Guillaume de Zwirek is founder and CEO of Artera of Santa Barbara, CA.

Tell me about yourself and the company.
I founded Artera seven years ago. We recently rebranded from Well Health. I had never been in healthcare before I founded the company. I was going through a personal experience with cardiac issues and had a really frustrating time interacting with all of my care providers outside of the four walls of the hospital. The question kept coming back to me — why is healthcare not amazing at customer service?
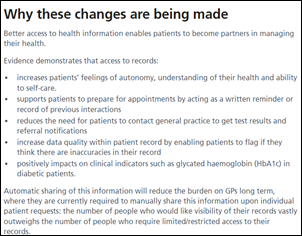
I founded this company with a simple mission, which is to make healthcare the very best industry when it comes to customer service. I came into it with a lot of naiveté and ignorance. We spent seven years thinking about how to build an effective patient communication system for hospitals that is open; that allows every vendor to deliver its interactions through that platform; and that allows health systems to control the flow, rhythm, and prioritization of their communication so they can have an effective and convenient relationship with their patients.
Is it harder in healthcare where health systems have a large volume of customers but see them infrequently and often involuntarily?
Healthcare is complicated for good reason. It’s protected information, and we want to be sensitive to the privacy of patients and their medical records. There are a lot of stakeholders, even within the hospital. You have your primary care doctor, specialists, labs, pharmacies, clinical trials organizations, payers, and employers. Those parties are are all competing at some point in time for the patient’s attention.
There isn’t a library of five care journeys. This isn’t like an airline, where people are only booking one-way flights, return flights, or getting connecting legs. An infinite number of scenarios could happen for a patient, which makes this so challenging,. Then you layer in all of the ecosystem of vendors who are all trying to help make that experience smooth. When you think about streamlining that communication, that’s a lot of people to consider.
Health systems will have different ways of thinking about the priorities. That’s what we’re trying to solve. How do you consider all of those voices; bring that and surface that to the hospital in a way that is easy to manage, control, and manipulate; add and remove players; and then have that experience feel completely seamless to the patient? We are largely SMS, but the dream is that you are on your phone, your doctor is saved as a contact, you have an issue, you send a text, you get a response back. Whether that response is automated, a human being, a PA that reports into a physician, I’m indifferent to that as long as we get the right answer to the patient every time in the medium that is most effective to them.
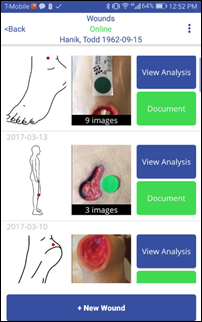
If I can just share a quick story, this came to life for me last week in a wonderful way. I got a call from one of our customers with a story. This customer, their population, is rather elderly. They skew probably 70-plus. They had a patient who had a fall and they were wearing an Apple watch that had their emergency contact saved as that hospital. When the new Apple Watch detects a fall, it will text your emergency contact. That text hit our system, a staff member saw it right away, and they got in contact with the family and arranged emergency services for that patient. There are so many scenarios like this one that we haven’t considered yet. That’s what makes this complicated, the infinite number of scenarios and players.
Amazon has set up its own personal monitoring program that is linked to Echo devices. Could a user’s preferred health system replace a third-party call center as a local first step for medical issues?
I had never thought of that, and I think that’s a very logical assumption. My wife works at Google and she just got a pamphlet in the mail for a 24/7 urgent care service where you can jump on the phone, and within two minutes, somebody’s on the other end triaging you. That’s actually driven by the payer, circumventing the health system that she would normally go to. The same thing could apply in this Apple example or Amazon with Echo.
It will be interesting to see where they start. If you can be that first point of contact, you have tremendous influence over where the care gets delivered. If that care is acute, if it’s a specialist type of visit, that’s where the money is made. It could be a big threat to hospitals.
