Ben Albert is founder and CEO of Care Team Connect of Evanston, IL.

Tell me about yourself and the company.
The company started officially in late 2008, but I took it on full time in early 2009. Prior to starting Care Team Connect, I worked in healthcare technology for my whole career, most recently in a services company, PatientKeeper, for the acute care setting, where we were pulling together data for hospitalists and the providers within the hospital to better coordinate and manage care within the hospital.
As a result of that and parallel to that, my grandfather had his second stroke. Seeing all the effort that was going into the inpatient setting and very little effort going into the community setting compelled me to start the company to better coordinate care in the community for high-risk patients.
Describe how care coordination should work ideally.
There’s a number of perspectives on that. In my opinion, the way care coordination should work is that patients should get a patient specific plan of care that encompasses all people who touch that patient so they’re singing off the same sheet of music. Making sure it considers psychosocial factors, patient history and patient risk, and the whole patient as the plan is assembled, so that everybody knows who is going to do what when for each patient. That will enable efficiency, lower costs, and higher quality.
What needs to happen to make the patient-specific plan of care ubiquitous, like medication reconciliation?
You need to have the right team in place in order to manage and coordinate a population’s care. While our technology will streamline it and allow you to do a tremendous amount more with the resources that you have than if you don’t have a platform like ours to power workflow and coordinate care, if you don’t have the people who are focused on it — and I mean truly focused on it, not tangentially focused on it — as soon as you determine that you need to establish a team that’s responsible for coordination, then you need to power that workflow and allow it to scale.
Where we see most of the initiatives fail is that people will make that decision, but then they won’t be able to get lift or scale around the population, because they end up managing just the highest of high-risk patients with a few part-time or full-time resources. That in itself isn’t a way to enable full, broad-scale care coordination.
You need a more systemic process around how you are going to manage the high-risk, moderate-risk, and low-risk patients. What things are you going to do specifically for each patient as they impact quality and cost? Then allow yourself to scale that through automated processes like our technology. But before you even get to technology, you need to talk about your program development and how you can scale, which we also help our clients with.
How does your platform support that process?
The platform listens for data that would trigger action on a patient that’s being managed in a population. Truly managed, not any patient in the population. We’ll identify which patients need to be managed. We’ll reconcile actionable data, which could be a real-time admission alert from an ADT, it could be a new medication, it could be a change in a patient’s psychosocial status like a change in home setting.
Any number of these things can be a triggerable event in our system that would drive action. The system listens for that, weights it against the patient-specific information and the risk to the patient and the care program that that person sits in, i.e. what we need to do in the event this piece of data comes in for this particular patient at this risk?
It drives the specific tasks to the right people across the continuum. When I say that, I mean those right people can be a family member, a clinician, a nurse, and anybody who has a relationship to that patient. The system’s rule will tell you, OK, based on this patient, here’s where you fire this task to.
What integration is required?
The most common integrations we do are to either claims or attribution models from payers or a shared savings program or ACOs or however they have their attribution models in their claims from the payers. We’ll pull that in as the foundation for the population being managed. Then we’ll marry real-time data to that on the fly, which includes ADT, medication feeds, and visits to the physician office. Those types of pieces of data are real time, married to the attribution and patient-specific data.
It can be labs. It can be any number of data elements that will trigger action. Based on the population being managed, we build these programs and actionable events around the data that’s more pertinent to the population being cared for.
How would a typical customer connect to that data and what are they doing with the results?
I’ll walk you through a couple of customer scenarios. We work with medical homes, ACOs, health systems, and we’re starting to get into some more of the employee health types of things. In the ACO medical home scenario, we’ll take a client who is currently managing 120,000 lives across an entire state with 77 physician practices. They need to manage that care across all those lives, across all those demographics.
They take their attribution, and then they take some real-time ADT information from various places across the state, and the plan of care that’s been established for each of the patients based on their criteria. They marry that specific data, i.e. an admission for anyone in their 120,000-patient population will trigger a workflow for the care managers or care navigators supporting that population. That’s a very basic core workflow that prevents readmission, increases coordinated care, and truly establishes a workflow around it, a transitions of care workflow in particular. That’s one example.
Another example might be a pure preventable readmissions initiative with a specific client, who upon discharge, we receive just ADT information along with some other data to identify which patients are at risk of readmission. From there, we’ll drive a particular plan of care based on what type of patient it is, what type of follow-up needs to occur, and drive the tasks and the actionable plan around that in an automated fashion.
If I go back to that first scenario for a second, I failed to talk about one core piece of data that is a differentiator. The population health analytics companies who today are doing a great job of identifying gaps in care and managing the data around the population that also in case of truly managing the health of a population, that data is valuable in addition to the real-time data, in addition to the attribution to trigger the right plans of care based on the patient’s attribution, risk, gaps, and beyond.
Many companies are involved in analytics and population health management. How do you see your offering fitting and who do you consider to be your competitors?
In the population health analytics space, we look at their data as great triggerable events married to all the other things we’re doing with the population. We like to work closely with them, especially if our clients decide to go in that direction and feel the need is strong enough for their population to identify gaps and do that analytics.
We really don’t feel like we’re competitors to the analytics companies. It’s more as a partner, where we can leverage their data to truly drive workflow and action, which seems to be a pretty big gap in the market right now that we’re filling.
Is it difficult for people to understand what you’re offering and how it fits in?
