Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
News 3/26/10
From Soft Sales: “Re: Microsoft Amalga. Robert Seliger, former CEO of Sentillion, will take over sales. This was announced internally on 3/15.” Not exactly, but close. Per my Microsoft contact, former Sentillion president Paul Roscoe will lead the sales organization of Microsoft Health Solutions Group, integrating the sales teams of HSG and its recent Sentillion acquisition. Steve Shihadeh will report to Paul. This is quite interesting — obviously Microsoft had a lot more respect for Sentillion than just buying its single sign-on and context management technologies. Putting someone with healthcare sales experience in charge is a good move if you ask me — we’re not talking shrink-wrapped retail sales here.
From UKnowMe: “Re: CSC. Is it putting itself up for sale? Or at least its healthcare biz?”
From All Hat No Cattle: “Re: NIST. Looks like they are still disregarding system usability.” NIST’s Health IT Standards and Testing page outlines its testing programs, none of which appear to involve usability. Of course, there’s already a measure of that: low adoption.
From OhWell: “Re: Epic installs. UKnowMe is right, Epic is selling like mad. Rumor has it that Epic is looking to hire 500+ people by the end of the summer. So much for experienced implementers or even experienced advisors with the time to focus on each install.” People have been saying for years that Epic, like Cerner and everyone else before it, will eventually hit a wall. It hasn’t happened yet, but competitors are hoping they’ll run out of steam. Of course, they aren’t really doing much to give Epic a run for their money, either.
From Mark Moffitt: “Re: HISsies award for service oriented architecture as the most overrated technology. I’m a big advocate of web services, aka SOA, as a catalyst for change in HCIT. That being said, I have to agree with the award above. Vendors may be embracing SOA under the hood, but very few vendors expose services so customers can take advantage of the technology. As a result, the impact has been muted from a customer perspective. Until vendors make services available to customers and other vendors, like: get_data(patient, med_list) or: go_do_something(patient, order, md), the HCIT public will continue to view SOA as an ‘overrated technology.’ I continue to plead with vendors to expose services. Unfortunately, I get the response, ‘When customers start demanding it, we will provide it.’ Well, I’m demanding it. How many more have demanded it and gotten the same response? Or they offer it but not to customers, only partners that don’t provide a competing product. The push back I hear from vendors is ‘we don’t want to be held liable.’ Really? If I repair my car and install brakes incorrectly, have an accident and crash into another vehicle, is the victim going to sue Ford, or Toyota, or GMC and win? I don’t think so. A simple release agreement that relieves a vendor of liability is all it takes. I’d like to hear from vendors on this topic.”
Inga’s been busy again, as you’ll see tomorrow when she posts our latest executive Q&A series entry. A dozen or so industry executives answered this question: “Now that the ONC has announced the initial grants for Regional Extension Centers, what will be the effect on EHR selection and implementation for both the industry and your company in particular?”
Listening: Luscious Jackson, reader-recommended, all-female pop with hip-hop influences. Defunct for a few years, but I’m pretty crazy about them.
UCSF names Elazar Harel as vice chancellor for IT and CIO, which includes dotted line responsibility for the CIO of UCSF Medical Center, fresh off a failed Centricity implementation.
Dave Garets and Mike Davis, the two top guys at HIMSS Analytics, start their new gigs with The Advisory Board Company on Monday. HIMSS says it will replace them.
Richard Ferrans MD, CMIO of Memorial Hospital of Gulfport (MS) will talk about the Mississippi Coastal HIE in a Medicity Webinar on Wednesday, April 14.
DEA publishes an Interim Final Rule on e-prescribing of controlled drugs (warning: it’s a 334-page PDF). There’s the usual 60-day comment period. I haven’t studied it yet, but if anyone wants to summarize whatever is interesting in all those pages, feel free to send me your thoughts.
Researchers in France begin a project to identify patients at risk for hospital-acquired infections by scanning electronic medical records with a Xerox text mining tool called FactSpotter.
Sisters of Charity Health System (OH) names Robin Stursa to the newly created position of VP/CIO. She was previously at Saint Vincent Health System (PA).
An opinion piece by Deborah Peel, MD of Patient Privacy Rights called Your Medical Records Aren’t Secure runs in the Wall Street Journal.
