Top News

Microsoft and GE announce the formation of a joint venture company that will take over most of the people and assets of the Microsoft Health Solutions Group along with specific GE Healthcare products. See the HIStalk story from early Thursday, which includes insights from interviews with the key executives involved.
Reader Comments
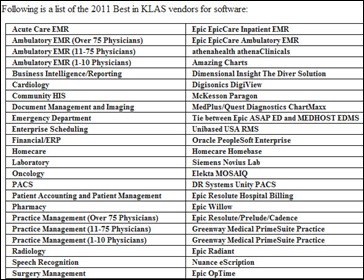
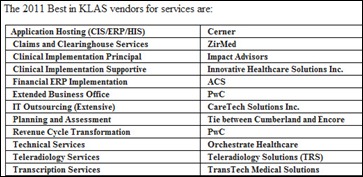
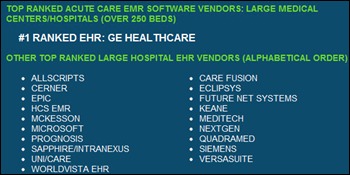
 From Curious Reader: “Re: Black Book Rankings. I am confused about Black Book’s results. Do they break out their ratings by hospital size? CPSI usually sells to community hospitals, not the same ones Epic sells to. I don’t know how those are comparable. How is Black Book even defining and EMR? Picis is a surgery and anesthesia vendor — they don’t really have an EMR system.” This report includes multiple categories including under 100-bed hospitals, community hospitals, large hospitals, health systems, and EDs. Per Black Book’s website, the rankings are based on survey results that cover 18 performance areas. To make the Top 20 list, vendors must have at least 10 unique clients participate. Results for these ratings were based on 12,075 validated responses. There is no mention on how an EMR is defined, though it may be included in the full report. In you need to further satisfy your curiosity, you can purchase a report for $3,250, but note it will only include details on a single category and not all the inpatient EHR categories.
From Curious Reader: “Re: Black Book Rankings. I am confused about Black Book’s results. Do they break out their ratings by hospital size? CPSI usually sells to community hospitals, not the same ones Epic sells to. I don’t know how those are comparable. How is Black Book even defining and EMR? Picis is a surgery and anesthesia vendor — they don’t really have an EMR system.” This report includes multiple categories including under 100-bed hospitals, community hospitals, large hospitals, health systems, and EDs. Per Black Book’s website, the rankings are based on survey results that cover 18 performance areas. To make the Top 20 list, vendors must have at least 10 unique clients participate. Results for these ratings were based on 12,075 validated responses. There is no mention on how an EMR is defined, though it may be included in the full report. In you need to further satisfy your curiosity, you can purchase a report for $3,250, but note it will only include details on a single category and not all the inpatient EHR categories.
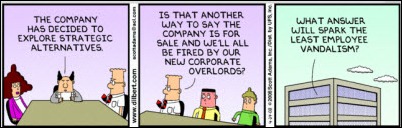
 From EMR Wannabe: “Re: GE and Microsoft. From trying to work with it, I know that Amalga UIS is an overly complicated hairball. I wasn’t sure about Qualibria, although last year when I asked a GE team how the knowledge project with Intermountain Health was going, they just broke into laughter and said, ‘depends who you ask.’ I said, ‘Well, I’m asking you,’ to which they took the Fifth (amendment, not bottle). Now with this announcement, we can see that Microsoft and GE decided to combine, and then bury, their respective dead or dying.” Amalga seems cool, but I don’t hear much from its customers once they’ve signed contracts, so NewCo should work to get the word out. I hope the companies really are planning to do something innovative like the announcement says. However, those with long memories will find it hard to forget (or forgive) historical examples of big, unfocused vendors who brashly stormed the HIT gates and then slunk off quietly shortly thereafter, unceremoniously dumping the charred remains of once-proud companies they had burned through and hoping the smell of utter failure would wash out of their Teflon-coated corporate suits. Recall when Baxter and IBM formed IBAX and quickly sold it off to HBOC, relieved to put distance between themselves and the albatross they had spawned from their passionate but short-lived union by creating a new company and not really caring whether it succeeded or failed.
From EMR Wannabe: “Re: GE and Microsoft. From trying to work with it, I know that Amalga UIS is an overly complicated hairball. I wasn’t sure about Qualibria, although last year when I asked a GE team how the knowledge project with Intermountain Health was going, they just broke into laughter and said, ‘depends who you ask.’ I said, ‘Well, I’m asking you,’ to which they took the Fifth (amendment, not bottle). Now with this announcement, we can see that Microsoft and GE decided to combine, and then bury, their respective dead or dying.” Amalga seems cool, but I don’t hear much from its customers once they’ve signed contracts, so NewCo should work to get the word out. I hope the companies really are planning to do something innovative like the announcement says. However, those with long memories will find it hard to forget (or forgive) historical examples of big, unfocused vendors who brashly stormed the HIT gates and then slunk off quietly shortly thereafter, unceremoniously dumping the charred remains of once-proud companies they had burned through and hoping the smell of utter failure would wash out of their Teflon-coated corporate suits. Recall when Baxter and IBM formed IBAX and quickly sold it off to HBOC, relieved to put distance between themselves and the albatross they had spawned from their passionate but short-lived union by creating a new company and not really caring whether it succeeded or failed.