It can be, until the market understands the difference between care coordination and care management and population analytics, which we’re charged with helping the market understand. There’s a huge difference. It can get gray in terms of the client’s perception of what we do versus what those solutions provide.
But as soon as a client really digs in and says, OK, how are we actually going to manage the population? Not how are we going stratify and identify the population, but how are we actually going to manage the population and all of these care coordinators we’re hiring now? How are we going to power their workflow in a way that we’re sure that they are going to follow the right patients and that we’re going to get the yield out of the initiative that we anticipated getting?
It’s the next step. People recognize that as a major need. We sit on front of it to make it all happen. But until there is that understanding of what analytics is really built around — and it’s really built around crunching the data and what we do, which is built around workflow and coordinated care — I think the market does get confused until they understand the difference.
It sounds so obvious that there should be a patient-specific plan of care. Describe how it gets created and maintained and what the end result looks like.
It is somewhat of a new concept in the way in which we approach it, but I think there had been a lot of folks after the longitudinal plan of care for a patient. They are often templated and disease based, much as disease management companies or groups like that have approached the market in the past.
What we do is much different. There are elements of disease-based plans of care, but it’s really about the patient themselves, the psychosocial data, meaning what is their mental health, what is their home status? A number of those other elements which can help dictate how to follow up and manage that patient. Essentially, how much do I need to do to support this patient as opposed to how much can they do on their own without my involvement?
Our approach takes that data, which changes over time, and marries it to the real-time data. The plan is always changing. It’s a living, breathing plan of tasks and documentation to support that patient. As data changes from a real-time perspective and there is a profile change for a patient, the plan morphs along with the patient to make sure that it’s always providing the right level of support and efficiency around that patient’s care as required.
That’s really a big difference for us. It’s by no mean a single-threaded plan of care. This is a living, breathing plan of care based on the data coming in to the system and the patient’s needs, which really hadn’t been done before, not in this way, anyways.
It seems to be getting a lot of traction in the marketplace as a result, because our clients don’t have all the resources in the world and that’s not going to change. How are you going to truly manage this population of patients and help our community members who are collaborating with you in this ACO or in this shared risk initiative to support the population in real time? That’s how we help it happen.
A typical example would be where there is a primary care provider and a hospital relationship that integrates specialists and therapies. They’re potentially with an admission or an ED visit and there might be a specialist involved and there might be therapies of some sort. The resulting plan integrates all that into a single single source of truth that everybody agrees and understands that is taking care of that patient.
Absolutely. You’ve got it. That plan is driven by the individual or group that is responsible for the population. The ACO group may create that source of truth through our platform, or the hospital. It really depends on where is the risk is. They’ll drive that plan based on the automated routines.
The new brave new world of ACOs has put together some bedfellows that may not be comfortable with each other, as in hospitals and practices.
You can add the health plans into that mix as well, in terms of all the groups who are participating in these initiatives and how well they work together in a way that makes sense for everybody.
I suppose the answer to you is that’s initiative by initiative, community by community. In some cases, like in Battle Creek where we are working, everybody is collaborating really well. It’s actually the practices who are leading the initiative, supported by the health systems and other folks in the community organizations and the community.
In the hospital-driven initiatives, it can be very effective. For example, we’re working with a health system in the Northeast. They are powering all their skilled nursing facilities through our platform. Upon discharge, one of the skilled nursing partners will get all their detailed plans for a heart failure patient that’s being discharged to them. Not in the placement type of variety, which I know is probably the next question, but more on, what’s the plan of care for this patient?
Those people are engaging and wanting that type of information because they aren’t armed with that data in a way that makes them successful. They want that type of collaboration. They know in the future it’s all going to be shared, and if they are not lining up to collaborate well with the health system today, it’s going to be a big problem for them in the future.
Everybody thinks about physicians and hospitals when they think about care coordination or ACOs, but in this model that you’re describing, it sounds like there is an important role for a nurse.
A huge role for a nurse and family and community partner. If you fall in to the trap of this is only a physician-led or hospital-led initiative, you’re not going to change things the way that they need to be changed in order to really coordinate care.
You need to infiltrate that with a care navigator-type nurse function that supports the population and also understands what it means to truly work with community members, Meals on Wheels, various partners in the community, family members, adult caregivers. All these people who can play a role for you.
I’ve got all this work to do for this population. I know I need to do to support the population well. I have a handful of resources to make it happen. There are community resources out there willing to do this and they just need to be armed and ready to go. If you put that process in right, you are actually solving a much bigger problem by truly supporting the community and the population as a whole.
Where do you see that company being in five years?
That’s a great question. I get it often. The way I answer that is, I’m not sure where the company will be in five years. We just keep delivering value week to week, month to month, year to year basis, and keep listening to what our clients are telling us. Making sure we understand where the market is going and keep driving and building a successful organization that has value and purpose.
We try very hard not to focus on our five-year plan, but to focus on execution, action, value, and purpose as an organization. The rest will take care of itself.
Any final thoughts?
The company is doing tremendously well. I’m sure this is consistent with what everybody says, but the company is truly doing great. We recently signed our largest client to date. I think Care Team Connect is very, very well positioned for the foreseeable future. We’re just excited to continue to read your blog and hopefully show up there more and more with good news.

















































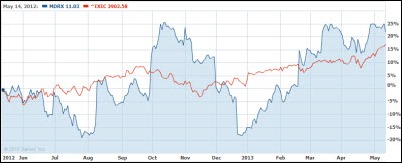























I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…