Monday Morning Update 12/17/12
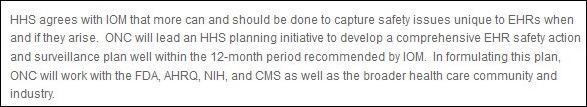
From John: “Re: ONC. What happened to its announced intention to publish an EHR safety action and surveillance plan? It was announced in November 2011 and was supposed to be finished within 12 months.”
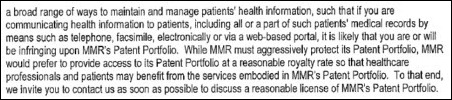
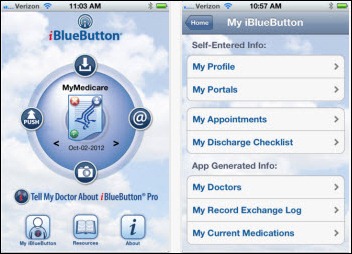
From California Dreamin’: “Re: MMRGlobal’s patent trolling lawsuits for patient portals. I hear ONC and the California Attorney General are interested in the company’s reason for e-mailing individual hospitals about its patents. The company seems to be going after hospitals rather than vendors for patent infringement.” The former is unverified, while the latter does seem to be the case as the company’s lawyers cast the net wide, apparently including just about every hospital as a potential patent violator.
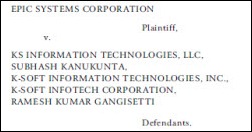
From Former Allscripts Employee: “Re: HHC lawsuit. I know for a fact that Glen and many others at Allscripts (as well as many outside of the company) are convinced that Epic is fleecing its customers. They feel Epic’s costs – especially the undisclosed long-term costs of operation – are outrageous and are hurting healthcare. As a former employee who participated in many C-level conversations, I’m guessing that they hope to use the lawsuit to bring those costs to light through the discovery process. Moreover, Allscripts has in fact demonstrated the integration of its ambulatory and inpatient EHRs at least one live site. And I’m sure they feel HHC could benefit from connectivity to Allscripts systems currently in place at Columbia, NewYork-Presbyterian, Memorial Sloan-Kettering, North Shore Long Island, and other NYC-based health systems serving millions of local patients whose records would be helpful to HHC providers. So while I agree it’s a dumb PR move for Allscripts, it’s not necessarily a bad business decision.”
Speaking of the Allscripts lawsuit, the company sent over this statement in response to Friday’s HIStalk write-up:
Allscripts filed the lawsuit because NYCHHC failed to even address, much less resolve, significant concerns that Allscripts’ raised in its agency-level protest concerning the propriety of HHC’s iCIS award decision. Documents produced by HHC indicate that the agency failed to follow the rules governing the competition and overlooked hundreds of millions of dollars in potential savings offered by Allscripts’ proposal. In these times, it is critical that public procurements be awarded through the conduct of fair competitions that objectively assess the merits of competing proposals and document a reasonable basis for the decision. From all available information, the HHC award to Epic is lacking in all of these respects. Allscripts’ product is currently being used by some of the most prestigious organizations in New York, we offered substantial cost savings over the life cycle of the project, and we committed to creating more than 100 new technology jobs in the City. Had proposals been evaluated properly, we believe that our offer was clearly the best value for the City. Our goal remains the same: We want transparency in the process… we want the bid process reopened so that the competing proposals can be reviewed fairly, consistently and side-by-side to ensure that the taxpayers of NYC obtain the best value Electronic Health Record solution.
I made a new Spotify playlist with old and new cool stuff from The Cult, Superchunk, Guided By Voices, Grizzly Bear, and others. It’s a work in progress since I may add more as I keep listening.
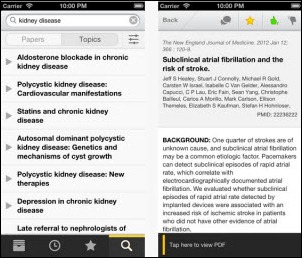
QxMD releases its free medical literature app, which allows browsing through topic reviews, reading journals, searching PubMed, and sharing articles via social media.
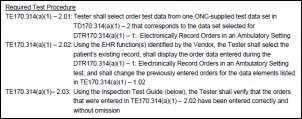
ONC announces the release of the 2014 Edition Test Method for EHR Certification.