There is no need to choose between the benefits of technology and our rights to health privacy. Technologies already exist that enable each person to choose what information he is willing to share and what must remain private. Consent must be built into electronic systems up front so we can each choose the levels of privacy and sharing we prefer. My organization, Patient Privacy Rights, is starting a Do Not Disclose petition so Americans can inform Congress and the president they want to control who can see and use their medical records. We believe Congress should pass a law to build an online registry where individuals can express their preferences for sharing their health information or keeping it private. Such a registry, plus safety technologies for online records, will mean Americans can trust electronic health systems.
Bonnie Siegel, formerly of Dorenfest and Hersher Associates, joins HIT executive search firm Sanford Rose Associates.
UC Irvine researchers are developing Telios, a Web-based telepresence system that will offer videoconferencing and remote patient monitoring tools.
Ironic beneficiaries of healthcare reform: offshore business process outsourcers, which are even more attractive when administrative cost-cutting gets serious.
A tidbit from the trial of the former CEO of University Medical Center (NV), accused of squandering $11 million on no-bid contracts: one contractor got $850K for producing a 30-minute PowerPoint describing an IT system the hospital already owned.
Red Hat announces Q4 numbers: revenue up 18%, EPS $0.12 vs. $0.08.
HERtalk by Inga
Earlier this week, Mr. H mentioned that The Kansas City University of Medicine and Biosciences and its former president are suing one another. A local paper points out that former president Karen Pletz is now better known than she was before the firing. That’s because there are plenty of people (like me) who are drawn to the salacious aspects of the story. On the one hand, we have the medical school, which claims Pletz abused her expense account, racking up $2.3 million in food and travel charges.Then we have Pletz, who counters that she’s a victim of conspiracy, aimed at making her the scapegoat for a board that was paying her a huge salary ($1.2 million a year) and approving hefty entertainment expenses. Someone’s hiding something and it all makes for a juicy trial.
Another not-for-profit hospital system agrees to be acquired and transformed to a for-profit entity. Caritas Christi Health Care says that private equity firm Cerberus Capital Management is buying the six-hospital system for $830 million, which includes $430 million to pay off debt and $400 million on major improvements, such as upgrades to IT systems.
Masonicare Healthcare Center (CT) agrees to deploy MED3OOO’s InteGreat EHR for the physicians serving its facility.
Vanderbilt University Medical Center selects Accelarad’s SeeMyRadiology.com service, giving orthopedic surgeons the ability to exchange medical images in real-time via the Web or a mobile device.
Allocade, a developer of patient flow software, closes a $5 million round of VC financing led by VantagePoint Venture. Allocade intends to use the money to expand operations to meet the increased demand for its On-Cue solution.
The ONC appoints Aaron McKethan and Craig Brammer as the new program director and deputy director of its Beacon communities project. The project will award about 15 grants to non-profit organizations or government bodies to help them achieve meaningful use of their EHRs. McKethan is a research director at the Brookings Institution’s Engelber Center for Health Reform and Brammer is a project director at Cincinnati’s Aligning Forces for Quality.
CareTech Solutions and ForeSee Results announce they’ve formed a strategic partnership to provide CareTech’s hospital clients with an online customer satisfaction measurement and monitoring tool.
ICA vice president John Tempesco is named a Fellow of the American College of Healthcare Executives.
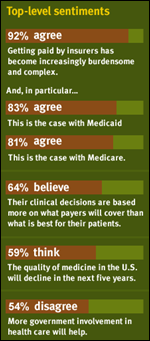
Sermo and athenahealth release results from a Physician Sentiment Index that indicates doctors aren’t too happy with the business of medicine. A couple of the more disturbing findings: 59% of physicians think the quality of medicine will decline in the next five years and 64% agree their clinical decisions are being based more on what payors are willing to cover than what they think is best for their patients. Sermo CEO Dr. Daniel Palestrant explains the results in more detail in this CNBC interview.
March 25th is National Medical Biller’s Day, according to the American Medical Billing Association. Thank you, billers, for keeping the money flowing!
Sixteen Harris County Hospital District employees who were fired for HIPAA violations in November get their jobs back. Hospital district administrators reassessed the intent of the violation and reinstated the workers’ jobs, though no back wages will be paid. The firings occurred after one of hospital’s medical residents was shot in a grocery store parking and became a patient at the hospital. The medical resident survived.
