Top News

A GAO report finds that the VA and DoD have made progress in their pilot project to integrate care at the James A. Lovell Federal Health Care Center (IL), but delays in implementing the IT component have resulted in additional costs. IT investments have already surpassed $122 million and some initiatives are almost two years behind schedule.
Reader Comments

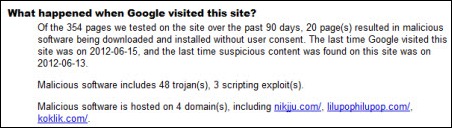
 From Convener: “HIStalk’s announcement on the Supreme Court ruling. Once again you beat Modern Healthcare and all the others, and with a more comprehensive article.” Since Mr. H is busy traveling for his hospital job, we decided in advance that I would sit by computer and TV, listen for the announcement, and send readers a quick update. The moment MSNBC said the healthcare law had been upheld, I looked for an online write-up. Above is a screen shot of what CNN posted, which obviously left me mighty confused (obviously several so-called journalists hit the “post” button for their pre-written stories after reading only the first sentence of the ruling.) Thankfully I decided CNN simply had it wrong before I blast the news incorrectly to the HIStalk universe. Boy, Mr. H would have never let me live that down.
From Convener: “HIStalk’s announcement on the Supreme Court ruling. Once again you beat Modern Healthcare and all the others, and with a more comprehensive article.” Since Mr. H is busy traveling for his hospital job, we decided in advance that I would sit by computer and TV, listen for the announcement, and send readers a quick update. The moment MSNBC said the healthcare law had been upheld, I looked for an online write-up. Above is a screen shot of what CNN posted, which obviously left me mighty confused (obviously several so-called journalists hit the “post” button for their pre-written stories after reading only the first sentence of the ruling.) Thankfully I decided CNN simply had it wrong before I blast the news incorrectly to the HIStalk universe. Boy, Mr. H would have never let me live that down.
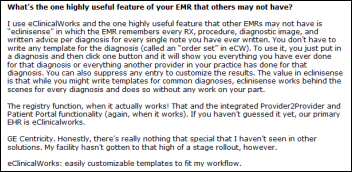
 From SummerFun: “HIStalk Practice Advisory Panel. I liked the write-up. Great questions and interesting answers.” In case you missed it, our first HIStalk Talk Practice Advisory Panel post was published earlier this week. The participants, who are primarily physicians and staff in ambulatory care practices, shared thoughts on their EMRs and discuss other technologies. It’s a fun read and a good mix of positive and negative impressions, just like real life.
From SummerFun: “HIStalk Practice Advisory Panel. I liked the write-up. Great questions and interesting answers.” In case you missed it, our first HIStalk Talk Practice Advisory Panel post was published earlier this week. The participants, who are primarily physicians and staff in ambulatory care practices, shared thoughts on their EMRs and discuss other technologies. It’s a fun read and a good mix of positive and negative impressions, just like real life.
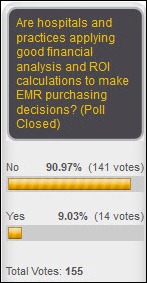
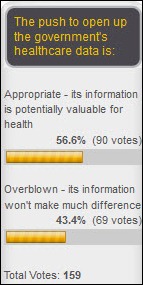
From Blue Eyes: “Re: healthcare reform act. What do you think of the news and its effect on healthcare IT?” I think people have forgotten that Thursday’s ruling affirmed only the legality of creating the law, not to assess it as a good or bad idea. I’ve yet to hear anyone claim to have read and/or understood the 2,900 pages of legalese, including the politicians who voted for or against it, and it’s discouraging that even the Supremes voted pretty much along liberal / conservative lines (it’s either legal or it’s not, but you wouldn’t know that from the 5-4 opinion). I don’t know if anyone of us know what it means beyond lots of newly insured people showing up at the doors of hospitals and practices (at least when they can find a primary care provider to schedule them). I’d bet healthcare costs will continue to go up, healthcare IT will ramp up for another year or two until the Meaningful Use wad has been shot and providers go back to buying only what boosts their productivity or bottom line, and we’ll nonetheless start getting some highly useful big-picture data telling us where we stand from a population health perspective but leaving us to actually do something about it (like finding a way to get Americans to lose weight, exercise, and manage their expensive chronic conditions wisely and cost effectively). Here’s where the crowdsourcing thing works well: click the Comments link at the bottom of this post and tell me what you think. For those who have never commented, you don’t have to register first and you can give a phony name to stay anonymous. My general assessment when wearing my HIT tunnelvision goggles is that it’s a good thing. As a taxpayer, I’m not really sure.
From Watcher of the Skies: “Re: HCA. Going Epic. I was in training in Verona and someone from HCA in my class said so.” Unverified. HCA originally said they were doing a one-hospital Epic pilot to decide between it and upgrading Meditech, but nobody’s told me definitively which way they’re going.
From Robbie Douglas: “Re: McKesson. Close to making an acquisition of [company name removed], whose offerings include an ambulatory EHR and billing and management services.” I removed the company’s name since the rumor is unverified, but it sounds like a done deal. It’s a pretty big outfit.

