Readers Write 5/21/12
Submit your article of up to 500 words in length, subject to editing for clarity and brevity (please note: I run only original articles that have not appeared on any Web site or in any publication and I can’t use anything that looks like a commercial pitch). I’ll use a phony name for you unless you tell me otherwise. Thanks for sharing!
The Art of Medicine: Unlocking the Power of Patient Data
By Nick van Terheyden, MD
We are awash with information and choices in every aspect of our lives, from the selection of our morning coffee to the choice of painkiller in our local pharmacy. Worth noting, Starbucks currently offers 30 variations of espresso beverages, and each comes in three sizes with four types of milk. That’s 360 choices — enough to potentially make you want to not get out of bed in the morning.
This problem is magnified in medicine with a deluge of new information, studies, treatments, and the explosion of genome understanding and its impact on patient care. Based on current estimates, medical information is doubling at least every five years. Cyril Chanter encapsulated today’s medical information challenges best when he said, “Medicine used to be simple, ineffective, and relatively safe. Now it is complex, effective, and potentially dangerous.”
There is general agreement in the medical profession that the delivery of quality medical care is no longer possible based on recall and applying what individuals can remember at the point of care. In fact, according to the Kaiser Permanente Institute for Health Policy, “Current medical practice relies heavily on the unaided mind to recall a great amount of detailed knowledge – a process which, to the detriment of all stakeholders, has repeatedly been shown unreliable.”
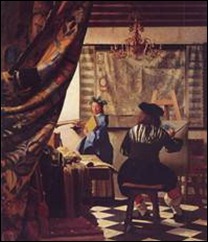
The digitization of medical records, accompanied by the requirement imposed on the care team to capture discrete data, is setting the healthcare system up for failure. We’re promoting the incomplete capture of the patient note. Discrete data is much like a black-and-white drawing — it contains some of the data, but much of the critical information and nuances are missing. In order to ensure the complete capture of the patient note, discrete data and the clinical narrative must coexist.
The key transport mechanism for medical intelligence is the clinical narrative, which provides the detail that is essential for the execution of intelligent, high-quality medical care. From there, language understanding offers a legend for these pieces of information – the narrative and discrete data – which allows us to view the complete work of art, also known as the patient note.
We are a long way down the path to enabling clinicians to capture complete patient information using the latest advances in voice recognition, which converts spoken word into text. Still, it is with language understanding that we unlock the true meaning of this information, offering a “Rosetta Stone” to tap into the insights of this information and allowing us to connect the dots in our expanding picture of patient care in a digital world.
It is this unlocked data that will link the subtle details of the patient record to vast mountains of medical intelligence; allowing for a guided, evidence-based approach to medicine alongside integrated decision support. This in turn will offer care takers a more complete picture from which they can guide individual care, while enabling possibilities surrounding large health population analysis and insight.
As we unlock the capabilities of clinical data in healthcare, we open the door to new discoveries, associations, and yet-unimagined treatments that will directly affect the care of those we love and look after now and into the future.
Nick van Terheyden MD is chief medical information officer of Nuance of Burlington, MA.
Stop Thinking “Universal Remote” and Put Patient Care On Demand
By Mary Baum
I once heard it said that successful device connectivity in a hospital is like implementing a universal remote on your TV. The consolidation of controls allows for easier training of new users, fewer steps to execute a command, and less room for error. But in today’s age of accountable care and new care delivery models, the health systems that are still operating in the “universal remote” mindset will be left behind as the industry progresses.
It’s great that my DVD player can talk to my TV. But what about when I want to watch the same movie on my laptop in the other room? And while this entertainment glitch is a little frustrating, it’s actually criminal when we think of a similar scenario in the healthcare world. We don’t need to just connect one point solution to another. We need to be able to effectively care for patients, regardless of where they are within the hospital; what systems the hospital has in place; or how many physicians, nurses or other staff are involved in the patient’s care. The sooner hospitals begin to think beyond individual technologies and develop an overarching strategy to connect people and processes, the faster we’ll start to see a real change in patient care.
Historically, hospitals and health systems have approached medical device connectivity tactically, focusing on how to connect a nurse call device to a smart phone, a monitoring device to an iPad, or data from a smart bed to an EMR. Often purchased by IT departments as middleware, a range of IT solutions have been viewed as a solution to one or two key problems, and have typically been implemented one department or one facility at a time.