GE acquires MedPlexus, an EMR PM vendor that targets the 1-10 physician practice market. My first thought was why would GE make this purchase given that they already have the Centricity product? However, if I recall my ambulatory EMR history correctly, Centricity EMR is not truly integrated with a practice management product, but interfaces with either the Centricity Practice Solution (the old Millbrook product) or Centricity Enterprise (the old IDX software). MedPlexus, however, appears to be a fully integrated PM / EMR / patient portal solution. It’s also a hosted product, which is possibly a more attractive and affordable solution than GE’s traditional client/server options. And, Centricity EMR has not had stellar KLAS ratings in the last couple of years, so perhaps GE needed a fresh option.
CentraState Healthcare System (NJ) contracts with Design Clinicals to implement MedsTracker patient medication management. CentraState went live December 7th and says they’ve cut medication reconciliation time from about three minutes to one minute 38 seconds.
Dell unveils its Medical Archiving Solution, which is based on its upcoming Dell DX Object Storage Platform. Dell hopes the new technology will appeal to hospitals needing to increase storage for growing EMR and digital imaging systems.
Huntsville Hospital (AL) selects MedAssets’ RCM solutions for claims management and claims audit and resolution.











I guess if Microsoft can make billions selling a horrible OS, why can’t EPIC make millions selling decades old technology. Does anybody really understand what they are buying. I feel like we are at a flee market.
Re: Oh Well on Epic hiring 500+.
They’re 3500 people, so factoring in some turnover at say 5% – that’s 175 people and some modest growth to be prepared for the industry starting back up, it doesn’t seem outrageous.
They have been on record with customers through the last 10 years having some years where they’ve hired 300 to 700 staff.
I suspect they’ll be just fine.
Re: Mark Moffitt :”I’m a big advocate of web services, aka SOA, as a catalyst for change in HCIT… but very few vendors expose services so customers can take advantage of the technology. … Until vendors make services available to customers and other vendors, like: get_data(patient, med_list) or: go_do_something(patient, order, md), the HCIT public will continue to view SOA as an ‘overrated technology.’”
Well, where to start… A Service Oriented Architecture is an architecture, not a technology. Also, note that it is *A* Service Oriented Architecture, not *THE* Service Oriented Architecture, because it has to be defined in a top down fashion, for the purposes of a particular business or organization. Especially jarring is the stated equivalence between web services (a technology) and SOA (an architecture). A lot of good information can be found at http://hssp.wikispaces.com/HSSP+Information+Center – see slide 17 of the Intro for a comparison between SOA and web services.
My guess is that at least some vendors would react to the statement above with the thought “well, the customer does not really understand all these buzz-words, do they actually know what they want?”
For the sake of discussion, let’s assume an organization has decided to build a service oriented architecture, and that the underlying technology will be SOAP web services. Now the request for the vendors will be much clearer, and the discussion on what services are needed, what parameters, what context, etc. can proceed.
Given the above assumptions, let’s look at one of the examples: get_data(patient, med_list) – let’s assume that the meaning of this service is, for a given patient, give me the list of medications. How do we identify the patient? Well, we are within a single organization, let’s assume there is a master patient identifier. So the first parameter for this service is the master patient ID. This means that before this service is called, the user of the service must somehow obtain the master patient ID – this likely means use another service.
So now my architecture must account for the orchestration of two services, get_patient_ID, and get_data for the medication list. Now I have an issue – if someone uses the get_patient_ID service, how do I determine that that someone is allowed to get the patient ID? When I do my service orchestration, do I need to tell the get_patient_ID service that I need it to obtain the patient’s medication list, or do I make this a secondary authorization verification, part of the get_data service, based on the fact that the data requested is the medication list? The answer will likely depend based on the architecture design in the organization, and thus the vendor will start facing a differing set of requirements for different customers.
Now let’s look at the second part of the get_data service, the parameter that tells it that we want the medication list. Now, what is the medication list? The current medications? What if the patient is in the hospital, do we include the hospital medications? Do we include canceled medications, or should we make that a different parameter? Do we need to add a parameter to have the current medications as of a given date? Or a couple of parameters, showing all medications for a time period? How about AIDS medications – do we check if the service user is allowed to see those? Should we also include the price of the medications? The patient portion maybe?