From Cool Runnings: “Re: Drex DeFord. Leaving Seattle to take CIO position at Steward Health in MA. Steward’s for-profit 80-hour work weeks have taken their toll on a few CIOs in a short period of time. The CEO likes to call his leadership on weekends and expects them to work as many hours as he does.” Drex has updated his LinkedIn profile to list the Steward CIO job, so I’ll call that rumor verified. I worked for a for-profit hospital chain once for a short time. It was run by the biggest scumbags in the industry given my first-hand observation of their indifference to patient care and total worship of the bottom line. I wouldn’t care to repeat the experience, but to each his own.
HIStalk Announcements and Requests
Here’s some highlights from the last week on HIStalk Practice, in addition to the above-mentioned post from our Practice Advisory Panel: the biggest challenges of running a group practice. Alleviant announces plans to open a new facility in Vermillion, NC. The Office of the Inspector General finds that EMRs from Allscripts, eClinicalWorks, and GE Healthcare were products most widely used by physicians to document E/M services. Humana is the top payer among US health insurers in athenahealth’s Payerview Rankings. Aaron Berdofe discusses the federated model in the second part of his series on healthcare infrastructure data models. It takes so little to make me happy: a glass of nice wine, a new pair of strappy sandals, or a few new subscribers to HIStalk Practice. Make me merry, if you can. And thanks for reading.
On the Jobs Page: Software Engineering Manager, Project Manager, Web User Interface Design Engineer, Senior Buyer – Third Party Labor.
Listening: Lush, underrated alt rockers from England who had a 10-year run that ended in the late 1990s when their drummer killed himself. The music is rich, sweeping, and sweet, but rocking in a wistful sort of way (some place them in the “shoegazer” genre, but I’m not sure about that). I don’t know how I missed them, but it’s not too late since it still sounds fresh today. You’ll like it if you enjoy Cocteau Twins.
Everybody’s talking about voting of one kind or another these days, so here’s an urge to visit the (electronic) polls. Register to vote by signing up for e-mail updates. Cast your vote for progress by liking, friending, and connecting with the HIStalk party (Inga, Dr. Jayne, Dr. Travis, and me) via the social media ballot boxes. Send us your tired, you poor, and your rumors and news. Show your appreciation of our supporters by checking out the sponsor ads to your left and trying out the searchable, categorized Resource Center and Consulting RFI Blaster. As Alice Cooper says, I’m your top prime cut of meat, I’m your choice, I wanna be elected – as HIT’s go-to site for news, scandalous rumors, and occasionally irrelevant amusement. Thanks for your vote to keep me in (my upstairs spare bedroom) office for another bunch of years – I won’t let you down. I’m Mr. HIStalk and I approved this message.
Acquisitions, Funding, Business, and Stock
Practice Fusion secures an additional $34 million in Series C funding led by Artis Venture. The company has raised $64 million since it launched in 2007.
Carena, which offers webcam-based provider visits and other products, completes $14 million in financing led by Catholic Health Initiatives.
People

The Digital Pathology Association appoints Sharp HealthCare CIO Bill Spooner to its board.


