
Healthcare consumer insight vendor Carrot Health will incorporate social determinants of health data from LexisNexis Risk Solutions into its predictive models.
UK-based Nuffield Health uses Lumeon’s Care Journey Orchestration Platform to scale its COVID-19 rehabilitation program across 40 regional centers.
Meditech announces its upcoming integration with IOS 15’s enhancements to Apple Health, in which providers can launch a web-based dashboard within Expanse to view the information that a patient has shared with them.
Other
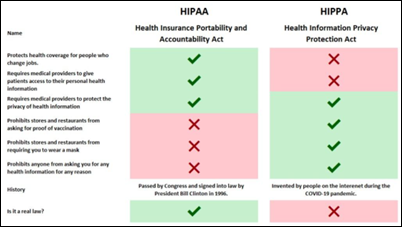
This is a savagely witty comparison of the real law (HIPAA) versus the imaginary one (HIPPA) that clueless folks use as justification for not doing something. The graphic is making its way around the Internet, although I don’t know the original source.
Sponsor Updates
- First Databank joins the National Council for Prescription Drug Programs Elite Partner Program.
- CTHealthLink, part of the Konza National Network, will explore opportunities to incorporate technologies developed by the UConn School of Nursing’s Analytics and Information Management Solutions.
Blog Posts
- Making the Complex Simple with a Data Analytics Solution for Investigating Real-time Medical Device Data (Part 2 of 2) (Capsule)
- A Year in Review for Healthcare – A Fireside Chat with Microsoft Health’s Chief Nursing Information Officer, Kathleen McGrow (Get-to-Market Health)
- Consumer Devices Are Rapidly Improving. What Does It Mean for Healthcare? (Twistle)
- Building a Smart Room: What Hospitals Should Consider (GetWellNetwork)
- Enhancing Diabetes Care with Technology: Key Strategies from Emory University and Grady Health System (Glytec)
- Technology to Reduce Nursing Burnout (Halo Health)
- How to Use HCC Analytics to Improve Provider Education and Point-of-Care HCC Capture (RCxRules)
- Three Keys to a Successful Data Governance Strategy (Health Catalyst)
- The role of reference data in your telehealth initiatives (Wolters Kluwer Health)
- Remote Work: Three Ways to Be More Present (Impact Advisors)
- 4 key differences between consumer and enterprise biometrics (Part 2) (Imprivata)
- Virtual Support for Virtual Implementations (Optimum Healthcare IT)
- Beyond Skin Deep: How Anatomic Pathology Software Providers Better Data to Save Lives (InterSystems)
- Getting Patients Back on Track: Wellness Visits & Preventative Care (Intrado)
- The evolving EHR: Workflow improvements for today’s clinician (Intelligent Medical Objects)
- Healthcare & SEO: Best Practices for 2021 (Kyruus)
- Beware of Regulations Strengthening Consumer Access to Personal Health Information (Medhost)
- Don’t Get Lost in the Numbers: Making Home Health Data Actionable (Meditech)
- Physical Therapy Marketing Advice: What Are the Pros Saying? (MWTherapy)
- Reimagining Consumer Empowerment in Healthcare Starts with Digital Identity (NextGate)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.














































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…