There was a recent report pointing to increased Medicare costs when patients returned to traditional Medicare, of course assuming that…
News 8/19/20
Top News
Interoperability platform vendor Bridge Connector raises $25.5 million in a Series B funding round, increasing its total to $45 million.
The Nashville-based company will use the funding to continue the rollout of its new Destination integration service. It says it is on track to boost growth by 1,000% in 2020.
Reader Comments
From Cam Sandford: “Re: telemedicine. I think the pushback against online classes offers a value warning.” Students who are paying megabucks for college tuition are not happy at being taught over the equivalent of Skype at full price, even though their degrees will presumably be worth the same in the end. The convenience factor isn’t convincing students and their parents that trading the campus experience for home learning is a good deal. The biggest risk to telemedicine is that patients often still have to go somewhere as a result –pharmacy, lab, x-ray facility, ED, or specialist – and that cancels out much of their overall convenience. I also wonder how patient satisfaction fared in the telemedicine tsunami, especially when segmented into the “I just need a prescription” kind versus complex, ongoing patient management. Most of us don’t conduct our business virtually with lawyers, accountants, and financial advisors and we might have the same reluctance to turn our medical issues over to the flickering image on a video screen, especially if we are just assigned some random, available doctor that we don’t know, can’t contact for follow-up questions or concerns, and will never see again. It would also be interesting to compare the experience, credentials, and outcomes of doctors who are willing to sell telemedicine time to those who aren’t, just like you don’t see top-tier actors and athletes hawking custom video birthday greetings on Cameo.
Webinars
August 19 (Wednesday) 1:00 ET. “A New Approach to Normalizing Data.” Sponsor: Intelligent Medical Objects. Presenters: Rajiv Haravu, senior product manager, IMO; Denise Stoermer, product manager, IMO. Healthcare organizations manage an ever-increasing abundance of information from multiple systems, but problems with quality, accuracy, and completeness can make analysis unreliable for quality improvement and population health initiatives. The presenters will describe how IMO Precision Normalize improves clinical, quality, and financial decision-making by standardizing inconsistent diagnosis, procedure, medication, and lab data from diverse systems into common, clinically validated terminology.
September 3 (Thursday) 2:00 ET. “How Does A Global Pandemic Reshape Health IT? A Panel Discussion.” Sponsor: Intelligent Medical Objects. Presenters: Rob Wallace, chief product officer, IMO; Andrew S. Kanter, MD, MPH, chief medical officer, IMO; Lori Kevin, VP of enterprise IT and security, IMO; Sahas Subramanian, MCA, enterprise architect, IMO. As COVID-19 continues to spread, regulation changes, code system updates, and an increased reliance on technology are making it hard to stay on top of the many ways the pandemic is altering health IT. What’s more, we’re confronting challenges that rely heavily on technological solutions – like accurate reporting tools or telehealth adaptations – and we need those solutions now. The panel of subject matter experts across the enterprise will share insights on how the global pandemic is reshaping the health IT world.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Perhaps this is telemedicine’s next acquisition, Medical cannabis telemedicine provider PrestoDoctor expands to Illinois after success in other states in selling medical marijuana cards for $50 to $200, depending on the state. It is fascinating to see how many buzzy startups sell nothing but rubber-stamped doctor prescriptions delivered impersonally online, adding minimal value and contributing little to drug safety and appropriate use by at least occasionally prescribing whatever the patient wants to keep the patient and their employer happy.
Sales
- Michigan Medicine chooses Sectra for enterprise imaging.
People


CloudWave promotes Erik Littlejohn, MBA to president/COO and Joseph Badziong, MBA to CFO.

Ciox Health hires Nick Giannasi, PhD (Change Healthcare) as chief product officer.

Todd Johnson (GetWellNetwork) joins Avia as SVP/practice leader.

Nordic hires Jeff Buss, MS, MBA (EY) as CIO.
Announcements and Implementations
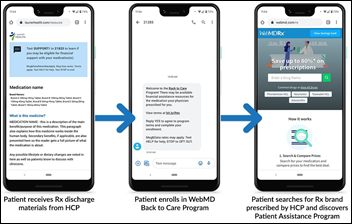
WebMD and Krames launch WebMD Back to Care, which connects patients with available prescription payment assistance programs. The information will be included in end-of-visit patient education materials provided by Krames, which joined WebMD as part of its StayWell Company acquisition from drug maker Merck in March 2020.
Virginia Cardiovascular Specialists deploys PatientKeeper for reviewing patient information and capturing professional charges on mobile devices.
3M-owned MModal says that 150 healthcare organizations are using its virtual assistant technology that captures the doctor-patient conversation to automatically document the encounter.
COVID-19

FDA warns labs and providers that Thermo Fisher’s TaqPath COVID-19 test kit can deliver false positive results unless labs apply software updates and follow the company’s instructions for vortexing and centrifugation.