I hope this illustrates some of the issues that need to be resolved when discussing SOA… It is important to understand that the organization needs to design and build the architecture, then work with the vendors on determining feasible specification for the necessary services. This includes intimate familiarity with HL7, HSSP, IHE, and to some extent DICOM and X12
It would be interesting to see an article on how reimbursement impacts EMR’s. Historically, charges needed to be moved between encounters. With EMR’s, we now have the challenge of trying to figure out how to move electronic clinical data as well.
Re: Decades old technology.
I’ve heard people make statements like this before – I’ve never really understood it as a criticism. Software that is actively developed and upgraded is never decades old.
The original Warcraft game came out in the mid 90s – is World of Warcraft “decades old” technology? Microsoft Excel is decades old as well.
Just because something was invented/created long ago does not make all current versions of it outdated.
I’ve worked for both Steve Shihadeh and Paul Roscoe, both are consummate professionals but Steve knows more about HIT in his pinky finger than Paul.
Paul is a fine gentleman with charming British etiquette, and a lethal golf game!
Steve is one of the few elevated executives in our industry, down to earth, with no hidden agendas.
I think MS has two excellent executives, fine people with very successful track records.
All the best to these two fine gentlemen!
RE: EPIC – with the economy still weak EPIC has its choice among the best gradautes from the best schools.
Even MEDITECH is able to hire a much higer caliber of employee than was possible a few years ago.
“Re: NIST. Looks like they are still disregarding system usability.”
This is the work of Booze Allen on the lucrative contract described on your pages of yore. Must be more Booze than Allen with a HIMSS chaser and a C$HIT faced cashier. The stuff may look like a f mignon when it really is kangaroo meat.
“Dave Garets and Mike Davis, the two top guys at HIMSS Analytics, start their new gigs with The Advisory Board Company on Monday (March 29) HIMSS says it will replace them. ”
At least they are not starting on April Fool’s Day!
HIMSS staff were told that beginning March 1, 2010, The Advisory Board Company and HIMSS Analytics would “collaborate to provide a new level of business-oriented information technology (IT) research
to health care executives and IT leaders”, and that the data from HIMSS Analytics Database w/b provided to ABC “as the foundation for new and expanded services and projects.”
Most HIMSS staff did not know until yesterday that Garets and Davis were leaving HIMSS Analytics. It was rumored that if HIMSS CEO H. Stephen Lieber were to step down, that Dave Garets would replace him. Garets was “appointed” to HIMSS Analytics in 2004 after he served as HIMSS BOD Chair from 2003-2004.
HIMSS Analytics was originally setup as a “for profit” arm of HIMSS, but now its profits flow through HIMSS nonprofit. HIMSS Analytics is still very profitable for HIMSS, and it is the reason HIMSS is able to use its money to lobby so extensively.
It is no surprise that Garets and Davis have left HIMSS to join a legitimate “for-profit” public company that provides general best practices research, executive education, consulting, and business intelligence solutions to hospitals and health systems.
So does this mean HIMSS is no longer “collaborating” with the Advisory Board Company? It appears everyone is trying to distance themselves from HIMSS, including HIMSS’ CCHIT Chair Mark Leavitt, who retires at the end of this month.
Your blog is very helpful to me. Keep the hits coming Mr H and Inga.
Pomposity and circumcstance at UCSF as shown in the report: “In his new position, Harel will oversee both the academic and administrative IT activities for the campus. The CIO of the UCSF Medical Center will have a dotted-line reporting relationship to Harel, UCSF said, “reflecting the coordination leadership Harel will provide for UCSF IT policies and infrastructure.”
The university has faced nagging delays and budgeting snafus connected with implementation of an electronic medical record system and other IT installations in recent years.
Harel’s broad scope of responsibilities “is unique within the UC system and represents a bold new vision for addressing the opportunities and challenges of information technology,” said Bluestone, who will oversee Harel along with Senior Vice Chancellor for Finance and Administration John Plotts.
The circumstance of how many patients died from Centricity failure is a good one. As for the pomposity, one would think there would be more humility expressed in the UCSF press release, considering the earlier disaster.
