News 12/10/21
Top News
Ambient clinical documentation vendor Robin raises $50 million in a Series B funding round.
The company says its physician users save 90 minutes per day. It guarantees its work in defending any audits that result.
Co-founder Emilio Galan, MD, MS founded healthcare transparency vendor HonestHealth, while co-founder Noah Auerhahn started and sold shopping portal Extrabux.
Reader Comments
From HisTalk Fan: “Re: Cerner. Sharp HealthCare and Shriners are leaving for Epic.” Verified for Sharp, not yet verified for Shriners (but likely), according to my contacts. Sharp is now an Epic enterprise customer for both the health system and its managed care business. It had been a Cerner user since 1995 and extended its Cerner contract in early 2019 for another eight years.
From Dr. J: “Re: AirStrip and Nant forming Adjuvare. Patrick Soon-Shiong owns AirStrip since recapitalizing it when Sequoia Capital dumped its holdings.” Thanks. The SEC filing is here.
HIStalk Announcements and Requests

From Patti: “Re: No Surprises Act. Seems to place a heavy burden on provider administrative staff.” CMS hasn’t posted the transcript of Wednesday’s call as I write this, but some of the elements of the act – which takes effect January 1, 2022 – require providers to: (a) not balance-bill for out-of-network emergency services or non-emergency services unless notice and consent is given; (b) provide uninsured or self-pay patients with good-faith cost estimates in advance; (c) accept plan payments for 90 days after a payer-provider contract ends; and (d) submit provider directory information to health plans at the beginning and end of the agreement and when changes are made and reimburse patients who are billed out-of-network rates because of a directory error. The act also establishes an arbitration procedure for provider-plan disputes (taking patients out of the back-and-forth arguing) and authorizes HHS to establish or improve an all-payer claims database. Providers also need to understand their state-specific billing rules and how they overlap with the No Surprises Act. Perhaps someone can elaborate on the practical impact to providers since the act takes effect in just three weeks.
Webinars
December 14 (Tuesday) 1 ET. “Using Cloud to Boost AI and Enterprise Imaging.” Sponsor: CloudWave. Presenters: Larry Sitka, MS, VP/CSIO of enterprise applications, Canon Medical Informatics; Jacob Wheeler, MBA, senior product manager, CloudWave. Enterprise imaging has remained a holdout of data center complexity despite the benefits the cloud offers. The presenters will discuss innovative ways to reduce complexity and lead with disruptive technology using AI, enterprise imaging, and the cloud.
December 15 (Wednesday) 1 ET. “Improve Efficiency, Reduce Burnout: Leveraging Smart Clinical Communications.” Sponsor: Spok. Presenters: Matt Mesnik, MD, chief medical officer, Spok; Kiley Black, MSN, APRN, director of clinical innovation, Spok. The presenters will identify the technologies that most often contribute to clinician burnout, then explain how improving common clinical workflows can help care teams collaborate better and focus on what they do best—taking care of patients. They will describe how a clinical communication and collaboration platform can automate clinical consults and code calls to alleviate burnout.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Online mental health services vendor Cerebral raises $300 million in a Series C funding round, increasing its total to $462 million. The company focuses on medications, referring to its providers as “prescribers” and mailing medications to patient homes. Founder Kyle Robertson was an Accenture consultant and founded a college startup website.
Bloomberg reports that the private equity owner of healthcare analytics vendor Cotiviti is considering selling the company for over $15 billion. Veritas Capital acquired the company in a $4.9 billion take-private deal in 2018. The private equity firm also acquired GE Healthcare’s value-based care business and invested in Truven Health Analytics.
Israel will fund a $18 million digital health innovation program that will help providers implement anonymized data-sharing with healthcare startups for research, hoping to develop an international data sharing standard such as the US-based SEER for cancer statistics.
Industrial IoT security platform vendor Claroty will use $400 million in new Series E funding to acquire healthcare IoT vendor Medigate. Medigate co-founder and CEO Jonathan Langer served in the Israel Defense Forces through 2016.
Included Health, formerly Grand Rounds and Doctor on Demand, is reportedly planning an IPO for the first half of 2022.
Sales
- Creative Solutions in Healthcare, the largest skill nursing operator in Texas, deploys the CareSafely quality, safety, and compliance software platform in its 91 facilities.
People

Anne Donovan, MBA (Zelis) joins Wolters Kluwer Health as VP/GM of its Health Language business.

Verisys hires Joe Alberta (Optum) as chief revenue officer.