University of North Carolina at Chapel Hill moves undergraduate classes online just one week after the start of in-person classes. The university reported several COVID-19 breakouts in communal living areas and a 13.6% test positivity rate that quickly filled its isolation dorm. UNC had ignored CDC’s recommendations, declined to follow the county health department’s recommendation to delay in-person classes for five weeks, and didn’t tell faculty members about the health department’s warning that it should not bring students back to campus. The independent student newspaper published an editorial about the clusters of infection under the headline “UNC has a cluster****” on its hands,” except they used letters instead of asterisks in describing how the university should have know that students would immediately start behaving recklessly at parties even before last Monday’s class start. Football practice will continue, however, and a home game is scheduled for UNC’s largely closed campus on September 12.
North Carolina’s health department says Monday’s case count was lower than expected because a commercial lab was late in sending its data file, the second week in a row where testing numbers were wrong due to lab data problems.
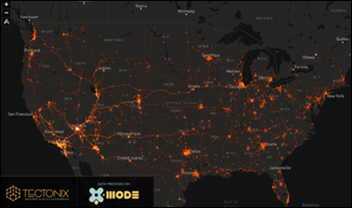
A ProPublica report says that cellphone tracking data shows that visitors to Las Vegas casinos, which re-opened on June 4, are likely spreading coronavirus to communities all over the country. Travel-related transmission cannot be easily detected by contact tracing, which is local rather than national in nature.
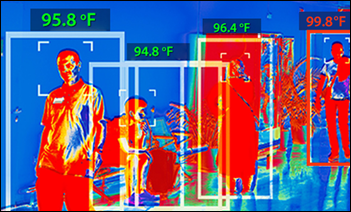
Three New Jersey hospitals implement thermal scanning to screen patients, visitors, and employees as they enter the premises, ignoring WHO’s conclusion that such scanners – which were never intended for medical use — do little except provide a false sense of security since many COVID-infected people are free of symptoms.
Other
Ohio-based contract Epic analyst Gurnee “GG” Green will be featured in the Democratic National Convention this week, explaining how her custom clothing boutique that she opened in December 2019 has struggled due to COVID-19.

The bond rater of Wise Health System (TX) says that one reason the health system’s margin has slipped is the cost of replacing Cerner with Allscripts, which in addition to staffing expense, created $12 million worth of revenue cycle inefficiency. It notes, however, that Wise Health Surgical Hospital improved its revenue cycle performance in 2019 following the EHR implementation.
Sponsor Updates

- The Ettain Group donates laptops to the Dottie Rose Foundation in support of its STEM and family-assistance efforts.
- Clinical Architecture will present during Logica’s Summer 2020 Virtual Meeting August 18-20.
- Everbridge wins The Help Desk Institute’s 2020 Best Customer Experience Award.
Blog Posts
- CDC advice for managing a staffing shortage – and how Ability can help (Ability Network)
- Three Simple Steps to Reducing Accounts Receivable (AdvancedMD)
- The 21st Century Cures Act: Deadline Approaching November 1 (Bluetree)
- Navigating the Next Phase of Telehealth Adoption (Bright.md)
- 3 Common Misconceptions About Business Associate Agreements (Datica)
- HAP’s Experience Managing Members During the COVID-19 Surge (CarePort)
- Mental Health Risks for COVID-19 Frontline Healthcare Workers (Optimum Healthcare IT)
- Price Transparency 2021 – Are You Ready? (Health Triangle)
- Addressing Physician Burnout via EHR Inboxes and Patient Message Management (ChartLogic)
- What You Need to Know About the CMS Interoperability & Patient Access Rules (Collective Medical)
- Rethinking Data Protection with Air-Gapped, Consistent Backups in the Cloud (CloudWave)
- Five Ways Providers Can Help Mitigate Telehealth Access Challenges (CoverMyMeds)
- 7 Keys to Better EHR Usability (EClinicalWorks)
- Home Care’s Increased Role During the COVID-19 Pandemic (Ensocare)
- Helping Hospitals Get Back on Their Feet with Advanced Analytics (EPSi)
- McKnight’s Power Panel EBook – Succeeding Despite the 2020 Pandemic (ESolutions)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




You raise interesting points re: the perceived value of telehealth. While I personally agree there is less value in virtual engagement with a random third-party provider via companies like Amwell, I am absolutely willing to pay more for virtual engagement with my PCP when it suits me. Those without a PCP may also see value in the former. Use will undoubtedly decline some post-pandemic but providers would be foolish not to invest in telehealth given new consumer expectations and the ongoing need for more convenient care delivery options – not to mention the digital safety net it will serve as during future public health fallouts.
That is certainly how most traditional healthcare providers think about it. Here’s how your insurance company thinks about it. You know that nurse line that they run where you can call in and ask questions? What if the people on that line could write prescriptions, order and interpret labs, etc.? What percentage of doctors office visits could they cover? Rough guess would be 1/3 of your typical PCP visits. How much less could the total cost be for that office visit? Maybe it is 60 percent of the in person cost, more in high rent areas or areas with limited physician supply. When an insurance company is required to spend 80 percent of revenue on claims and they optimistically have a margin of 5 percent, it is a no brainer for them to try as hard as possible to make their telehealth solution work for their consumers. I agree it doesn’t make sense for traditional fee for service health systems to be using telehealth. Instead it is something that cuts the traditional health system out of the relationship because they are too expensive or their service is too bad.
Which makes the idea of health systems buying telehealth services sound strange to analysts. Why would health systems want to fund their competitors unless they have no hope of putting the telehealth cat back in the bag?
Why would providers move to telehealth you ask?
Simple
If they are moving to taking on more risk, potentially capitation they’ll want to lower utilization costs. Telehealth can, if done correctly, assist with that.
I would rather some dumb startup provide access to marijuana cards, rogaine, birth control, contact lenses, etc. than have to wait in line behind those people in the doctor’s office. Those are mostly just doctor employment programs anyway which they don’t need.
Spoke with MD yesterday, they’re doing pot over the phone now. Great job telehealth… you really saved the world this time.
Meanwhile, back at the facility, kidney patients are bearing a covid burden on top of the mortality rate associated with dialysis…
Point: mobile works, big brick things with windows that don’t open don’t. Disclaimer: I’m talking about patient healthcare, not funding a better grasp on a sinking anchor.