Robert Murphy, MD is chief medical informatics officer at Memorial Hermann Healthcare System of Houston, TX.
Tell me about your priorities at Memorial Hermann.
I’m the system CMIO at Memorial Hermann. The organizational priorities really continue to be the same. We’re trying to drive quality, creating the best experience for our patients and our physicians.
The Meaningful Use thing that just came out has helped stimulate or augment the priorities, but really, they were things we were doing already. It may be helping us accelerate in some areas faster than others, but we already had CPOE planned across the enterprise. We already had CDS [clinical decision support] in a pretty deep fashion.
We’ll probably add a little bit more in the documentation and maybe getting more effort on the ability to exchange information with our physician practices. We had all of these elements in place even before the stimulus plan was announced.
What’s your reporting structure?
I report directly to Dr. Mike Shabot, who is the chief medical officer, and dual-report to David Bradshaw, the system chief information officer.
How about underneath you?
I have the area of medical informatics — CPOE and clinical decision support. I have the groups that do the order sets and support the CDS. Also, some pharmacist informaticists and some outcomes folks who work on my team.
What are your thoughts about the value of CPOE in outcomes and patient safety based on recent studies? You’ve done this in more than one place.
You know the history of the literature. You know some of the things that have come out with potential unintended consequences, and I guess I’ve been a consumer of whatever research and practices and articles that come out to learn from whatever those experiences are. I think there are certain things that, as a physician, clearly you see the benefit of simple things like handwriting. Having practiced for over 10 years, I saw quickly that handwriting is a contributor in many ways.
In addition, you start to see the benefits of what clinical decision support can do. That’s probably the area that I feel is the most valuable in all of this.
On the flip side, seeing the potential for unintended consequences has made me very thoughtful and exhaustive in preparation to make sure that we do everything we can to prepare the medical staff, prepare the clinical operation staff, and to be very dynamic in responding to issues that come up.
It’s clear to me that well-implemented physician order entry with decision support can make improvements in quality of care. Internally, certainly we are seeing some demonstrable quality outcomes from that. We’ve gone a slower approach than many, so our implementation, our first two hospitals, went service line by service line over a month. It took us almost two years to get to 75%.
That was really by design and slow and purposeful, but now as we’re bringing in additional campuses and departments online, I think we’ll be able to accelerate. I think the initial focus on careful, slow attention has been beneficial.
Are you a Cerner shop there?
We are.
Everything that you have on the clinical side is Cerner?
Everything but our OB department. That’s the only major clinical area that’s still not Cerner.
How should hospitals approach the clinical decision support requirements of the proposed Meaningful Use criteria?
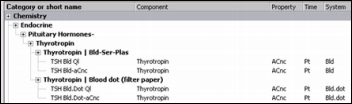
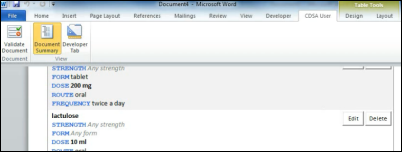
You really start to see several buckets of where clinical decision support is important. The first is there’s just simple check objectives — do you have drug-drug interactions, drug formulary, drug-allergy checking? I would say that’s often the most rudimentary type of decision support.
In fact, the more and more we evaluate it, the more we are refining that from the simple tool that the vendors supply. For instance, the major pharmacy databases — First DataBank and Multum — come packaged with these drug-drug interactions. The longer we’ve gone, the more we’ve customized and turned off the alerts that are not that helpful clinically. To sites that are just going live, I think it’s some thoughtful caution and what level you set any of those settings. That’s the first big bucket of those simple ones.
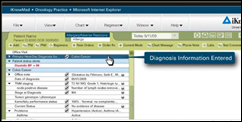
Then you get into the current proposed objective that says you must have five CDS rules and those must be related to the quality measures. I think that was in advance from the original draft, and I think it’s one of which most of us embrace and are happy to see.