For those scoring the Microsoft-GE JV at home, I’d watch for: (a) an indication of how much money the partners are investing vs. just letting the new organization sink or swim on whatever revenue it can muster; (b) the announcement of a real, delivered, buzzword-free product; (c) press releases listing newly signed contracts from paying customers that aren’t cherry-picked partner sites getting something else in return; (d) a lengthening roster of third-party developers that buy the “ecosystem” story and build useful apps on top of it; and (e) the assignment of experienced, high-ranking executives to the new company (so far new CEO Michael Simpson is the only person named and he’s been with GEHC only since 2010.) Some would say Peter Neupert’s retirement was the most negative aspect of the news (and it wasn’t even included in the announcement,) but to me it’s the fact that the announcement was made in such a hurry that they hadn’t even chosen a company name yet. We will report their progress here, good or bad. I’m as guilty as anyone about moaning that nobody innovates, then laying on the scorn when someone tries, so I’ll try to be cautiously optimistic, even though in talking to Neupert and Simpson Wednesday before the announcement, I couldn’t figure out exactly what they are planning to build, who the customer will be,and how the odd lot of products will contribute to the end result. I’m neutral on most of the products named since I’ve heard little about them, but I hope the former Sentillion people and applications don’t suffer in the chaos since they deserve better, having created a strong base of hospital customers that rely on their technologies.
 From SmallMe: “RE: Microsoft HSG. Major RIF and re-org in advance of the HSG/GE joint venture announcement.” According to our Microsoft contact that I asked to confirm, “Like all companies, Microsoft evaluates our business priorities regularly. As we evolve HSG’s strategy, we’re concentrating more on building a compelling platform and have eliminated a small number of positions to align with current priorities.”
From SmallMe: “RE: Microsoft HSG. Major RIF and re-org in advance of the HSG/GE joint venture announcement.” According to our Microsoft contact that I asked to confirm, “Like all companies, Microsoft evaluates our business priorities regularly. As we evolve HSG’s strategy, we’re concentrating more on building a compelling platform and have eliminated a small number of positions to align with current priorities.”
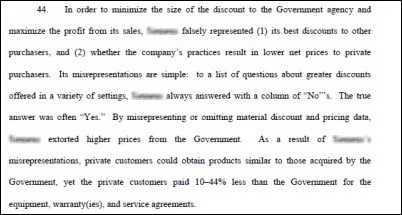
 From EthicsInHealthcareBusiness: “Re: RSNA. I’m surprised there isn’t more stringent hiring vetting by big vendors. Take the example of [vendor VP name omitted], who while at [vendor name omitted] was named in a federal lawsuit (CIVIL NO. 2004-116) accusing him of fraudulent pricing in dealings with government purchasing agents. The lawsuit was dismissed on a technicality, but it drove a parallel criminal investigation by the Defense Department and the US attorney’s office in Philadelphia. Why would a company risk this potential liability?” I omitted the specifics since, as you said, the lawsuit was dismissed and his innocence must be presumed. If he’s found guilty by the Feds, I’ll name names. His previous employer was known both globally and historically for shameful bribery. I blurred their name only a little above, but enough to say I didn’t unfairly name the company specifically.
From EthicsInHealthcareBusiness: “Re: RSNA. I’m surprised there isn’t more stringent hiring vetting by big vendors. Take the example of [vendor VP name omitted], who while at [vendor name omitted] was named in a federal lawsuit (CIVIL NO. 2004-116) accusing him of fraudulent pricing in dealings with government purchasing agents. The lawsuit was dismissed on a technicality, but it drove a parallel criminal investigation by the Defense Department and the US attorney’s office in Philadelphia. Why would a company risk this potential liability?” I omitted the specifics since, as you said, the lawsuit was dismissed and his innocence must be presumed. If he’s found guilty by the Feds, I’ll name names. His previous employer was known both globally and historically for shameful bribery. I blurred their name only a little above, but enough to say I didn’t unfairly name the company specifically.
 From Erik: “Re: McKesson. Halting all development of Horizon Clinicals 10.3 and deployment of Horizon Enterprise Revenue Manager.” Unverified. I got several e-mails from MCK employees Thursday morning that a company call was in progress (our readers are so loyal I’m surprised they didn’t conference us in.) Inga asked what was up and I told her if I had to guess, I would say MCK is either killing off Horizon or moving its revenue cycle efforts from HERM to Paragon since both had been rumored previously. I’ll be crowing to her endlessly if both guesses are correct, although I must credit readers who reported those possibilities to me in the first place starting many months ago. I’ll know more Friday, as McKesson Provider Technologies President Dave Souerwine asked to brief me. Unfortunately it will be late in the afternoon since I have to get home after work from the hospital to do it (darned day job!), but I’ll recap in the Monday Morning Update if not before.