Employee scheduling software vendor Avantas announces the promotion of Christopher Fox from SVP of growth and innovation to CEO and Jackie Larson from VP of client services to SVP. Fox takes over for founding CEO Lorane Kinney, who is retiring.


athenahealth appoints Charles D. Baker (General Catalyst Partners) and Jacqueline B. Kosecoff, PhD (Moriah Partners/Warburg Pincus)to its board.
Announcements and Implementations
Hoag Memorial Hospital Presbyterian (CA) implements Unibased’s ForSite 2020 RMS resource management and patient access solution across all of its diagnostic imaging locations.
The Pennsylvania eHealth Collaborative announces a grant program that gives providers a free year of DIRECT messaging services for secure health information exchange.
RiverView Health (MN) will go live on Epic July 1.
Ochsner Health System (LA) will go live on Epic this week ad its health center locations.
Government and Politics
Five senators introduce a bill that would create a national standard for notifying affected individuals about information security breaches. The bill, the fourth attempt to create national requirements, would also move enforcement to the Federal Trade Commission and allow that agency to levy fines of up to $500,000.
Other
The Bethlehem Area School District (PA) joins The Children’s Care Alliance, which maintains an EMR database of student health data supplied by school districts and made accessible to area hospitals.
Meditech President and CEO Howard Messing provides the opening remarks for the 11th Annual Pappalardo Fellowships in Physics Symposium at MIT, which is obviously supported by Neal Pappalardo of Meditech. Both are MIT alumni and physics fanboys. It’s a good talk.
Highline Medical Center and Franciscan Health System (WA) announce plans to explore a strategic affiliation, partly driven by Highline’s interest in using Franciscan’s Epic system that will go live next year.
University of Texas MD Anderson Cancer Center (TX) notifies patients that a computer containing patient and research information was stolen from a physician’s home April 30. The hospital says it will step up efforts to encrypt its computers, making you wonder how an organization as smart and rich as MDACC needed negative press to finally move the needle on encryption. Here’s a gentle nudge for their fellow fence-sitters: if you don’t encrypt your portable devices, you are being inexcusably irresponsible and deserve the inevitable headlines, CIO firing, and class action lawsuits that are likely to result when the “pay me now or pay me later” time bomb you allowed to be planted finally goes off. Everybody knows that healthcare IT is stuck in a 1980s time warp, but are we seriously still waffling on encrypting PHI-containing devices?
Meanwhile, the Alaska Department of Health and Social Services agrees to pay HHS $1.7 million to settle possible HIPAA violations stemming from the,theft of a USB hard drive from an employee’s car. The Office of Civil Rights determined that the Alaskan agency had inadequate security and risk controls in place and now must take corrective action to safeguard electronic PHI.
Is that a parachute in your backpack or are you just glad to see your surgeon? Mexican doctors remove a 33-pound tumor from the back of a two-year-old, 26-pound boy.
Sponsor Updates
- ICA announces that the Central Illinois HIE is live, with four up and running.
- Kony Solutions expands support of open standards with the release of its KonyOne Platform v5.0.
- Phoenix Children’s Hospital (AZ) chooses Access Intelligent Forms Suite to integrate data among its Allscripts HIS, electronic forms, and its MedPlus ChartMaxx content management application.
- Kareo releases a free iPhone app for accessing physician schedules online.
- Ingenious Med explains how its PQRS Registry is helping healthcare facilities to avoid penalties and improve revenue.
- Medicomp Systems CEO Dave Lareau discusses five EHR considerations for organizations preparing for ICD-10.
- Julie Corcoran, principal consultant with Hayes Management Consulting, highlights five of the major issues facing hospital revenue cycle teams.
- MyHealthDIRECT expands its partnership with Amerigroup to include Amerigroup’s Maryland provider partners and giving them access to MyHealthDIRECT’s online scheduling services.
- Wolters Kluwer Health announces that Essentia Health (MN) is the 1,000th customer to deploy its ProVation Medical software.
- BridgeHead Software releases the results of a survey finding that only 26% of worldwide HIT leaders have robust disaster recovery plans in place.
- Centracare Health System’s St. Cloud Hospital (MN) selects Merge PACS.
- New York eHealth Collaborative says it’s the first REC to hit 1,000 providers qualifying for Meaningful Use money.
EPtalk by Dr. Jayne
Like Inga and Mr. H, I sometimes become annoyed when my day job cuts into my HIStalk time. Unfortunately, this is one of those weeks. I had taken some time off this week to make sure I would be able to immediately respond to the much-anticipated Supreme Court decision, but it has been sucked up by a couple of hospital projects that have gone off the rails. I’ll definitely be responding to the decision, whatever it may be, but just not tonight.
HIStalk reader and contributor Micky Tripathi writes about “The Dangers of Too Much Ambition in Health Information Exchange.” He warns of over-architected HIEs that try to be all things to all people at the expense of short-term wins with real value. It’s a great piece that I hope obtains wide readership.
CMS will begin enforcing the use of version 5010 HIPAA transactions next week. Although it doesn’t seem there are continued widespread issues, anecdotal reports include ongoing tales of claims difficulties.
Physicians are subject to as many as 20 different varieties of payer audits. The American Medical Association has archived a webinar that covers the who, what, where, when, and why of auditing. Anyone who wonders about the high cost of health care and declining levels of provider satisfaction should take a peek.
No surprise: An online article in the Journal of the American Medical Association discusses the higher per-patient operating costs found in clinics with higher medical home scores. Medical homes can reduce overall health care spending, but there is little incentive to incur the upfront burden if the savings isn’t passed to those doing the work.