PatientBond hires Jeff Bohmer, MD (Northwestern Medicine Central DuPage Hospital) as chief medical officer and Mark Spranca, PhD (Mathematica) as chief strategy officer.

Industry long-timer Brian Graves (Optum) joins surgical care team coordination solutions provider RelayOne as chief revenue officer.

Vu Van, MBA (Livongo) joins Transcarent as VP of health systems.

Orchestrate Healthcare hires Eric Boone (InfoBionic) as VP of sales, southeast.
Announcements and Implementations
Google is working with WHO to develop an open source software developer kit for developing FHIR-powered mobile solutions for Android. One of the apps is EmCare, a clinical decision support system that is based on WHO SMART Guidelines.

Amazon’s Comprehend Medical natural language processing service adds support for SNOMED-CT and reduces the charge for using its API by up to 90%.
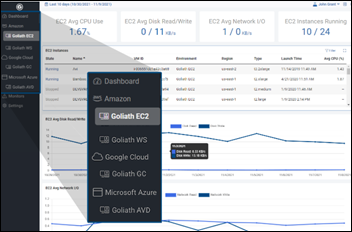
Goliath Technologies launches Multi-Cloud Monitoring, which provides a unified view of AWS EC2 and Workspaces, Microsoft Azure, Citrix Cloud, and Google Cloud for troubleshooting performance, availability, and end-user experience.
Asynchronous telehealth platform vendor Bright.md announces Navigate, in which patients enter their primary symptom and the app presents the appropriate next step – on-demand asynchronous visit, appointment scheduling, or urgent care — based on health system configuration.
Government and Politics
CDC says its questionably accurate vaccination rates among US seniors – which at times has showed more people in a given age group vaccinated than exist – overestimates first doses and underestimates follow-up doses because it can’t always identify people who get their shots from different providers or states. CDC says that providers are required to de-identify their data, which limits the organization’s ability to match vaccinations to recipients.
Other
Memorial Sloan Kettering paid $1.4 million in severance to three former executives in 2020, with the largest payment of $700,000 going to former CIO Pat Skarulis.
A study of Epic-using ambulatory care clinicians finds that EHR clinician time and after-hours work dropped early in the pandemic, but had recovered by July 2020. Patient messages increased 157% of the pre-pandemic average, with each message requiring more than two minutes of additional clinician EHR time. The authors speculate that increased messaging was caused by the increased use of patient portals, leading them to conclude that higher message volume will persist.
Epic CEO Judy Faulkner says in a “Hey Judy” EpicShare story that she decided to build an Epic campus when the company hit 300 employees, estimating that a safe bet was a capacity of 10 times the headcount then (3,000 employees). She and Carl Dvorak visited the Microsoft campus where her son worked and then found a Verona corn field that she thought was about the same size, only to find later that the Microsoft campus was 29 acres and the Verona property was 350 acres because “we had no ability whatsoever to correctly judge land mass.” The campus has since expanded to 1,200 acres for its 10,000 employees.
Sponsor Updates
- Meditech celebrates 30 years of supporting healthcare in the UK.
- Healthcare IT Leaders adds multilingual support from Voyce to its COVID-19 contact tracing capabilities.
- The Meditech Podcast, “How genomics will revolutionize healthcare in the next decade,” features First Databank Director of Product Management Anna Dover.
- LexisNexis publishes a case study, “Lehigh Valley Health Network Innovates Strategic Planning in Healthcare with LexisNexis MarketView.”
- Lumeon’s COVID-19 remote home monitoring solution wins a Silver Best in Biz Award in the Best New Product of the Year category.
- DCH Health System (AL), which recently went live with Meditech Expanse, has been named to CHIME’s Digital Health Most Wired list.
Blog Posts
- How a Continuous SOC Can Help Healthcare Facilities Avoid Data Loss (Fortified Health Security)
- The Year of Employee Burnout & How to Address It (Halo Health)
- 5 Things to Consider When Evaluating a Community Connect Host (Healthcare Triangle)
- Three Crucial Mindset Shifts to Reach Peak Financial Healthcare Management (Health Catalyst)
- What Value Does an Epic Service Desk Bring? (Impact Advisors)
- The complexity of COVID-19 variant data (Intelligent Medical Objects)
- Five Steps to a Successful Clinical IT Implementation – Pt 1 (Medhost)
- How to Attract New Talent at Your PT Practice (MWTherapy)
- Vaccine Administration – a year later and still inefficient (NextGate)
- Combining the advantages of close-talk and far-talk speech recognition (Nuance)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.







































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…