From Erik: “Re: McKesson. Halting all development of Horizon Clinicals 10.3 and deployment of Horizon Enterprise Revenue Manager.” Unverified. I got several e-mails from MCK employees Thursday morning that a company call was in progress (our readers are so loyal I’m surprised they didn’t conference us in.) Inga asked what was up and I told her if I had to guess, I would say MCK is either killing off Horizon or moving its revenue cycle efforts from HERM to Paragon since both had been rumored previously. I’ll be crowing to her endlessly if both guesses are correct, although I must credit readers who reported those possibilities to me in the first place starting many months ago. I’ll know more Friday, as McKesson Provider Technologies President Dave Souerwine asked to brief me. Unfortunately it will be late in the afternoon since I have to get home after work from the hospital to do it (darned day job!), but I’ll recap in the Monday Morning Update if not before.
 From MCKWorker: “Re: McKesson. All HERM staff essentially laid off. New direction for development, to combine with Paragon. HERM employees will have 60 days to interview for positions with that new strategy.” Unverified. It’s funny that Inga pinged a couple of her MCK sources and they told her company bigwigs had warned them that HIStalk would be probing for information. They were correct. Inga and I were flattered, even though the compliment was almost certainly unintentional. Apparently they weren’t too worried about anyone but us being on top of the breaking news and caring enough to dig beyond any official announcement.
From MCKWorker: “Re: McKesson. All HERM staff essentially laid off. New direction for development, to combine with Paragon. HERM employees will have 60 days to interview for positions with that new strategy.” Unverified. It’s funny that Inga pinged a couple of her MCK sources and they told her company bigwigs had warned them that HIStalk would be probing for information. They were correct. Inga and I were flattered, even though the compliment was almost certainly unintentional. Apparently they weren’t too worried about anyone but us being on top of the breaking news and caring enough to dig beyond any official announcement.
 From Must Remain Anonymous: “Re: McKesson. It has finally happened! The call came today that McKesson will cease development of its Horizon product. All support will stop in seven years. Product development will now focus on the Paragon application instead. To be announced to their physician advisory council tomorrow morning. It is about time that McKesson drops the dead weight.” Unverified, until Friday anyway. If true, that would be truly remarkable given that Paragon has been close to being killed off several times, as Vince has explained in his HIS-tory lessons. Horizon has ample problems, but to think of Paragon as MPT’s flagship product is a mind-bender. If true, kudos to that little engine that could for hanging in there, excelling over and over, and giving the company an overachieving understudy for when its star couldn’t make curtain call.
From Must Remain Anonymous: “Re: McKesson. It has finally happened! The call came today that McKesson will cease development of its Horizon product. All support will stop in seven years. Product development will now focus on the Paragon application instead. To be announced to their physician advisory council tomorrow morning. It is about time that McKesson drops the dead weight.” Unverified, until Friday anyway. If true, that would be truly remarkable given that Paragon has been close to being killed off several times, as Vince has explained in his HIS-tory lessons. Horizon has ample problems, but to think of Paragon as MPT’s flagship product is a mind-bender. If true, kudos to that little engine that could for hanging in there, excelling over and over, and giving the company an overachieving understudy for when its star couldn’t make curtain call.
And lest we forget among the corporate announcements from the several companies mentioned here, there are people behind these decisions, grunts like you and me who leave their families every day to do the best job they can, competently even though their expertise is related to products no longer in favor, who are torn with worry about their future livelihoods that are being manipulated invisibly by factors entirely beyond their control as corporate drones judge them unfairly on what they do today rather than their ability to contribute in a different way tomorrow (I hate that about corporate BS more than anything). Right now, they’re putting on a game face to try to make a nice Christmas or Hanukkah for their kids and families without seeming too preoccupied by work stuff that shouldn’t be intruding on their celebrations and religious observations, but at night when the lights go out, they are sleepless in contemplating what could change for them and those who depend on them. Join me in beaming some positive thoughts their way because I’m guessing they could use them right about now. I’ve been there and it sucks, but it eventually gets better.
 From Kurt: “Re: McKesson. I’m hearing they announced that they are spending $1 billion in healthcare IT. Is this correct? If so, this is more than most other vendors combined.” I’ll let you know soon. That sounds like an awfully large number even for a company of McKesson’s size, but I’m not ruling anything out. If they asked me for advice (not likely), I’d say they should show some leadership (meaning spend money) in building innovative solutions that will make their HIT presence respectable (i.e., high KLAS scores and a growing customer base), unlike their fellow conglomerate vendors that seem to be happy milking the wrinkled, desiccated udders of their thinning herds of malnourished and badly aging cash cows. In McKesson’s defense, they did make a huge investment (and later write-down, unfortunately) in developing HERM, so give them some credit for taking action, even if the result wasn’t what they had hoped. Corporate management has changed since then (and probably for that reason), so perhaps the environment is more conducive to nimble innovation now. I’d have to see that to believe it since it’s a rarity in a huge, publicly traded company.