My personal opinion is that competition is great and we should all challenge ourselves to do better. At my core, I believe in the physician-patient relationship. I believe that to be thoughtful and proactive about your care, you have to have a relationship with your PCP. You need to feel like you’re disappointing somebody and somebody has your back if you don’t adhere to directions.
I’ve been using the gym more regularly for three months. I went to see my PCP and he said, great news, your cholesterol has dropped 50 points, what changed? I said that I had started going to the gym. Now I’ve kept it going and I think of him every time. Maybe that’s just me, but I believe that when people have a great relationship with their PCP, they never leave, kind of like the dentist. That’s who our energy is going to be focused on serving,
How does a health system define their customer when people move around, change insurers that take them into or out of network, and perhaps don’t want to hear from providers until they have an acute need?
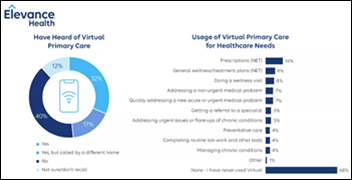
There’s a whole market around that with population health. Many companies are tackling who to reach out to and onboard, how to bring panels into the system. That’s why the relationship outside of that visit is so, so important. I texted my PCP to see if I could get the third booster, for example. There are so many opportunities for the physician to engage with you, or for you to engage with them, outside of the point of care.
When you think about the younger generation, if you can create that relationship with the parents, many children will follow in their parents’ footsteps. I hope that there doesn’t have to be an art of engaging this lost population who never got care. COVID may make that necessary for us to catch up. I hope that we can build those types of relationships from birth and it can be a habit that is sustained throughout a patient’s life. I hope that’s the norm that we can get to as a civilization.
We don’t expect to have a telephone conversation with an actual human employee when we need to interact with a big company like Amazon, where most communication is via an online form, email, or other electronic message. How has that expectation affected healthcare?
Access is good. The mode of the day may be messaging, but it will undeniably change. You see this with connected devices. The example you just highlighted presents an interesting opportunity for health systems and providers. These big tech companies are actually going to a further extreme, which is attacking the labor problem. They want to optimize, they want margins to go up, and they have started making everything automated.
I had an issue recently with a ride hailing service. I called the company and couldn’t talk to a human being. It only gave me automated menu options. I went through it five times just to keep saying I was dissatisfied. I wanted them to know five times that I was dissatisfied. There’s an opportunity for health systems to give real human care and not over-rotate the way some of these big tech companies are doing because of pressure from the public markets. It’s an interesting thing to explore. I’m going to bring it back to the team.
Who within a health system defines the messaging to customer personas that include both active patients as well as potential ones?
In the seven years since we started this company, this has changed. Seven years ago, it didn’t exist. There wasn’t anybody making those decisions. People were thinking about how to make sure patients show up to their appointments. It was a very specific point in time with the acute problem of making sure that we don’t have wasted slots. There’s more and more competition for the patient’s time right now, and there are more and more people who want to engage with a patient.
The role that we have seen come up increasingly is chief digital officer or chief patient experience officer. They may be VPs or SVPs. Maybe the most famous example of this is Aaron Martin when he was at Providence. Right now, he’s at Amazon, going back to one of your earlier points, which should probably make us a little more scared of Amazon. I have seen the role of chief digital officer that focuses on end-to-end patient experience. Cedars-Sinai has a similar role. We’re seeing this more and more, and we are also seeing a lot of folks outside of healthcare being brought into these roles, pulling from places like Disney and AARP and other brands that have done a decent job of building those relationships with their customers. I like the trend and I hope it continues.
Was it a big change for EHR vendors to open their system to third-party applications? Do you expect further EHR integration developments?
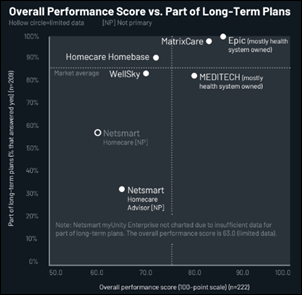
There were couple of announcements recently. You wrote about this, with Larry Ellison at Oracle Cerner making a big push around partnering and saying that partners were really important to them. I love to hear things like that. It warms my heart. Epic has done a lot of work with their App Orchard, and they’ve announced a lot of enhancements to that program. That significantly expanded the APIs that are available. We have a close relationship with Oracle Cerner and Meditech as well, and we have seen them be open in terms of data sharing. It certainly is moving in the right direction.