That gets into the more complicated type of decision support of workflow and how you’re going to capture these patients. What’s the correct trigger? What’s the correct notification to what user at what time? Folks here knew those quality measures.
If folks are just getting started, they need to keep it as simple and straightforward as they can. Simple things like on an order set for an acute MI — make sure the aspirin is checked or contraindication is documented. The one thing for some advanced hospitals is, if I look at that one — aspirin in acute MI — most of our hospitals are 100%, and have been so for the last six months.
Is that helpful for us to put a rule in place for something we’re already 100% for? For us, probably not. But for hospitals that aren’t 100% and need something simple to get in, those are thing kind of things I think you’ll see them focus on.
The third element is what clinical decision support can maybe bring as you continue to advance the tools that you have. One that we’re investigating right now is how do you correctly populate a problem list? For a large organization, on the inpatient hospital side, managing a problem has become very, very difficult with so many users — physicians, consultants, nursing, and others.
What is the most valuable part of a problem list? From a CDS perspective, we may, in fact, try to focus on identification of certain conditions — diabetes, high blood pressure, heart failure — that we can identify with good specificity and maybe add those as part of our CDS portfolio. You start to see, again, from the rudimentary to the more advanced organizations, will have to progress. I think most places will have several years to get there, but it’s still going to be a big challenge for small hospitals, I think.
Most clinical decision support isn’t guidance, but rather non-personalized canned warning messages that are either turned on or turned off for everyone. What about being able to tailor specific types of warnings to specific practitioners or types of practitioners?
We have those features in place and I would say most large vendors’ sophisticated CDS engines will have those capabilities. The problem is the work that requires for that customization. It takes an analysis of workflow and even certain elements of credentialing — which user can or cannot respond and answer to a request to initiate an order? Can it be a nurse or pharmacist or a mid-level provider, or must it be a physician? At certain places, is it the resident or the attending?
It gets into such role-based specificity it really is a challenge, even with the tools that are available. They often allow that flexibility. It’s a real burden for organizations how to effectively analyze, plan, monitor, and continue to improve those sorts of tools.
But in general, it seems there’s a gap between what outsiders who are setting these things up think physicians should need to see or want to see, versus those that the real practicing doctors actually find useful. How do you address that gap?
That, again, shows you the scale from the rudimentary — the drug-drug interactions. For instance, we’re a large organization, so we’re doing the specific work. We will turn off the Multum pharmacy formulary drug-drug interaction. We will most likely build a custom alert that will be able to analyze several parameters of that drug-drug interaction, not just this patient falls into a generic category, but your patient is this age, this weight, on these other medications all at the same time; you may want to consider X, Y, and Z. That’s the complexity that it’s going to be there for.
I do worry a little bit about the industry just trying to put in drug-drug interactions from a generic platform across large organizations or large populations. I think you’re going to see more and more refinement, and hopefully, tools for which we can all share that information.
You’re starting to hear discussion on how are we going to build these repositories of CDS knowledge through perhaps the AHRQ or other groups who could help us catalog that information that could then be more easily implementable. Right now, that’s the most basic, core format — things like drug-drug interactions that have very low utility.
The average hospital subscribes to First DataBank or Multum or whoever and then just selectively turns things on and off because that’s all the time and resources they have. How much of the value of decision support are they really getting by just looking at those warnings versus real guidance that let doctors make the right decisions instead of telling them when it looks like they didn’t?
I can share our internal experience once we began looking at specific drug-drug-based pairs. When I started five years ago, we had a large population of drug-drug interactions that were overridden 100% of the time. We had pairs that were 98-99% of the time. You start to see the incredible burden that has. That may lead to alert fatigue.
I think we need to continue to study alert fatigue. There may be a critical CDS rule or intervention that is very specific and very sensitive and very important to be addressed. If, however, that’s firing in a constant bombardment of 10 or 20 interactions and interventions, the truth is, you will begin to ignore the most important interventions.