From Kurt: “Re: McKesson. I’m hearing they announced that they are spending $1 billion in healthcare IT. Is this correct? If so, this is more than most other vendors combined.” I’ll let you know soon. That sounds like an awfully large number even for a company of McKesson’s size, but I’m not ruling anything out. If they asked me for advice (not likely), I’d say they should show some leadership (meaning spend money) in building innovative solutions that will make their HIT presence respectable (i.e., high KLAS scores and a growing customer base), unlike their fellow conglomerate vendors that seem to be happy milking the wrinkled, desiccated udders of their thinning herds of malnourished and badly aging cash cows. In McKesson’s defense, they did make a huge investment (and later write-down, unfortunately) in developing HERM, so give them some credit for taking action, even if the result wasn’t what they had hoped. Corporate management has changed since then (and probably for that reason), so perhaps the environment is more conducive to nimble innovation now. I’d have to see that to believe it since it’s a rarity in a huge, publicly traded company.

 From Leotardo: “Re: Epic in the UK. Old news?” Two big-name English hospital trusts name their short list of potential post-NPfIT EMR vendors: Cerner, Epic, and Allscripts. The report says that “Epic is known to have invested heavily in the Cambridge procurement.” The Brits had better price out flights from London to Madison before finalizing a budget since they would be creating a massive carbon footprint for the endless mandatory training visits. Britain was one of few places where Cerner could pursue business knowing that Epic wouldn’t be sitting across the table, so news of an Epic win would not be celebrated in KCMO. And if Epic loses, that would be even bigger news since they usually don’t.
From Leotardo: “Re: Epic in the UK. Old news?” Two big-name English hospital trusts name their short list of potential post-NPfIT EMR vendors: Cerner, Epic, and Allscripts. The report says that “Epic is known to have invested heavily in the Cambridge procurement.” The Brits had better price out flights from London to Madison before finalizing a budget since they would be creating a massive carbon footprint for the endless mandatory training visits. Britain was one of few places where Cerner could pursue business knowing that Epic wouldn’t be sitting across the table, so news of an Epic win would not be celebrated in KCMO. And if Epic loses, that would be even bigger news since they usually don’t.
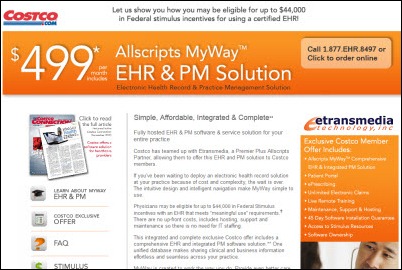
 From Wildcat Well: “Re: Costco selling Allscripts MyWay. Isn’t that an insult to every EHR sales rep out there? What exactly will Allscripts sales reps do now? The EMR adoption bubble is developing a very short shelf life.”
From Wildcat Well: “Re: Costco selling Allscripts MyWay. Isn’t that an insult to every EHR sales rep out there? What exactly will Allscripts sales reps do now? The EMR adoption bubble is developing a very short shelf life.”

 From JB: “Re: Epic. I think this job would be humorous to highlight.” Epic hires only fresh-from-college greenhorns, so if you are experienced in healthcare IT, informatics, consulting, or process re-engineering, this is your one chance to get your foot in the Star Trek-themed door. I wonder how many Epic dishwashers have passed the company’s notorious MUMPS programming test?
From JB: “Re: Epic. I think this job would be humorous to highlight.” Epic hires only fresh-from-college greenhorns, so if you are experienced in healthcare IT, informatics, consulting, or process re-engineering, this is your one chance to get your foot in the Star Trek-themed door. I wonder how many Epic dishwashers have passed the company’s notorious MUMPS programming test?
 From Poutine: “Re: Quebec’s medical error registry. Finally done after being promised in 2002, but not getting provider data.” Provider error reporting is mandatory, but a third of them submitted incomplete information, while nine hospitals claimed “technical difficulties” that prevented them from filing even one report.
From Poutine: “Re: Quebec’s medical error registry. Finally done after being promised in 2002, but not getting provider data.” Provider error reporting is mandatory, but a third of them submitted incomplete information, while nine hospitals claimed “technical difficulties” that prevented them from filing even one report.
