EPtalk by Dr. Jayne 11/11/21
I had dinner with one of my friends from residency tonight. She’s considering leaving practice even though she’s not even 50. She had two unvaccinated patients die from COVID this week, one of whom was only 46 years old and who died after being in the intensive care unit and on a ventilator for over two months. Her late patient left behind several children, and apparently their father spent the last several days harassing my colleague because she had refused to treat the patient with ivermectin. The harassment included threatening comments and a visit to my friend’s house, resulting in a call to the police and my friend bundling her own children off to their grandparents’ just in case. Physicians have been fighting this pandemic for more than a year and a half and they certainly didn’t sign up for what she experienced.
On top of that, her partner quit and the health system she works for has been unable to hire a replacement who is willing to join a rural practice, leaving her to care for more than 6,000 patients on her own. She has also developed a severe skin reaction from the soap and sanitizer used in the office, resulting in a worker’s compensation claim after multiple product changes failed to yield results. She’s had to miss work due to numerous physician visits, including second and third opinions from dermatologists at the local medical schools. Every time she takes off for a physician visit, it negatively impacts her office productivity, and the medical group’s newly appointed administrator asked her why she can’t schedule her visits after hours. As she was telling me the story, I wondered if the administrator had ever been a patient or caregiver, because that’s just an asinine suggestion.
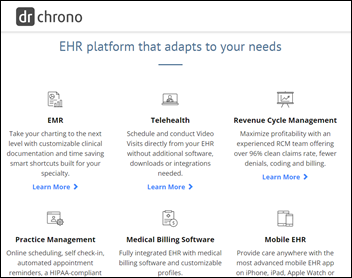
She had a lot of questions about telehealth and whether that might be an option for her if she isn’t able to find a solution to her allergic skin reactions. Her only experience with telehealth was during the height of the pandemic, when the health system encouraged physicians to embrace virtual visits because patients didn’t want to come in. However, in her particular community, many patients didn’t think COVID-19 was a big deal and thought that dealing with a computer was a bigger nuisance than risking infection, so telehealth never really took off. From a technology standpoint, they were using a solution that was completely cobbled together and had no integration with their EHR, so I encouraged her not to judge her options based on that experience.
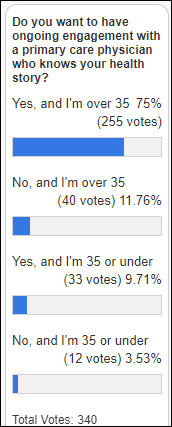
We talked about some trends in telehealth, including insurance plans that have a virtual-first focus. I would propose that such plans would be most effective if continuity could be preserved, either with the same care team providing both in-person and virtual care, or if dedicated virtualists had full access to the patient’s medical records. There are concerns about physicians providing virtual-only care as far as not being able to perform a physical exam. The new plans are designed to have networks of in-person physicians that can perform hands-on services when required, and who can coordinate with the virtual physicians. Although payer-sponsored plans might have their own patient records, they might have difficulty coordinating when patients receive services from non-network physicians or other care providers. Some of the plans have high deductibles for in-person care, which may serve as a deterrent. Additionally, they may not be compliant with the Affordable Care Act.
We also talked about the challenges of practicing telehealth, including technology issues. A recent piece in JAMA Network Open looked at factors influencing whether patients and physicians were able to successfully complete telehealth visits. The authors looked at over 137,000 video visits and found an overall success rate of 90%. Patient factors were “more systematically associated with successful completion of video visits” where “clinician comfort with technology was associated with successful video visits or conversion to telephone visits.” Certain factors were associated with conversion to telephone visits, including lower clinician comfort with technology, greater patient age, lower patient socioeconomic status (including low availability of high-speed internet), and racial/ethnic minority status.
The study has some limitations, including having been conducted at the height of the COVID-19 pandemic when most of us were still getting used to the idea of video visits and many providers were using substandard technology platforms to try to connect with patients. Visits at that time were often sporadic and urgent, and there was little lead time to help patients with technology or their comfort level with video encounters. The study also was conducted in the Midwest and at a single healthcare organization. Longer duration studies with a broader cross section of patients would be beneficial.
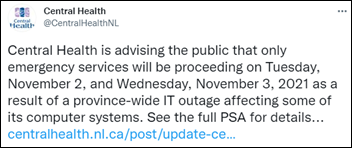
Our conversation crossed into a lot of different elements of practice, and she was interested to hear about my recent experiences in EHR training. We’re both veterans of multiple EHR conversions and implementations, and she asked if I had seen the story about the US Department of Veterans Affairs being ordered to pay $160 million to clinicians for extra work hours spent updating EHR data. I hadn’t seen it until she mentioned it, but the short version is that 3,200 nurse practitioners and physician assistants who were employed by the VA at the time worked overtime doing various EHR functions and weren’t compensated appropriately. The court ruled that employees should have had received overtime pay any time they worked more than eight hours in a day. In the class action suit, each member will receive about $50,000 in compensation.
The last thing we talked about as our bottle of pinot noir became depleted was an article that looked at whether physicians could accurately predict the out-of-pocket costs for medications they were prescribing. The authors found that only 21% of physicians could do so, which sounds like what I might expect given the craziness of medication pricing and the challenges in figuring out various formulary coverage, deductibles, co-pays, and annual caps. We’ve both used EHRs that were supposed to display formulary and eligibility data in a way that should help physicians figure this out, but have found that none of them were particularly effective, especially since different payers use different formulary levels that resulted in confusing EHR displays and data that just didn’t make sense.
The evening ended with a discussion of her children and their career plans and the fact that she’s completely baffled her children want to pursue careers in medicine despite her obvious dissatisfaction with it and eagerness to leave it. They’re still relatively young, in middle and early high school, so of course things can change. Given the way things are now, I know quite a few physicians who wouldn’t choose the career again, or if they did, would choose a different specialty. It’s a sad commentary on what healthcare has become for a lot of physicians.
If you had it to do over again, would you still choose healthcare? Leave a comment or email me.

Email Dr. Jayne.











































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…