With the interoperability that just went into play, there was some disappointment by a lot of folks in the space that it was pared back a little bit. There’s a lot of hoops that we have to jump through in healthcare. Even when we think about these feeds, APIs may cover 20% or 30% of the use cases for a vendor if you’re lucky. For the remaining 70%, you’re doing custom HL7 or going to FHIR or Interconnect web services.
That stuff is custom, and it rarely translates from customer to customer. That makes it significantly more complicated. It’s not like an app in the App Store, where you deploy it to Apple and anybody can download it. It requires an implementation. There’s a whole industry in healthcare around professional services and consulting firms that do this for a living. So we are definitely going in the right direction, but we are nowhere near where some other industries, like high tech, are.
A lot of technology adoption happened during the pandemic. As we try to find the new normal, how will that experience be applied?
I have this belief that in the universe, everything has to balance out at equilibrium. This is true for politics, relationships, you name it. Everything needs to find its balance. Things went off balance during COVID. What I’m seeing now is that we are going to shift to the other extreme, and eventually, we are going to find the middle ground. There was really quick adoption of lots of different forms of technology, purchasing cycles, and shortened deployment cycles. We solved problems very quickly.
I’m hearing more and more about consolidation. What does my EHR do? How much of this can I bring back to the EHR? I think we will see a significant paring back of the ecosystem of vendors that provider organizations maintain, along with a shift towards bringing things to the EHR that can be brought to the EHR. We will probably go to that extreme a little too much, and it will likely be a year or two before we find that balance again, where the EHR continues for those core investments and the truly additive things get prioritized and integrated and built on top of it.
How does the market for innovation look if EHRs replace some of those third-party applications and health system consolidation creates bigger but fewer prospective customers?
There’s a famous saying in Silicon Valley that down markets are where the best companies are formed. That creates pressure and forces entrepreneurs to the right places. If a health system can get “good enough” from their EHR, they’re going to go with that. Innovation will need to be unique, differentiated, and tough to replicate. It will do a good job of weeding out the possible solutions in the market, which could be good for healthcare IT overall. In the markets, it will look like investment dollars are slowing into healthcare IT. It will look like fewer purchasing decisions and like more consolidation. But the very best companies will form out of that pressure.
It will be net positive, but it will feel rough for a while. It may hurt health systems that adopted a lot of those technologies during COVID. Some of those technologies may disappear because the company goes out of business or is gobbled up by somebody else. It’s more important than ever to provide differentiated value and to understand the problems du jour of our customers, because they are very different than they were during COVID. It’s a totally different set of challenges. Now it’s labor shortages, labor costs, and margins. We see this in the news every day. We see a tremendous number of layoffs despite a really strong jobs market. It’s a confusing time.
What will be the direction of the industry and company over the next three or four years?
We absolutely have to be added to the EHR. We need to work with the big EHR players, understand what they’re going to tackle and what they’re not going to tackle, and fill in those holes. We need to pair that with what our customers are telling us they need, that are must-dos for them to get through this. It will be a dark period for the next couple of years.
We believe in creating an open platform. It will be important to create and invest in our infrastructure so that anybody in the healthcare IT space, any vendor, can route communications through us. I’d like them to be able to do it with no friction. Plug in to Artera once and you can send communication to any of our healthcare partners who enable you. That’s where we need to get to. We need to create that network. That will create a lot of value for healthcare IT and health systems.
Comments Off on HIStalk Interviews Guillaume de Zwirek, CEO, Artera















































Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…