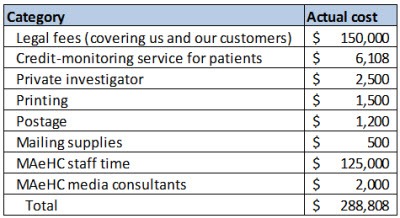
 From Skeptic: “Re: Micky Tripathi’s breach article. Part of me says. ‘Well done for a conscientious job.’ It’s not as if the folks involved had much of a choice in how to respond if they wanted to be law-abiding and careful stewards of the cards handed them by our system. The rest of me says. ‘This is insane.’ A street thief steals a laptop and there is ‘an infinitesimally small chance’ the information would be accessed and/or abused. We spend $300K direct dollars and another large chunk of internal time — not to mention hours spent on the government regulatory side — addressing it, after which the thug still has the laptop and the exposure is still infinitesimally small. How much will we spend when the risk is real? And the lesson learned is that we all need to behave even more carefully and institute even more policies. This is great news for security companies, government agencies, and regulators. It’s horrible news for patients. Every dollar we spend on this kind of craziness is a dollar not available for patient care. At present, we’ve managed to construct a ridiculously expensive system relative to actual care delivered. This is an index case of how we’ve done it. (a) lesson one: no amount of anything is going to prevent this sort of thing. That’s not an excuse to be careless, but we need to use some common sense when applying blame. This blame falls on the thief. Period. (b) lesson two: the most sensitive data the healthcare system owns is financial. Identity theft is worth cash; PHI is close to worthless despite the paranoia surrounding it. We need to find ways to universally encrypt ADT/financial information and to not bind it so tightly to PHI. (c) lesson three: if we want to deliver better healthcare, there are better places to spend our patients’ money.”
From Skeptic: “Re: Micky Tripathi’s breach article. Part of me says. ‘Well done for a conscientious job.’ It’s not as if the folks involved had much of a choice in how to respond if they wanted to be law-abiding and careful stewards of the cards handed them by our system. The rest of me says. ‘This is insane.’ A street thief steals a laptop and there is ‘an infinitesimally small chance’ the information would be accessed and/or abused. We spend $300K direct dollars and another large chunk of internal time — not to mention hours spent on the government regulatory side — addressing it, after which the thug still has the laptop and the exposure is still infinitesimally small. How much will we spend when the risk is real? And the lesson learned is that we all need to behave even more carefully and institute even more policies. This is great news for security companies, government agencies, and regulators. It’s horrible news for patients. Every dollar we spend on this kind of craziness is a dollar not available for patient care. At present, we’ve managed to construct a ridiculously expensive system relative to actual care delivered. This is an index case of how we’ve done it. (a) lesson one: no amount of anything is going to prevent this sort of thing. That’s not an excuse to be careless, but we need to use some common sense when applying blame. This blame falls on the thief. Period. (b) lesson two: the most sensitive data the healthcare system owns is financial. Identity theft is worth cash; PHI is close to worthless despite the paranoia surrounding it. We need to find ways to universally encrypt ADT/financial information and to not bind it so tightly to PHI. (c) lesson three: if we want to deliver better healthcare, there are better places to spend our patients’ money.”
HIStalk Announcements and Requests
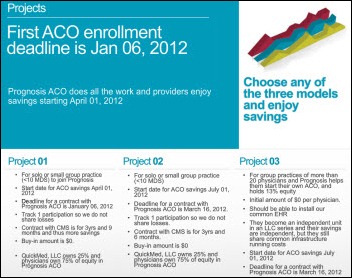
 Thanks to Micky Tripathi’s outstanding contribution on his organization’s patient data security breach, traffic on HIStalk Practice has been especially heavy this week. We’ve posted a number of other great items over the last week including Brad Boyd’s discussion on the need for clinically integrated organizations. Other news bits of note: CMS releases a well done MU toolkit for providers. Physicians are fairly unaware of ACOs and don’t know if they should join one. Only 4% of all eligible providers have been paid incentives for meaningful EMR use. Physician wait times are shortest in Wisconsin and longest in Mississippi. Requests: (a) read HIStalk Practice regularly because it thrills me to know that my father is not the only one tuning in; (b) next time you need to purchase something HIT-related, consider the offerings of our sponsors; and (c) sign up for HIStalk Practice e-mail updates because I love knowing that I am not the only one with an overflowing inbox. Thanks for reading.
Thanks to Micky Tripathi’s outstanding contribution on his organization’s patient data security breach, traffic on HIStalk Practice has been especially heavy this week. We’ve posted a number of other great items over the last week including Brad Boyd’s discussion on the need for clinically integrated organizations. Other news bits of note: CMS releases a well done MU toolkit for providers. Physicians are fairly unaware of ACOs and don’t know if they should join one. Only 4% of all eligible providers have been paid incentives for meaningful EMR use. Physician wait times are shortest in Wisconsin and longest in Mississippi. Requests: (a) read HIStalk Practice regularly because it thrills me to know that my father is not the only one tuning in; (b) next time you need to purchase something HIT-related, consider the offerings of our sponsors; and (c) sign up for HIStalk Practice e-mail updates because I love knowing that I am not the only one with an overflowing inbox. Thanks for reading.