Our attention in the last several years has been to turn off the generic, non-specific items and build more and more custom. I think it really does create some challenges for smaller organizations to address that. I just have to hope to continue to see the industry and some of the specialty societies in informatics and AHRQ who can then help us come up with more specific proposals for effectiveness in the CDS space.
The announcement just came about of the three big hospital systems that licensed their order set content to Zynx. That didn’t work so well when Eclipsys paid a fortune for Brigham’s BICS rules back in the ‘90s. Do you think that the rules that one facility creates are useful to others?
There again, you get into some of the local details that need to be built, as opposed to the medical evidence that needs to be somewhat codified. That’s where I look.
I know the AHRQ has a project underway to look at screening recommendations. Those are pretty straightforward on the evidence, but once again, that information is very helpful for us to share. Even our experience on the effectiveness of a certain rule may be useful. But as far as sharing the actual codified rule, even among Cerner clients, that’s often just a template to get started, but it often takes the customized work from the local environment.
I can give a couple of examples. What is the correct value of a potassium warning? Is it 5.0, 5.5, 6.0? You can look at it a lot of different ways, but often the sensitivity and specificity is inversely related as those levels go up. Somebody at some point must make an objective decision what it’s going to be. Is it going to be 5.5, 5, or 6? Most often, you’re going to need a local decision on governance to see what your final flag might be set at.
Isn’t that kind of a conundrum, though? All these rules that are very black-and-white specific, yet every hospital says, “I don’t like the way those come.” Is medicine really scientific enough that a rule ever fits?
You can continue to imagine, with a large amount of data points, to make them more and more specific. Like I mentioned earlier, the more specificity you can have on a patient’s age and weight and previous medications and previous problems, they give you more data elements to make the rules and interventions more specific. But once again, you’re looking at large computing power. You’re looking at ways to not negatively impact response time, for instance.
It remains, I think, one of the big challenges in the field is to have things that have a very high positive predictive value — that when an alert fires, it changes behavior. I guess the ideal state would be that’s the only kind of intervention that would fire is when it changed a behavior. Most groups think well, if you can get above 50%, you’re probably doing a pretty good job, but approaching 100% will be very difficult. If you can get above 50%, most of your users are finding things more helpful than annoying. That’s probably a reasonable goal for most interventions.
You can measure that. Are you shutting off those that don’t change behaviors?
Absolutely, and that is another component of the work required to have effective CDS is that monitoring. As I mentioned, we do analyze response to alerts. We look at the clinical outcomes, not just the response to the alert.
Another interesting fact we’re discovering is there are times in which the alert is overridden, yet later, the correct behavior is changed. At first thought you say, “Well, they overrode the alert; therefore, it was useless.” But it turns out, in certain situations, you’ve at least prompted them to think about things. You notice as you analyze more data that they actually did make a positive response.
Certain elements such as warfarin dosing with an elevated INR — that’s been a classic example where we’re seeing that those alerts are helpful even when they override the initial alert. They can maybe dose it more correctly later in the stay and during the days of administrations. It’s a component of correct design and monitoring and continuous feedback to make them better and better for the users.
I think people miss the fact that CPOE itself is clinical decision support even without all the warnings and alerts because it presents only the most common orders and the preformatted doses. Would you agree?
I absolutely agree. I think that’s what you find in the folks that do this work longer and longer. You realize that clinical decision support is really a comprehensive approach that includes how you structure your data. How you present information is even a form of decision support.
Then, the computer-based logic is only one component, but how you build the order sets, the choices you give for selections, are often — we use the phrase, “You want to make the right thing the easy thing.” You want to make the right thing in the information you present them; the right thing in the orders and the sequence of the orders, the choices that are most available; and the right thing in a clinical decision support rule that may help catch things that were missed at first. All of those elements together help you have that comprehensive approach that’s necessary, I believe.
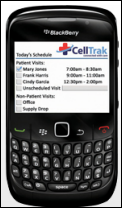
You’ve done some work with mobile devices.