In the final analysis, is the new guy fit for the task, and when did he last take care of a patient?
Anonymous:
Are you serious?
>How do we identify the patient?
Is that a serious question?
>This means that before this service is called, the user of the service must somehow obtain the master patient ID – this likely means use another service.
Wow, you are really going out on a limb with that assumption!
>So now my architecture must account for the orchestration of two services, get_patient_ID, and get_data for the medication list.
No you don’t. In this example I’m sending you patient identifier. You don’t need to orchestrate anything. I’m sending you a service request to get a med list and in that service request is a patient identifier. At least in this example.
>Now I have an issue – if someone uses the get_patient_ID service, how do I determine that that someone is allowed to get the patient ID?
That is not the responsibility of the service. It is the responsibility of the program consuming the service to determine if the user is allowed to view that information. The service should have a mechanism that only allows certain services to use the service. There are numerous ways to accomplish this. Pick one and use it.
>When I do my service orchestration, do I need to tell the get_patient_ID service that I need it to obtain the patient’s medication list, or do I make this a secondary authorization verification, part of the get_data service, based on the fact that the data requested is the medication list? The answer will likely depend based on the architecture design in the organization, and thus the vendor will start facing a differing set of requirements for different customers.
It really is not that complicated. Unless you have some other agenda.
It is a simple web service that you have made unnecessarily complicated: Pass in patient identifier, return list of meds. One method would be to return all current meds, PRN meds, and DC meds. Only allow requestors that meet “some security requirement.”
How do you make breakfast in the morning? That seems really complicated too!
Agree with Mark. This is a pretty straightforward and easy request. Granted there are some serious caveats (like the organization actually has a MPI and that it is robust enough from a sensitivity/specificity if homegrown to cut the mustard especially if it is a large organization) but Anon just made this seem much more complicated than it really is.
Mark Moffitt: Yes, I am serious – the purpose of describing these seemingly obvious details is that in many cases they are not that obvious. Also, I did a poor job distinguishing between the “organization” and the “vendor”, so your criticism is warranted…
The first “obvious” detail – that the “patient” parameter is a patient ID is indeed obvious, but there was nothing in the original description of the service to be sure. Then I mis-wrote: “So now my architecture must account for the orchestration of two services, get_patient_ID, and get_data for the medication list” – as you pointed out, it is the organization’s responsibility to do orchestration, and since it is the organization’s architecture, that is what I meant…
[MM]:’It is a simple web service that you have made unnecessarily complicated: Pass in patient identifier, return list of meds. One method would be to return all current meds, PRN meds, and DC meds. Only allow requestors that meet “some security requirement.”’
What suggestions do you have for a method to “meet some security requirement”?
And one more detail – what should the service return? A list of medication codes (NDC, RxNorm)? A text description (XML fragment, XHTML fragment)? A simple data structure (code, text sig, or code, discrete sig)? A complete description of each med (e.g. http://www.hl7.org/v3ballot2009sep/html/domains/uvct/editable/COCT_RM230100UV.htm) An identifier that you can later use with other services to obtain more information about each individual medication?
Lazlo: In order to get to more substantive points, I thought we need to establish some common understanding first. Maybe I didn’t use the best approach, but we got to one point of agreement, I think – the organization that wants to use SOA must build the architecture that suits its needs…
Anonymous:
My initial question was related to vendors (lack of) providing web services to get data and do “stuff.” It was really not about architecture.
Can you identify yourself so readers can understand your POV? Are you speaking from the HCIT vendor side or do you work for or provide services related to SOA?
Mark Moffitt:
I was trying to get to the reasons why you can’t get seemingly simple web services in a structured and logical way, but it got too long and unwieldy…
So I will try to list few reasons, hopefully that will make more sense:
* Vendors are unlikely to structure their application architecture in a way such that the equivalent of a simple get_data(patient, med_list) method exists.
* The security and use context are critical in maintaining data integrity, and translating that context from an application architecture to a web services environment is not trivial.
* Different customer requirements are likely to require different granularity of web services; maintaining multiple service layers only complicates software development.
Moffitt and anonymous are in to self serving sales. Too bad that none of these products are fit for purpose, patient care that is.