 On the Jobs Board: Manager of Professional Services, Senior Trainer, Senior Software Engineer. On Healthcare IT Jobs: NextGen Workflow Process Consultants, EMR Application Specialist, Technical Services Manager.
On the Jobs Board: Manager of Professional Services, Senior Trainer, Senior Software Engineer. On Healthcare IT Jobs: NextGen Workflow Process Consultants, EMR Application Specialist, Technical Services Manager.
 Inga, Dr. Jayne, and I take risks writing HIStalk. We could get fired from our real jobs if unhappy companies figure out who we are and complain to our bosses about something we’ve said about them. We could lose sponsors for reporting news objectively and stating our opinions honestly (GE, Microsoft, and McKesson are all HIStalk sponsors, for a current example, but we still have to say what we think or else we’d be just another rag that uncritically spews vendor-friendly non-news). We could lose long- or short-term significant others because we sit in front of computers way too much, or risk letting life pass us by as we fixate on the relatively tiny topic of healthcare IT after spending already-long days at work (tonight’s HIStalk took me 5.5 hours, so my total non-work time in the past 24 hours, including sleep, was about six hours.) If you want to provide some reward to offset that risk, (a) sign up for e-mail updates for HIStalk, HIStalk Practice, and HIStalk Mobile; (b) connect with us on Facebook and LinkedIn; (c) support our sponsors, especially those we have to occasionally say negative things about, by clicking their ads, checking them out in the searchable, indexed Resource Center, and sending them consulting RFIs; (d) send us rumors, news we might have missed, and updates on what’s going on where you work; and (e) help us find the good news of IT helping patients, IT people doing commendable work, and IT companies innovating and making a difference. Thanks for being part of what we do, which means you’re actually part of who we are.
Inga, Dr. Jayne, and I take risks writing HIStalk. We could get fired from our real jobs if unhappy companies figure out who we are and complain to our bosses about something we’ve said about them. We could lose sponsors for reporting news objectively and stating our opinions honestly (GE, Microsoft, and McKesson are all HIStalk sponsors, for a current example, but we still have to say what we think or else we’d be just another rag that uncritically spews vendor-friendly non-news). We could lose long- or short-term significant others because we sit in front of computers way too much, or risk letting life pass us by as we fixate on the relatively tiny topic of healthcare IT after spending already-long days at work (tonight’s HIStalk took me 5.5 hours, so my total non-work time in the past 24 hours, including sleep, was about six hours.) If you want to provide some reward to offset that risk, (a) sign up for e-mail updates for HIStalk, HIStalk Practice, and HIStalk Mobile; (b) connect with us on Facebook and LinkedIn; (c) support our sponsors, especially those we have to occasionally say negative things about, by clicking their ads, checking them out in the searchable, indexed Resource Center, and sending them consulting RFIs; (d) send us rumors, news we might have missed, and updates on what’s going on where you work; and (e) help us find the good news of IT helping patients, IT people doing commendable work, and IT companies innovating and making a difference. Thanks for being part of what we do, which means you’re actually part of who we are.
Acquisitions, Funding, Business, and Stock
 A day after we (and thus you) were tipped off by HIStalk reader Elroy, Streamline Health Solutions announces that it has signed a definitive asset purchase agreement to acquire Interpoint Partners for $5 million. We like to think they had to fast-track the announcement because of Elroy’s rumor report.
A day after we (and thus you) were tipped off by HIStalk reader Elroy, Streamline Health Solutions announces that it has signed a definitive asset purchase agreement to acquire Interpoint Partners for $5 million. We like to think they had to fast-track the announcement because of Elroy’s rumor report.

Humana acquires healthcare analytics company Anvita Health.
Sales
The federal government awards McKesson Provider Technologies its DIN PACS III contract, allowing it to sell PACS and related sub-systems to all branches of the US armed forces and civilian defense department agency facilities. The two-year contract has a potential value of $30 million.

Morehead Memorial Hospital (NC) selects Unidesk for desktop provisioning and application delivery for its VMware-based Virtual Desktop Infrastructure.
Meridian Health (NJ) to ICA’s CareAlign 3.0 for its 95 locations.
Group Health Cooperative of South Central Wisconsin and Group Health Cooperative of Eau Claire (WI) select McKesson Analytics Advisor.
Tidewell Hospice (FL) chooses Allscripts Homecare and EPSi financial management.
China-based diagnostic testing vendor Kindstar Globagene Technology chooses PathCentral’s anatomic pathology system for its 2,000 hospital customers in China.
Personal health record vendor MMRGlobal, which runs the MyMedicalRecords.com site, says Surgery Center Management has offered $30 million to license its patents for the PHR, patient video site, and document management system for providers.