That’s been an interesting journey as well. We were a very early adopter, six or seven years ago, at Memorial Hermann. At that point, I think there were some big technology barriers — large devices, heavy batteries, needing an internal wireless network connection — that were a struggle.
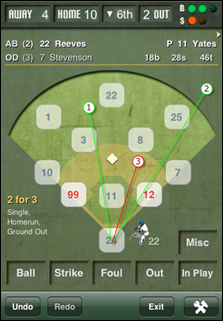
Now we’ve advanced into more the iPhone-enabled group. Once again, it’s the right device with the right information at the right moment. The big one we’ve seen a huge success on is the AirStrip OB product, which allows fetal monitoring to be seen by our obstetricians. They can talk directly to the nurse about what patterns they’re seeing. It’s had a large and growing usage with our obstetricians. It’s wonderful to hear from the nurses that they feel so much more connected to the physician in being able to review strips remotely together and then making a good decision. That particular product has been very well received.
We’ve not really gone into clinical systems on our mobile platforms. We have a trial coming up this summer of one we’ve internally developed for the iPhone, and it’ll just be a snapshot of patient data. The great thing about iPhones and web development is that those things can be pretty straightforward to produce, and so we’ll be trialing our own internal version of that later this summer. We’ll continue to see.
We’ve understood vendors are out there with CPOE Lite products, but at a certain point … I’m not sure. It might be a nice bridge to help physicians though it, but for a large enterprise, I’m not sure it’s going to be the kind of solution that they’re looking for.
You mentioned that you’re pretty comfortable, or had an early start at least, on Meaningful Use. Based on the proposed criteria, how prepared is Memorial Hermann and what to-dos do you think you need to accomplish to be ready?
I guess the biggest one is going to CPOE at what percentage at our hospital. We have 11 hospitals. Our first two hospitals came live with CPOE.
We clearly had the strategy. The hospital would come up and we’d get the hospital totally up to a 75% or higher physician ordering usage. Once we had that, we quickly realized at that point, that was the inpatient ordering, and we then realized that it was critical to have our ER on the same system. So, we actually took a pause and we have installed the Cerner FirstNet product while that was going forward. With that, all of our ERs are going CPOE, so that’s really the first unit in all of the other hospitals that will go live with CPOE.
Well, Meaningful Use came out and said there’s a 10% threshold. We thought, well that’s great, because the ER would cover that 10%. Then, to find out they’ve actually excluded the ER from that calculus at present.
Once again though, we’re not going to alter our strategy. We’re going to finish our first wave of rollouts. Then this fall, we’ll have additional hospitals coming up. But we still believe that we need to have a hospital-wide approach. We don’t want to get on a partial 10% of every hospital just to get the number. Some of our hospitals will be delayed.
That’s probably the most challenging of the measures to hit. Most of the other measures we have good plans for and projects in place. I think we should be able to meet the other objectives pretty straightforwardly.
Any concluding thoughts?
As a physician, I got into this field of medical informatics, you know, you want to make a big difference for an organization and for patient care.
The longer I’m in this, you start see that people, process, technology triangle that defines medical informatics. I think it continues to be in that order — the people, the process, and then the technology. I’m finding that with the right amount of money and the right engineering and support staff, you can get the technology right.
The people and process of healthcare are challenging in the nature of healthcare. Often they’re just challenging from being the cottage industry that we are. That individual autonomy is such a strong current. But you hope and you start to see that by providing tools that provide consistency and standardization and provide value that you can help drive hospitals and populations to improve care.
I think that’s what I continue to focus on, really — the people, process, and technology. If we can keep focused on that, hopefully we’ll continue to do good work.






































































In fairness to the person on the thread the other day: Now THIS is politics on the blog. :)