They are fit for ringing up upcoding on the cash register since it is a matter of one swift click of the mouse to move a full past history, review of systems, med lists, etc from progress note to progress note and bill the highest codes.
There are clinics that have the patient fill out a 10 page history check list (sounds like CCHIT Certification) before they could see a doctor. The doctor spends a few minutes reviewing the HPI and examines the patient.
The hourly minimal waged clerk clicks in the patients’ checks and there you go, a complete level 5 H and P.
That is meaningful use! Notify Blumenthal to add this one.
Anonymous:
That wasn’t so hard was it? I mean answering the question in a straightforward manner.
I don’t agree with what you wrote but at least you wrote in response to my question and didn’t go off on another rant.
I’m curious, why don’t reveal who you are or, at least, your experience with web services and SOA in healthcare? Your comments suggest to me you have read about web services and SOA, maybe “Googled and cut-and-paste” your initial response, but have never written a line of code. But I open to being proved wrong on that assessment.
Suzie RN:
“Moffitt and anonymous are in to self serving sales. Too bad that none of these products are fit for purpose, patient care that is.”
I work for a provider organization and am looking for ways to extend the functionality of HCIT systems. I’m curious, why do you think I’m trying to sell something? Maybe because I have a strong opinion on what I write and the only reason I take the time to respond is because I’m looking to make money?
The reason I take the time is because I’m not satisfied with the current state of HCIT and am passionate about improving and innovating to improve the state of HCIT.
Nursing is not the only profession in healthcare that passionately care and want to improve outcomes through hard work and dedication to the healthcare profession. People like me have the same passion as Nursing professionals but do the work “behind the scenes.” We are just as dedicated.
It’s not really about the money. I suspect there are many others who read this site that are like me.
Hey Mr. H…
I think you should have Moffit & Anon do separate ‘Readers Write’ essays on their points of view. A nice point – counter point piece. Of course with both clearly identified…
To the Moffitt who said “I work for a provider organization and am looking for ways to extend the functionality of HCIT systems.”
That is all well and good. When did you last take care of a patient?
Do your doctors and nurses complain of the hazards constructed for their care and their patients? Never? Do you report adverse events to the FDA and ISMP?
One of the blogs had a letter from amother nurse from Canada
commenting on your ilk. I think it may have been on Dr. Silverstein’s site.
Suzy, RN:
Interesting comments:
“When did you last take care of a patient? Do your doctors and nurses complain of the hazards constructed for their care and their patients? Never?”
“…. another nurse from Canada commenting on your ilk.”
Your comments reveal much about your POV and your attitude towards those in healthcare that are not involved in direct patient care.
If I were to categorize you it would be an older nurse who resents the changes taking place in healthcare and IT is a convenient target for you to focus your anger. Long for the day of yesteryear when life was much simpler and “change”, and a coke, was what you got back from a quarter that you put in the “soda machine?”
Mark Moffitt:
You are free to assume whatever you want, please provide your reasons why you disagree. If you would like me to clarify my answers further, please let me know. My identity or qualifications are irrelevant if my statements cannot stand on their own.
Anonymous, Statements are well and clear but the reasons behind the statements must also be known so they can be taken into context. Having worked for both a vendor and a provider organization there is a vast difference in the methods taken to obtain a goal and a gulf between identifying goals.
HISJunkie, I must agree with you, a “debate” of sorts would prove intriguing to read.
Mark, this morning I heard someone comment that we’ve all got to find something in life that makes us angry so that we can have the energy to fight to make a difference. I prefer your description of passionate.
However, I do feel that you dismissed Suzy very quickly, one of the most obvious issues between IT departments and the IP floors is their lack of respect for one another. Suzy may have a bone to pick (or she may not) but that does not mean from her viewpoint things shouldn’t be different.
She feels [strongly] that those in IT cannot understand patient care without being a provider. Personally as someone with no patient care background that’s difficult for me to swallow. However, I cannot change anyone’s mind in regards to my understanding patient care and entering data and the frustration of learning a new system while juggling 15 different tasks without first being willing to listen to their concerns and empathize with them.
Suzy, RN: I have difficulty taking your concerns seriously if you choose to use loaded terms such as “ilk” when Mark has responded politely enough that he does work for a provider organization and is endeavoring to improve his system.