CSC says it expects its NPfIT contract will be extended by an extra year through 2017, despite the company’s past problems delivering implementations on schedule that contributed to the cancellation of the $19 billion project. CSC expects to earn up to $3 billion for the 12-month extension. The former CIO said CSC would probably sue if its contract was cancelled, concluding that it might be cheaper just to pay them.
People
Medical documentation software provider Emdat hires Michael Grayson (Eclipsys, Sentillion, IDX) as VP of strategic partnerships.




HIMSS adds four members to its board of directors: Dana Alexander, RN, MSN, MBA, FHIMSS (GE Healthcare); Brian R. Jacobs, MD, MS, FHIMSS (Children’s National Medical Center, DC); Kenneth R. Ong, MD, MPH, FACP, FIDSA, FHIMSS (New York Hospital Queens); and Fred D. Rachman, MD, FHIMSS (Alliance of Chicago Community Health Services.)
Encore Health Resources expands its client services leadership team with the hiring of Greg Bluth, Ken Frantz, Jason Griffin, and Jim Kearns.

MED3OOO’s board of directors promotes Carl Smollinger from executive VP of ACO and employer services to COO.
Announcements and Implementations

NYU Langone Medical Center implements IOD’s release of information solution.
Wolters Kluwer Health releases its expanded IPhone app, UpToDate MobileComplete.
University Behavioral HealthCare (NJ) goes live on Stockell Healthcare Systems’ InsightCS Revenue Cycle Information Management platform.
DrFirst partners with Atlas Medical to offer physicians the ability to place lab/rad orders and review results via DrFirst’s Rcopia e-prescribing solution.
Government and Politics
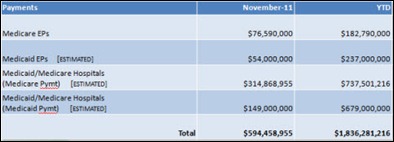
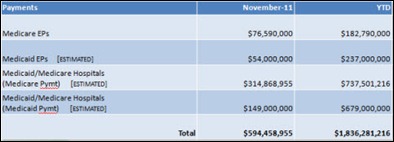
Medicare and Medicaid have paid 2,868 hospitals and 21,425 EPs approximately $1.8 million for the Meaningful Use of EHRs through the end of November.
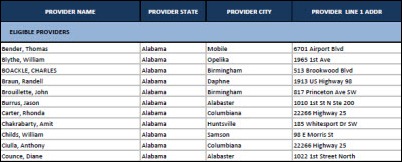
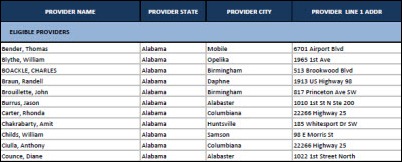
Dr. Jayne mentions below, but here’s a list of all Medicare EPs who have received HITECH money through September 30.
The State Department and the US Coast Guard sign an interagency agreement to share Epic’s EHR and access to VLER, the EHR used by the US Armed Forces EHR for its current and retired members.
Other
VA employee unions raise concerns that a plan to add RTLS technology will lead to staff monitoring. The VA is issuing a $550 million draft request for proposals for RTLS to interface with cleaning and sterilization equipment. The department claims it has no official plans to tag and track employees. One union representative views any plans to use RTLS to track employees as “the beginning of Big Brother” and “and invasion of privacy.”

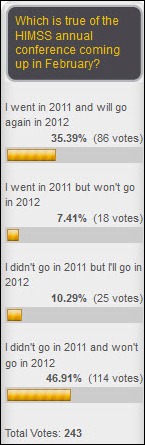
Meditech announces it will return to the HIMSS conference this year as an exhibitor. In looking at the HIMSS conference site, it does not appear that Cerner will be following Meditech’s lead in coming back.
Programmers world-wide celebrated last weekend with Random Hacks of Kindness, where self-proclaimed hackers developed programs for humanitarian purposes. Among them were an emergency response system for the Samoan Islands, a real-time disease tracking system, and an app that can scan a photo of water-borne bacteria to determine if it’s safe to drink.
The FBI subpoenas several businesses in its investigation into the financial dealings of Wayne County, MI. Among the companies whose contracts are being reviewed is Strategic Business Partners, a Detroit IT company that has billed the county for $22 million over several years, some of that for developing EMR software for the county jail.
A hospital in Canada being sued for malpractice by a patient who suffered a stroke during surgery tries to convince a judge to give it access to the patient’s Facebook and Twitter accounts, her computer, and her iPhone. The hospital’s argument was that since the patient claims her health and enjoyment of life had been harmed, they should be able to look for evidence to the contrary. The judge said no, calling it “ a classic fishing expedition without the appropriate bait.”
Sponsor Updates

- The Advisory Board Company’s Crimson business unit wins the Best Booth award at the IHI forum in Orlando, with recognition of its employees for their knowledge and demonstration skills.
- GE Healthcare releases a white paper that highlights the use of Centricity Practice Solution to achieve Meaningful Use requirements.