Because many of these technology investments were made to solve only singular, point-in-time problems, providers still struggle to deliver care that focuses on the patient across the entire care continuum. They need to get smart about implementing solutions that cater to the unique workflow of their personnel – not their hardware – if they want to drive efficiency and improved patient care.
It’s not really the provider’s fault, though. The vast majority of vendors have played into this universal remote mindset by building point solutions that connect a small subset of devices or departmental systems to one another, rather than focusing on the entire system. Providers need solutions that both cater to a department’s unique workflow and enable collaboration from one department to the next, making it possible to efficiently serve patients as they move between these diverse care settings. They need to come to the table with customizable solutions, and with services that help hospitals implement these solutions as part of a broader workflow strategy. It’s not enough to drop off a box and wish them well. Providers need partners to help them learn and improve for years to come.
We need a new movement in healthcare, one that takes a system-wide view to clinical workflow design and leverages clinical technology solutions to both connect devices and foster collaboration across the entire system. This includes everyone from patients to clinical teams to ancillary groups (biomedical engineering, dietary, environmental services, IT, and pharmacy). Clinical workflow is about more than hardware and software. It’s about the clinicians who use these solutions and need them to promote — not hinder – high-quality patient care. Vendors need to offer their customers something better than stale point solutions.
As an industry, we need to map to the bigger picture, driving teamwork and collaboration among every individual and across the entire care continuum in order to drive dramatic performance improvements for healthcare organizations.
Mary Baum is chief healthcare officer of Connexall USA of Boulder, CO.
The Long Road Ahead: Choose your Traveling Companions Wisely
By Chad Morrill
When hospitals choose a healthcare IT provider, they too often just focus on the same questions many of us consider when buying a car: “How fast does it go?” and “How much does it cost?” But for a successful project, these are just two of the many factors to consider. Another key decision point should be a vendor’s suitability as a long-term partner.
We’re not just talking the equivalent of a 100,000-mile power train warranty, whereby the vendor will fix your system if it breaks, though of course responsive support is important. But beyond that, you’ll be better off working with a company that not only understands its products and services, but also your processes, your staff, and your goals, and will do its best to unite these elements to give you maximum performance and value.
The first thing to consider before getting on the road is your hospital’s needs, both now and for the next few years. What are the pain points you’re trying to overcome, what new compliance mandate are you struggling to satisfy, or which facet of your EMR/EHR project are you finding most troublesome? This then defines the focus of your solution search, which will in turn narrow your list of prospective vendors.
Next, ask for references from facilities like yours and see how they’re solving the very issues you want to solve. Then ask them what else they’ve been able to do with the product. A hospital sometimes picks a solution because it fits neatly into whatever box they’re trying to fill, but yet leaves the full potential of that solution untapped. One of the reasons is that an IT team is typically tasked with solving a very narrow problem, and once they’ve done it, they must move on to putting out the next fire lit by clinicians or the CIO. They then go out and look for other vendors to meet the very needs that could be met by the product they’re already using – a waste of time, effort, and money for everyone involved.
Executives tend to chase the next “shiny object” or respond to the newest tech trend, and this leads to the misconception that something ‘new and improved’ is required. Just like we all want the next iPhone or iPad, many hospital users hanker after the latest IT toys on the market, following the hype rather than putting in the effort to explore the full capability of the applications already deployed.
Despite the need for hospital project managers to be proactive in working with vendors to get the most from their systems, the burden cannot fall solely on the facility. A responsible vendor that cares about its customers and the staff and patients they serve should dedicate time and resources to helping hospitals get the most out of its solutions. A regular onsite “checkup” with both a customer advocate and a member of the vendor’s executive team can provide the hospital with a view of what its products can do now, and what the roadmap is for upcoming functionality. The vendor can explain and even demonstrate how other customers are using its offerings in new ways, and can then help the IT staff put this knowledge into action. Executive buy-in is also crucial on the hospital side, as the CIO and IT director will be key in both understanding the full potential of vendors’ products and services, and then in driving widespread user education and adoption.
The challenge to such leaders: push your IT analysts/project managers to explore each product’s entire feature set and get involved in engaging your vendors to see what else you could or should be doing. Yes, it requires accountability and an upfront time investment. But it will yield the benefits of doing more with existing tools, moving further toward achieving your facility’s goals, and, most importantly, of improving care and service to your patients. Time to start your engine!
Chad Morrill is an account manager at Access of Sulphur Springs, TX.







Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…