In England, a government spending watchdog considers a review of the Department of Health’s payout to CSC for terminating its sole provider status as NPfIT was being dismantled. The Department of Health has said its ongoing support payments to CSC are funding centralized support, which critics say gives CSC a competitive advantage. Cerner has already raised concerns.
Baylor Health Care System announces that it will merge with Scott & White Healthcare, creating the largest not-for-profit health system in Texas with 34,000 employees, 42 hospitals, 4,000 physicians, and $8 billion in annual revenue. They created Vision for Texas Care site to explain the rationale.

NextGen Healthcare over sent an explanation of Michael Lovett’s new role mentioned in Friday’s post: “Michael Lovett is the senior vice president and ambulatory division manager for NextGen Healthcare. This is a newly-created role and Michael is responsible for developing and implementing the division’s strategic plan and ensuring that this plan is aligned with the company’s strategic direction.”
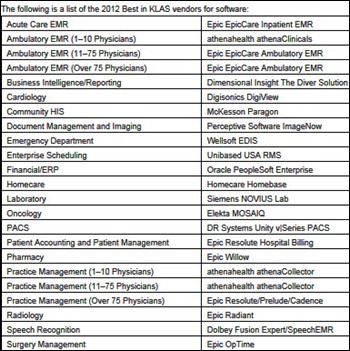
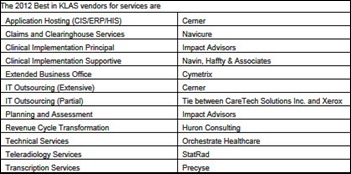
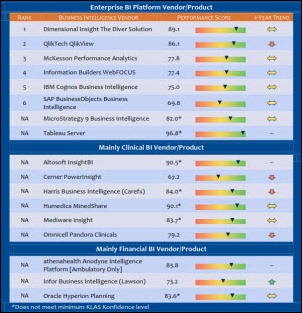
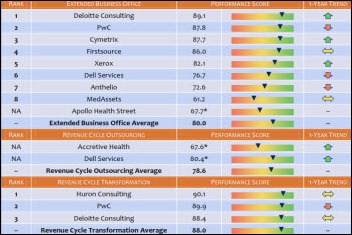
Just in case you missed Inga’s Friday morning post, here are the Best in KLAS winners for 2012. Notable factoids from it: (a) it was not surprising that Epic was by far the highest-ranked product suite, but McKesson Paragon beat Cerner to come in at #2, while the usual other big-hospital contender Allscripts finished next to last at #8; (b) McKesson came in last in physician practice rankings, with Cerner, Vitera, and Allscripts rounding out positions 7 through 9 ahead of it; (c) in the all-important inpatient EMR category, nobody’s even close to Epic, while Allscripts and Meditech populate the bottom; (d) Siemens Soarian takes the #1 spot for community EMR, although Prognosis, Meditech C/S, and RazorInsights had similar scores but were excluded because of confidence levels or because that’s not their primary market; (e) Epic is easier to beat in departmental systems, where it lagged other vendors in ED, scheduling, and anesthesia. The top three vendors overall were Epic, Wolters Kluwer, and 3M, while the bottom three were Agfa, McKesson, and Allscripts.
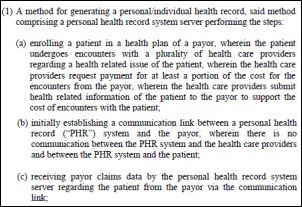
HealthTrio files a patent infringement lawsuit against Aetna and its ActiveHealth Management and Medicity subsidiaries, claiming that its patient portal patents have been violated.
Healthland will make the FollowMyHealth Universal Record Solution from Jardogs available to customers of its patient engagement portal.
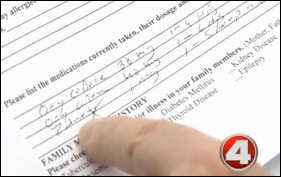
A jury returns a $140 million medical judgment against an Alabama hospital following the 2008 death of one of its patients by insulin overdose. The patient’s physician had dictated the results of his medication reconciliation, and since his original paper form was being scanned, the offshore-prepared transcription was used by a nurse as an order. The patient was given 80 units of Levemir insulin — 10 times the prescribed dose — and died. Testimony in the trial indicated that India-based transcription companies like the ones involved follow more lax standards. Precyse Solutions, the American company to which the hospital had contracted its transcription services, claimed that its Indian subcontractors follow American error standards, but deposed officials from those companies testified that they do not. The defendant’s attorney said the mistake should never have happened because the nurse should not have used the unreviewed transcription document to create an order. He also says hospital employees and physicians did not know that transcription work wasn’t being performed in-house, adding that the hospital’s executives did not know even the names of the Indian companies until the deposition. Those companies had previously settled with the plaintiff.