- Healthwise launches Healthwise Spanish Knowledgebase, which includes evidence-based health information.
- Symantec Health and DrFirst will present at April’s EPCS Leadership Symposium.
- Blanton Godfrey, co-founder of the Institute for Healthcare Improvement, keynotes at TeleTracking Technologies’ 2011 Client Conference and predicts that better workflow choices will determine winners and losers after health reform.
- DIVURGENT releases a white paper on the selection of the right IT infrastructure for ACOs.
- The Irish Health Service Executive announces that four of its 35 hospitals are live on McKesson’s Horizon Medical Imaging PACS, with the remainder coming up within 20 months.
- T-System’s CMIO Robert Hitchcock MD and CFO Steve Armond CFO discuss how to use IT to make an emergency department profitable.
- Lawson Software introduces Infor10 Lawson S3, which includes integration between Lawson technology and products and applications from its newly acquired company Infor.
- e-MDs customer James F. Holsinger, MD, PC wins the 2011 HIMSS Ambulatory Davies Award of Excellence for the quality of patient care through practice’s Meaningful Use of EHR.
- MedVentive was selected to participate in last month’s Mid-West BluePrint Health IT Innovation Exchange Summit.
- Intelligent InSites posts congratulations to President and CEO Doug Burgum, who is also chairman of the board of the SuccessFactors, just acquired by SAP for $3.4 billion. He was also an early investor and leader of Great Plains Software, which Microsoft acquired for $1.1 billion in 2001.
EPtalk by Dr. Jayne
HIPAA 5010 report: just a tad more than three weeks left until the January 1, 2012 deadline. Although CMS has announced that it won’t enforce compliance until March 31, don’t let the extension fool you. Many in the industry are predicting transaction rejections and cash flow interruptions to those who are not ready. CMS will be looking for non-compliant physicians who are expected to provide proof that they are preparing to be fully compliant.
It’s National Influenza Vaccination Week through Saturday. I’ve been impressed by the Centers for Disease Control and its use of social media (they had me at the Zombie Apocalypse.) Hospitals and health systems are steadily moving towards making vaccination a condition of employment whether you’re in direct patient contact or not. Several of the “IT guys” I work with always complain about it since they don’t work in the hospital proper and I usually have to remind them it’s not just about patients, but also about lost workforce productivity and increased healthcare costs. People do still die from the flu and it’s recommended this year for everyone age six months and older. Please get your flu shot, especially if you’re in a high-risk group.
The American Medical Association publishes a “How To” guide for Accountable Care Organizations and Co-Ops. Chapter Six includes advice on EHR incentive programs. It’s not a bad read for those who either have been living under a rock the last several years or just need a refresher on the basics. I like the chapter’s closing paragraph:
As is clear from this chapter, the adoption of a certified EHR system and the achievement of Meaningful Use is a very arduous task. Eligible professionals should remember that the incentives or penalties that are the consequences of this task are not insignificant.
Speaking of Meaningful Use, if you’re a Safety Net provider, I thought this upcoming webinar from the Health Resources and Services Administration (HRSA) looked interesting: Tips for Overcoming the Gray Areas of Meaningful Use for Safety Net Providers. At least someone is admitting there are some gray areas. Presenters from Regional Extension Centers and CMS will review “problem areas” that include vendor relations, attestation, and troubleshooting quality measures. It’s December 13 at 2 p.m. EST. You can send questions in advance to healthit@hrsa.gov.

CMS has a new web page that shows MU incentive payment and registration data through October 2011. Maps show payment and registration breakdowns by state as well as individual state reports of registrants and payments. For those of you who want to know if your colleague in the doctor’s lounge was just blowing smoke, here’s the list of those who have already received payments.
There was an announcement earlier this week that Medicare will allow mining of its claims database for the purpose of creating report cards on providers. Employers, insurers, and consumer groups will have access to the data and physicians will be individually identifiable. People have been after this data for a long time, but I’m not sure how useful it will really be. There are so many other factors that go into determining quality other than sheer volume and claims data. One prominent hospital I worked at appeared on some payer reports as having poor numbers for morbidity and mortality for certain high-risk procedures. Once the case mix was analyzed, it was apparent that this tertiary referral center really did have patients that were sicker than average and also that they were willing to attempt procedures on patients so sick that other facilities wouldn’t even consider it. We’ll just have to see what comes out of the data.
I’m back from the rodeo and settling back into the daily routine of crunching quality reports of my own, as well as doing never-ending upgrade planning and dealing with ever-cranky colleagues. I do have something big planned for next week, but you’ll have to keep reading to find out what it is. Let’s just hope it doesn’t end up involving law enforcement or a bail bondsman.
Have a question about Meaningful Use, CMS, or whether the wearing of red Rocky Mountain jeans really says something about a girl? E-mail me.

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.

































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…