For Inga: a chocolatier says the Massachusetts pharmaceutical gift ban is hurting its business. Their popular corporate gift: chocolate shoes.
PremierConnect debuted this week, allowing providers and healthcare systems to access data from payers, claims, lab, billing, and other sources to monitor clinical performance and perform predictive modeling. The aggregated database includes data from more than 2,600 hospitals.

I was in Canada recently and heard quite a few public service announcements on the radio encouraging blood donors to step up and give. I haven’t heard much at home, but blood supplies in the US have reached “emergency levels,”according to the Red Cross. Summer heat and vacations typically limit donations and only 3% of people in America donate blood. If you’re looking for an air-conditioned place to spend some time over the upcoming holiday, consider taking a trip to your local blood bank. Chances are you’ll leave with a cookie and some orange juice in addition to knowing you may have just saved a life.

Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.










 From Convener: “HIStalk’s announcement on the Supreme Court ruling. Once again you beat Modern Healthcare and all the others, and with a more comprehensive article.” Since Mr. H is busy traveling for his hospital job, we decided in advance that I would sit by computer and TV, listen for the announcement, and send readers a quick update. The moment MSNBC said the healthcare law had been upheld, I looked for an online write-up. Above is a screen shot of what CNN posted, which obviously left me mighty confused (obviously several so-called journalists hit the “post” button for their pre-written stories after reading only the first sentence of the ruling.) Thankfully I decided CNN simply had it wrong before I blast the news incorrectly to the HIStalk universe. Boy, Mr. H would have never let me live that down.
From Convener: “HIStalk’s announcement on the Supreme Court ruling. Once again you beat Modern Healthcare and all the others, and with a more comprehensive article.” Since Mr. H is busy traveling for his hospital job, we decided in advance that I would sit by computer and TV, listen for the announcement, and send readers a quick update. The moment MSNBC said the healthcare law had been upheld, I looked for an online write-up. Above is a screen shot of what CNN posted, which obviously left me mighty confused (obviously several so-called journalists hit the “post” button for their pre-written stories after reading only the first sentence of the ruling.) Thankfully I decided CNN simply had it wrong before I blast the news incorrectly to the HIStalk universe. Boy, Mr. H would have never let me live that down. 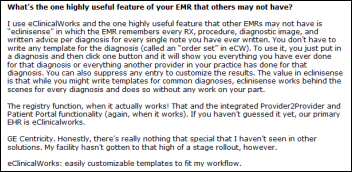






















































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…