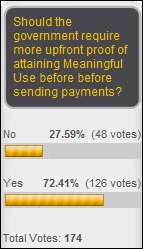
Conservative commentator Michelle Malkin calls HITECH a "big fat bust," saying it is not adequately supervised, it has created cronyism, and it has negative effects on job creation and privacy. There’s not a single original thought in the entire piece, as it was obviously just assembled from readily available Internet content. It claims that Epic "lobbied loudest for the mandates" as one of the dated "hard-drive dependent software firms." She also makes the classic but nearly unforgivable mistake of editorializing loudly about providers who are fraudulently receiving payments for using EMRs they already owned, apparently unaware that HITECH was written precisely to encourage that practice. Unlike Cash for Clunkers, EMR drivers get paid for driving their same old cars.
An article in Iowa newspaper says that the i-PHACTS system developed by the state’s Department of Public Health in 2010 to track available hospital beds is nearly useless for placing patients because it’s only updated daily. A medical student is creating his own version, but it has the same limitation — integration with hospital systems is complex and hospitals aren’t willing to manually update their information on unoccupied beds regularly.
A North Carolina business paper profiles Greensboro-based Intellect Resources, which it says has quadrupled sales in each of the last two years as it provided consulting and recruiting services for hospitals implementing electronic medical records.
Health Management Associates, the subject of a "60 Minutes" report claiming its hospitals admitted patients needlessly, says the program’s sources were disgruntled former employees, one of them a physician who used court-sealed information provided to him by the program to amend his lawsuit afterward. The doctor changed his 2010 lawsuit when he saw sealed details claiming that the company’s ED software was being used to increase admissions, adding that claim to his own already-filed suit. HMA says its ED doctors don’t make admission decisions and they’ve stopped using the software.
An armed visitor shoots a police officer and two employees of St. Vincent’s Hospital (AL) on a nursing floor at 4:00 a.m. Saturday. Their injuries are not life-threatening. The suspect was shot dead by a second police officer.
Medicare’s $77 million fraud detection system, widely panned after audits found it had prevented only around $8,000 in fraudulent claims, is now claimed by CMS to have saved $115 million, although the report does not indicate how many providers were suspended from Medicare as a result. The report also indicates that the actual savings was $32 million, with the higher total being claimed as the future value of fraud that would have happened otherwise.
Health management and analytics systems vendor Medecision will lay off 83 employees in Wayne, PA headquarters, according to WARN act documents filed with the state. The company says those affected work in software development, program management, and technical support.
Weird News Andy is tickled by this story, which he snickeringly subtitles, “Little Angel.” Doctors eventually figure out what’s causing the swollen jaw of a seven-month-old girl: a two-inch feather embedded in her cheek.
Communications. Combine the following medical, cultural, and technical TLAs and FLAs into a meaningful sentence. You may use one pronoun, one verb, two prepositional modifiers, and a gerund. Ex: IMHO, CMIO NCQA PCMH FAQs without LOINC, HL-7, or SNOMED FYIs were DOA and SOL. SNAFU.
PS: if you know all these, you do not need to complete the rest of the test.
- SQL, LOS, CMS, PDQ, CDS, MSSP, MRSA, TIN, RAC
- HTML5, CVA, TJC, CFO, FYI, CXO, EDW, HIE, AKA
- CPOE, CTO, SOL, HIPAA, ACO, TIA, IMHO, GOMER
- PERL, TWAIN, ACA, VTE, PHR, CAPTCHA, POS, POC
Patient management. Who will have the most useful problem list?
- Five different hospitalists, NPs, and nurses using a combination of ICD9/10, SNOMED, and homegrown synonyms, with no one in charge
- A 70-year-old GP using free text
- Surgeon – two items for 84-year-old ICU patient
- Neonatologist — 27 SNOMED items for a three-day-old
- Patient’s PHR
Training. Which of the following techniques works least badly?
- Day-old pizza and handouts in the lunch room
- Department meetings at 7 a.m. on a Monday
- E-mails from people no one has heard of
- At-elbow support by people who just heard about the project yesterday
Leadership. You have 15 hospitals over four states. Which model of leadership works best?
- Central (disconnected, jet lagged, and intermittent)
- Local (random, quirky, and adversarial)
- Democratic (but only certain people can vote)
- A CMIO with no direct reports, graded on “influence”
Fill in the correct phrase or words.
- CFO is to Budget as Sphincter is to __________.
- Twitter is to Communications as Static is to ____________.
- Regulation is to Efficiency as Friction is to ____________.
- ACO is to HMO as Deja vu is to ___________.
Order management. You are leading a CPOE installation and want to use the latest evidence-based guidelines. What is the right approach?
- Call a meeting of department leads, take two years, then make them up yourself
- Use third-party content, send to department leads, wait six months, then make them up yourself
- Use your paper-based content and sneak in the latest content with the one guy who comes to your meetings (i.e., make them up yourself)
Support. You are stopped in the hall and asked to design a new system that will save this physician maybe 2 –3 clicks a week, but will take your team at least two months of design, development and testing, two more months of training the entire staff, along with disrupting everyone else’s workflow. What is your response?
- Ask them to send you an e-mail describing the effort, knowing that they are “too busy” to get around to it
- There is no other correct answer
Software selection. You have been asked to select a new EMR for your 200-bed hospital. What are the first steps you should take?
- Change your bed number to 500 so Epic will talk to you
- Watch the Cerner salespeople twitch when you ask one of them to demo the entire “standard implementation”
- Read KLAS, develop detailed requirements, do reference visits, then cave in to the most powerful docs (that couldn’t be bothered to come to demos) because they heard that System X was hard to use
- Go to HIMSS for wine and dine, then play spin-the-pocketbook and pray you get the “mature” implementation team promised by a sales guy you will never see again
Statistics. Which of the following principles are true?
- Pareto principle – 20 percent of the producers will make 80 percent of the product, but they will not be paid like it
- Death panel principle – 5 percent of the population consumes 50 percent of the costs, but you can’t do anything about it
- Incentive principle — the other 80 percent (see Pareto) will spend more energy gaming the system than producing
- Software development principle – 3 percent of the use cases will drive 80 percent of the timeline delays
Meetings. As CMIO, you are invited to a 2.5 hour mandatory budget meeting. What is your response?
- Attend with iPhone and iPad charged and catch up on e-mail
- Dial in while getting work done from your office, knowing that the CFO’s secretary will not be able to figure out the teleconference link
- Attend, listen closely, and wait for the moment when a physician’s fiscal wisdom will be most appreciated
- CMIOs do not get invited to budget meetings, and if they do, that is when you use the spam filter excuse.
Alerts. What is the most effective method of providing meaningful alerts to busy clinicians?
- Goldilocks – community-based balanced approach that will still get you eaten by the bears, and the “ community” will be nowhere around
- Overalerting — as determined by docs who just want to know when they are definitely going to kill someone
- Underalerting — as determined by your legal representation
- Individually tuned for relevancy, with actionable orders easily accessible within the order, highlighting only important info that you didn’t know and makes a difference in this unique patient (available in the next release)
- Horror stories in the physician’s lounge
User interface. Which of the following is the most effective modality for communicating key clinical information?
- A 24-inch LCD monitor with 5,347 elements in three-column view, vertical scrolling, and 23 colors
- An iPhone with no information on the top screen, but multiple branching links which will eventually lead you to YouTube
- An angry nurse that you have not returned pages to for over an hour
- An intern whose pre-med major was theatre arts
13. Pa55Words. Which of the following is optimal policy?
- Same password for all your applications “HckerPLsDoEmails2OK?”
- Four factor – iris scan, voice profile, 10-character randomly generated password changed every three months, with RFID embedded chip, Comrade
- Three strikes, you get pepper spray
- Prefilled sticky notes attached when shipping monitors
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.













































... because it's a construction worksite. (It's a bit more evident from the second photo in the linked post.)